Published online Aug 26, 2021. doi: 10.4330/wjc.v13.i8.348
Peer-review started: January 28, 2021
First decision: May 6, 2021
Revised: May 13, 2021
Accepted: July 20, 2021
Article in press: July 20, 2021
Published online: August 26, 2021
Processing time: 207 Days and 5.4 Hours
Coronary artery bypass grafting is a surgical treatment for ischemic heart disease. Although development in surgical technique and improvement of perioperative management reduced the postoperative complications, some patients still delayed in progress of postoperative rehabilitation. In this study, we aimed to investigate the effect of daily intake of an herbal medicine-containing drink for rehabilitation after surgery in patients with ischemic heart disease.
To investigate the effect of taking an herbal medicine-containing, commercially available drink for postoperative rehabilitation in those patients.
Patients who underwent isolated off-pump coronary artery bypass (OPCAB) surgery were divided into two groups depend on the timing of the admission to the hospital: the Yunker (YKR) group, that consumed one bottle of a caffeine-free nutritional supplement drink on a daily basis and the control group (CTL) that underwent regular rehabilitation.
A total of 229 patients (CTL = 130, YKR = 99) were enrolled. No significant differences were observed in the baseline characteristics between the two groups. The YKR group had a significantly increased number of daily steps postoperatively (P < 0.05) and had significantly lower postoperative serum tumor necrosis factor-alpha levels (P < 0.01), while no significant differences were observed in the levels of other inflammatory or stress-related cytokines (interleukin-6, adiponectin, superoxide dismutase, and urine 8-hydroxy-2′-deoxyguanosine) between the two groups. Also, the YKR group showed a significant improvement in the Hospital Anxiety and Depression Score (P < 0.05). Moreover, there were no differences in postoperative complications and the duration of postoperative hospital stay between the two groups.
Our results demonstrated that the daily intake of an herbal medicine-containing drink after OPCAB surgery may have beneficial effects on cardiac rehabilitation by reducing inflammation markers and depression.
Core Tip: Ischemic heart disease is still a major cause of death in the developed country. Cardiac rehabilitation for the patients who underwent coronary artery bypass grafting surgery has known to be associated with early recover. Daily intake of an herbal medicine-containing drink after the surgery enhances the postoperative cardiac rehabilitation by reducing inflammation and improving depression.
- Citation: Matsushita S, Shimada A, Yamamoto T, Minematsu K, Inaba H, Kuwaki K, Amano A. Nutritional supplement drink reduces inflammation and postoperative depression in patients after off-pump coronary artery bypass surgery. World J Cardiol 2021; 13(8): 348-360
- URL: https://www.wjgnet.com/1949-8462/full/v13/i8/348.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i8.348
Ischemic heart disease is still a major cause of death in the developed country. Coronary artery bypass grafting (CABG) is a surgical treatment for ischemic heart disease. Although postoperative complications are reduced with the technical development of the surgery, such as the off-pump technique[1,2], or with the improvement of perioperative management, variable amounts of physical and mental stress still occur after surgery. Postoperative rehabilitation following cardiac surgery is highly recommended since it increases motion tolerability[3,4], improves cardiac function[5,6], and reduces postoperative depression[7,8]. The recent guideline recommended the early induction of postoperative rehabilitation for the prevention of perioperative heart or respiratory failure, resulting in short hospital stay and early social recovery[9]. Despite the abovementioned recommendation, patients with low cardiac function, high age, frail, or complicated conditions often show delay. With the recent increase in the elderly population, the number of octogenarians who underwent CABG has also increased. These patients are potentially frail and exhibit systemic deterioration.
Consuming a commercially available nutritional supplement “energy” drink when a person experiences fatigue or develops illnesses such a cold is a widely accepted practice in the Japanese society. Some people habitually consume this type of drink as a treatment for chronic fatigue or to maintain motivation. Various kinds of nutritional supplement drinks are commercially available in Japan. Although, many of these products commonly contain multiple vitamins, caffeine, and sugar, only few contain herbal products, of which some have been known to reduce the physical and mental stresses. In this study, we aimed to investigate the effect of taking an herbal medicine-containing drink for postoperative rehabilitation in patients with ischemic heart disease.
Adult patients (≥ 20 years of age) who were scheduled for elective isolated off-pump coronary artery bypass (OPCAB) surgery at Juntendo University Hospital were enrolled consecutively in the study from January 2014 to December 2017. The patients were assigned to one of two groups as follows: Those enrolled from January to June 2014 and September 2016 to December 2017 were assigned to the control group (CTL), and those enrolled from June 2014 to September 2016 were assigned to the treatment group. Patients in the treatment group consumed 30-mL of a caffeine-free, herbal nutritional supplement from a commercially available bottle, (Yunker DCF, Sato Pharmacy. Co. Ltd, Tokyo, Japan) every day after being granted permission to resume a liquid diet following surgery (YKR group). Patients with liver dysfunction (defined by tests exceeding the normal value in any of the following markers at the time of administration: alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, or γ-glutamyl transpeptidase), who underwent hemodialysis due to kidney dysfunction, or who experienced preoperative gait disturbance were excluded from the study. The contents of the drink are shown in Table 1. Patients in the CTL underwent the regular post-cardiac surgery course and did not consume the supplement drink. Both groups were treated according to our post-CABG clinical path. In addition, patients who received concomitant surgery due to the surgeon’s decision during surgery and those who experienced stroke (including transient ischemic attack) or infections such as pneumonia postoperatively were excluded from the study.
| Contents | |
| Agkistrodon meat and bones tincture | 100 mg |
| Civet tincture | 250 mg |
| Ginseng fluid extract | 600 mg |
| Hawthorn flower extract | 30 mg |
| Rehmannia root extract | 120 mg |
| Royal jelly | 100 mg |
| Vitamin B1 nitrate | 10 mg |
| Vitamin B2 phosphate ester | 5 mg |
| Vitamin B6 | 10 mg |
| Tocopherol acetate | 10 mg |
| Nicotinamide | 25 mg |
| Panthenol | 10 mg |
| Chondroitin sulfate sodium | 120 mg |
The primary endpoint of the study was whether the YKR enhanced the activity postoperatively. To evaluate perioperative activity, we used an accelerometer (Omron HJA-350IT, Kyoto, Japan). As indices of the activity, the number of daily steps, daily total activity [metabolic equivalent (MET) × hour], and moderate-to-vigorous intensity physical activity (MVPA) were used. Total activity was determined by calculating the integrated METs per minute for 1 h (60 min), while MVPA was calculated using more than three METs of total activity.
The maximum value in each period (pre-/postoperative) was compared between the two groups. If preoperative or postoperative data were lacking, they were excluded from the activity analysis.
Results of blood tests performed upon admission and on the 2nd and 7th postoperative day (2 POD and 7 POD, respectively) were used in this study. In addition, the levels of the following inflammatory cytokines were measured in serum and urine (SRL, Inc., Tokyo, Japan) and compared between the two groups: interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), adiponectin, superoxide dismutase (SOD), and the ratio of urine 8-hydroxy-2’-deoxyguanosine and creatinine (8-OHdG/Cre).
Before and on 7 POD, the levels of depression and anxiety were assessed. We used the Hospital Anxiety and Depression Scale (HADS) and Geriatric Depression Scale-15 (GDS). The HADS has two subscales: HADS_A, used to measure the level of anxiety; and HADS_D, used to measure the degree of depression. Each value and changes in intra-patient values were compared between the groups.
The Kolmogorov-Smirnov test was used to assess the normality of data distribution, and further statistical analyses were subsequently performed. Patients’ baseline data were compared using the chi-square test and Student’s t-test. In the development data set, we formulated a predictive equation based on sex, age, body mass index, ischemic heart disease, treatment with cardiopulmonary bypass, hypertension, diabetes mellitus, dyslipidemia, preoperative hemodialysis, smoking (present/history), persistent atrial fibrillation (AF), serum brain natriuretic peptide level, New York Heart Association classification, left atrial diameter, and left ventricular ejection fraction. Multicollinearity among the variables in the predictive equation was considered. Data were analyzed using SPSS 22.0 (SPSS, Tokyo, Japan). All data are expressed as mean ± SE. Statistical significance was set at a level of P < 0.05. The statistical methods of this study were reviewed by an expert Biostatistician Dr. Minematsu K.
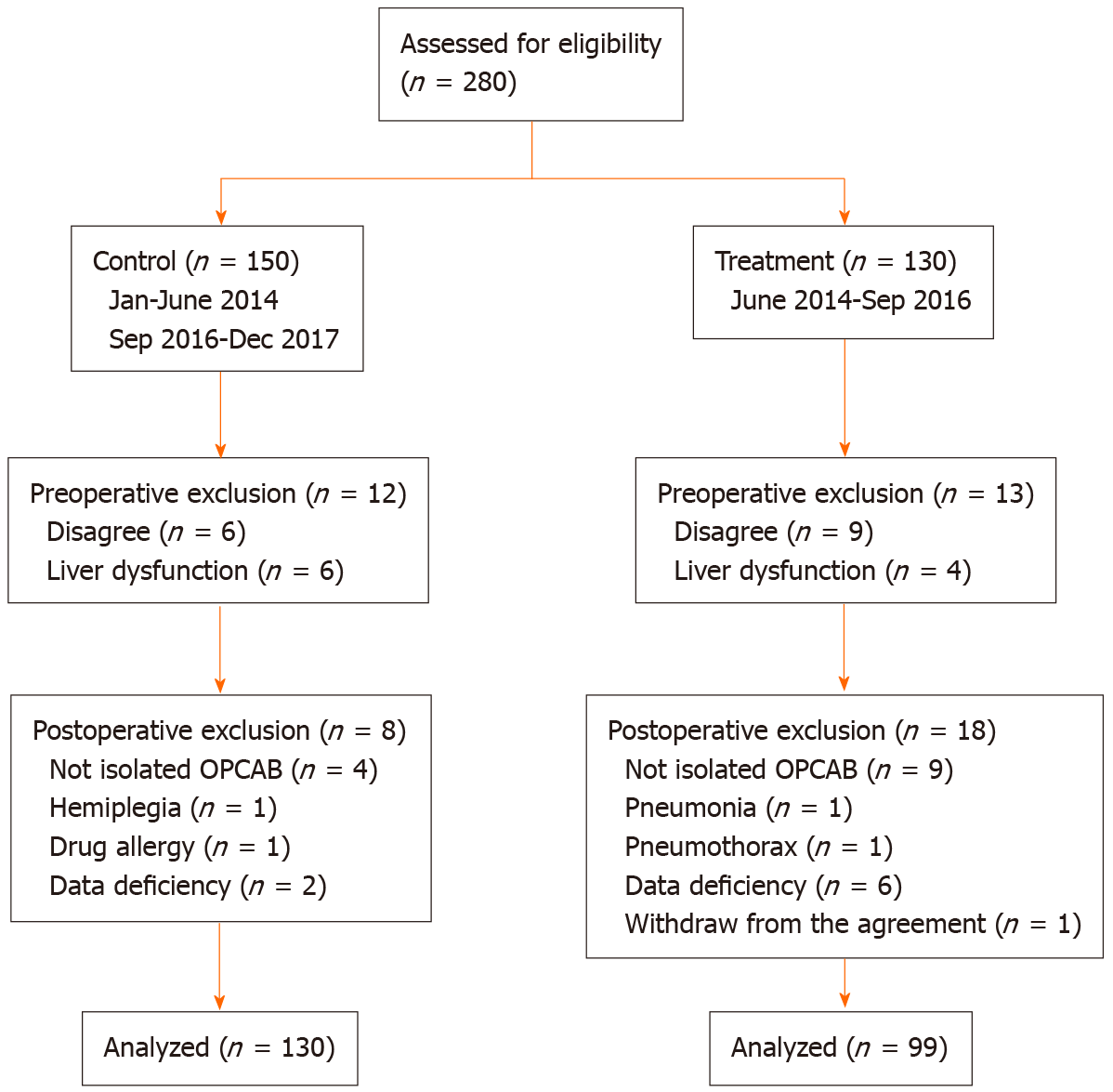
Altogether, 280 patients were eligible to enroll in this study (Figure 1). Fifteen patients did not consent for enrollment and 10 were excluded preoperatively because of liver dysfunction. Thirteen patients who were initially eligible did not undergo isolated OPCAB surgery due to their physician’s decision, one withdrew from the study, and four other patients were excluded because they developed hemiplegia of the right hand, postoperative pneumonia, pneumothorax, or a drug allergy. Furthermore, eight patients were excluded for missing data. In total, 229 patients were analyzed; 130 were in the CTL group and 99 were in the YKR group. The characteristics of the patients are shown in Table 2. There were no differences in these indices between the two groups.
| CTL | YKR | P value | |
| Number of patients | 130 | 99 | |
| Age, yr | 69.4 ± 0.8 | 68.5 ± 1.0 | 0.437 |
| Female (%) | 20 (15.4) | 12 (12.1) | 0.481 |
| BMI | 24.5 ± 0.3 | 24.7 ± 0.3 | 0.644 |
| Hypertension (%) | 90 (69.2) | 74 (74.7) | 0.360 |
| Diabetes mellitus (%) | 70 (53.8) | 49 (49.5) | 0.407 |
| Dyslipidemia (%) | 94 (72.3) | 75 (75.8) | 0.791 |
| Smoking history (%) | 78 (60.0) | 59 (59.6) | 0.950 |
| Preoperative AF (%) | 4 (3.1) | 1 (1.0) | 0.261 |
| NYHA | 1.6 ± 0.1 | 1.7 ± 0.1 | 0.725 |
| LAD, mm | 37.3 ± 0.4 | 37.9 ± 0.5 | 0.316 |
| LVDd, mm | 47.8 ± 0.5 | 49.1 ± 0.7 | 0.131 |
| LVDs, mm | 32.0 ± 0.6 | 32.7 ± 0.8 | 0.537 |
| IVST, mm | 9.7 ± 0.1 | 9.9 ± 0.1 | 0.266 |
| PWT, mm | 9.8 ± 0.1 | 10.0 ± 0.1 | 0.195 |
| LVEF, % | 61.0 ± 0.8 | 60.0 ± 1.4 | 0.540 |
| Operation time, min | 253.6 ± 5.7 | 248.4 ± 6.8 | 0.555 |
| Intubation time, h | 6.7 ± 0.7 | 5.6 ± 0.4 | 0.176 |
| Number of distal anastomosis | 3.2 ± 0.1 | 3.2 ± 0.1 | 0.964 |
| Right gastroepiploic artery graft (%) | 66 (50.8) | 52 (52.5) | 0.793 |
| Saphenous vein graft (%) | 47 (36.2) | 32 (32.3) | 0.470 |
| Blood transfusion (%) | 23 (17.7) | 19 (19.2) | 0.662 |
| Postoperative AF (%) | 31 (23.8) | 24 (24.2) | 0.936 |
| ICU stay, d | 1.2 ± 0.0 | 1.2 ± 0.0 | 0.895 |
| Hospital stay, d | 10.1 ± 0.3 | 10.7 ± 0.4 | 0.187 |
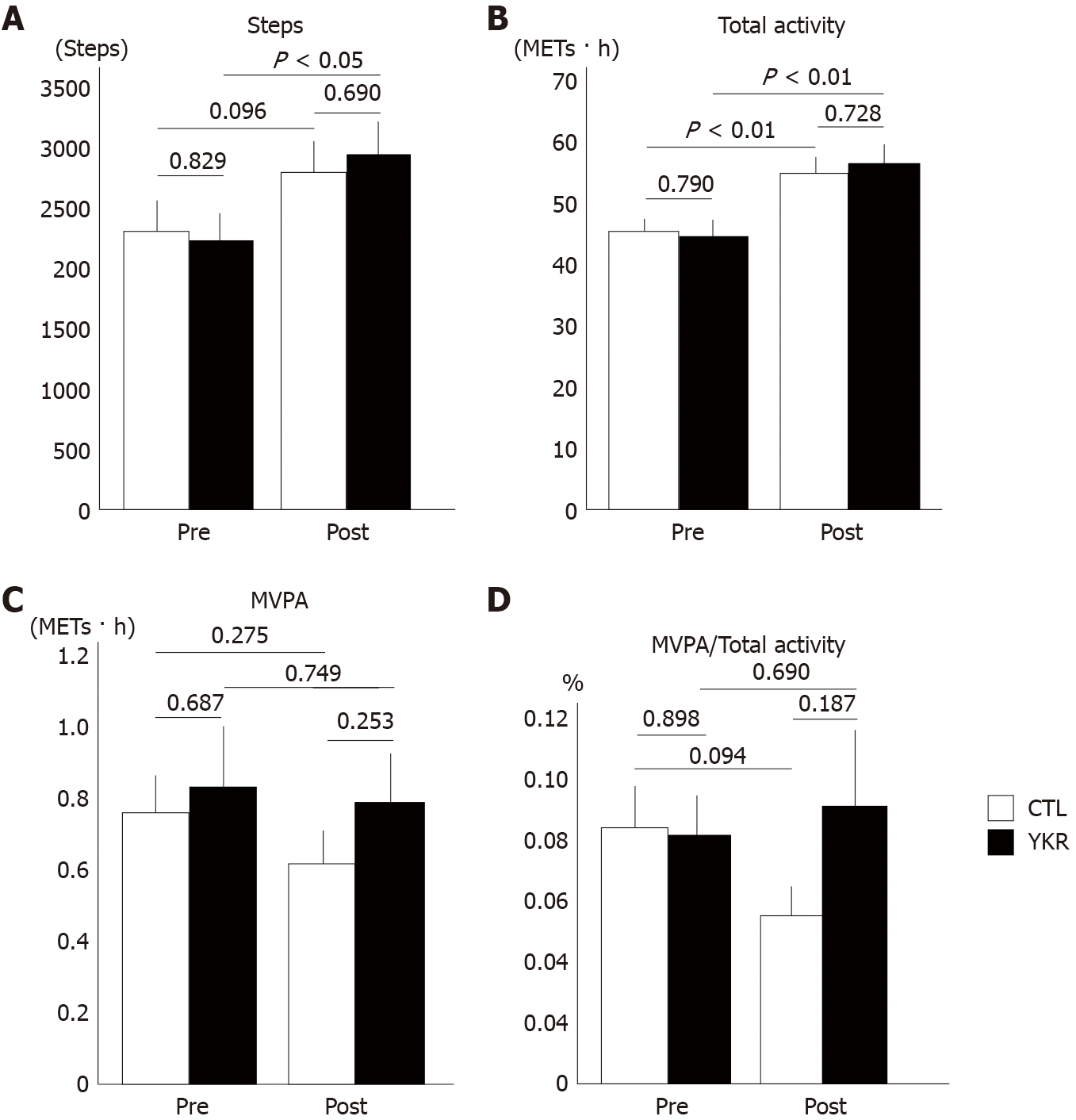
Figure 2 shows the number of preoperative and postoperative steps, activity, and MVPA, which were recorded using an accelerometer, in each group. The mean number of postoperative steps (Figure 2A) was increased in both groups, but only the increase in the YKR group was significant (preoperative vs postoperative: CTL, 2301 ± 253 steps vs 2787 ± 257 steps, P = 0.096; YKR: 2223 ± 225 steps vs 2943 ± 272 steps, P < 0.05).
The total activity (Figure 2B) significantly increased both in the CTL and YKR groups postoperatively (preoperative vs postoperative: CTL, 45.6 ± 1.9 METs∙h vs 55.1 ± 2.8 METs∙h, P < 0.01; YKR, 44.8 ± 2.6 METs∙h vs 56.6 ± 3.4 METs∙h, P < 0.01). The postoperative MVPA, an integrated activity of >3 METs, showed a nonsignificant decreasing trend in both groups (Figure 2C; preoperative vs postoperative: CTL, 0.76 METs∙h vs 0.61 METs∙h, P = 0.275; YKR, 0.83 METs∙h vs 0.79 METs∙h, P = 0.749). Despite the decreasing trend of the MVPA, the ratio of the MVPA to the total activity in the individual patients (Figure 2D) increased postoperatively in the YKR group. By contrast, it decreased in the CTL group, although no significant differences were found in the two groups (CTL, 0.084% ± 0.014% vs 0.055% ± 0.010%, P < 0.094; YKR, 0.081% ± 0.013% vs 0.091% ± 0.025%, P < 0.690).
The results of blood tests performed upon admission and on 2 POD and 7 POD are shown in Table 3. No significant differences were observed in the investigated indices between the groups at any period.
| Group | Pre | P value | 2 POD | P value | 7 POD | P value | 7-2 POD | P value | |
| WBC, × 109/L | CTL | 6.1 ± 0.3 | 0.991 | 12 ± 0.3 | 0.962 | 7.6 ± 0.2 | 0.534 | -4.4 ± 0.2 | 0.568 |
| YKR | 6.1 ± 0.2 | 12 ± 0.4 | 7.8 ± 0.2 | -4.2 ± 0.3 | |||||
| Hb, g/dL | CTL | 13.3 ± 0.1 | 0.645 | 11.2 ± 0.1 | 0.876 | 11.7 ± 0.1 | 0.130 | 0.5 ± 0.1 | 0.027a |
| YKR | 13.4 ± 0.2 | 11.3 ± 0.1 | 11.5 ± 0.1 | 0.2 ± 0.1 | |||||
| Hct, % | CTL | 39.2 ± 0.4 | 0.315 | 33.3 ± 0.3 | 0.854 | 34.6 ± 0.3 | 0.194 | 1.3 ± 0.2 | 0.053 |
| YKR | 39.8 ± 0.5 | 33.4 ± 0.4 | 34.0 ± 0.4 | 0.6 ± 0.3 | |||||
| TP, g/dL | CTL | 6.8 ± 0.0 | 0.616 | 5.7 ± 0.0 | 0.904 | 6.1 ± 0.1 | 0.789 | 0.4 ± 0.1 | 0.684 |
| YKR | 6.8 ± 0.0 | 5.7 ± 0.1 | 6.2 ± 0.1 | 0.5 ± 0.0 | |||||
| Alb, g/dL | CTL | 4.0 ± 0.0 | 0.482 | 3.5 ± 0.0 | 0.337 | 3.4 ± 0.0 | 0.385 | -0.1 ± 0.0 | 0.821 |
| YKR | 4.0 ± 0.0 | 3.5 ± 0.0 | 3.3 ± 0.0 | -0.1 ± 0.0 | |||||
| ChE, IU/L | CTL | 301.7 ± 6.9 | 0.953 | 176.3 ± 4.0 | 0.258 | 183.0 ± 4.0 | 0.227 | 6.7 ± 2.4 | 0.934 |
| YKR | 302.3 ± 7.8 | 183.3 ± 4.7 | 190.5 ± 4.6 | 7.0 ± 2.3 | |||||
| CK, IU/L | CTL | 101.3 ± 6.9 | 0.565 | 482.4 ± 22.7 | 0.443 | 67.8 ± 5.3 | 0.736 | -391.7 ± 16.9 | 0.878 |
| YKR | 95.3 ± 7.6 | 458.0 ± 19.8 | 70.2 ± 4.3 | -387.8 ± 18.2 | |||||
| ALP, IU/L | CTL | 217.2 ± 6.1 | 0.491 | 142.7 ± 3.1 | 0.734 | 201.4 ± 6.0 | 0.103 | 58.7 ± 5.3 | 0.097 |
| YKR | 210.8 ± 6.9 | 141.0 ± 4.1 | 222.8 ± 13.0 | 81.9 ± 12.8 | |||||
| T-Bil, mg/dL | CTL | 0.8 ± 0.1 | 0.194 | 1.2 ± 0.1 | 0.100 | 0.9 ± 0.0 | 0.580 | -0.3 ± 0.1 | 0.123 |
| YKR | 0.7 ± 0.0 | 1.0 ± 0.1 | 0.8 ± 0.1 | -0.2 ± 0.0 | |||||
| AST, IU/L | CTL | 21.8 ± 0.7 | 0.133 | 28.9 ± 0.9 | 0.748 | 20.1 ± 0.9 | 0.245 | -8.8 ± 1.1 | 0.556 |
| YKR | 23.6 ± 1.0 | 29.3 ± 1.0 | 21.6 ± 0.8 | -7.9 ± 1.0 | |||||
| ALT, IU/L | CTL | 21.4 ± 1.1 | 0.388 | 16.4 ± 1.0 | 0.543 | 20.3 ± 1.2 | 0.101 | 3.9 ± 1.3 | 0.244 |
| YKR | 23.1 ± 1.6 | 17.4 ± 1.3 | 23.7 ± 1.7 | 6.2 ± 1.5 | |||||
| γGTP, IU/L | CTL | 33.1 ± 2.0 | 0.352 | 24.3 ± 1.3 | 0.555 | 38.2 ± 3.2 | 0.540 | 14.0 ± 2.7 | 0.489 |
| YKR | 36.0 ± 2.5 | 25.5 ± 1.6 | 41.4 ± 3.9 | 16.9 ± 3.2 | |||||
| BUN, mg/dL | CTL | 16.8 ± 0.5 | 0.814 | 20.6 ± 0.5 | 0.667 | 17.7 ± 0.8 | 0.619 | -2.9 ± 0.7 | 0.840 |
| YKR | 16.6 ± 0.6 | 21.0 ± 0.7 | 18.3 ± 1.0 | -2.7 ± 0.9 | |||||
| Cre, mg/dL | CTL | 0.9 ± 0.0 | 0.606 | 1.0 ± 0.0 | 0.954 | 1.0 ± 0.1 | 0.828 | 0.0 ± 0.0 | 0.633 |
| YKR | 0.9 ± 0.0 | 1.0 ± 0.0 | 0.9 ± 0.0 | 0.0 ± 0.0 | |||||
| eGFR | CTL | 72.1 ± 1.9 | 0.219 | 68.0 ± 2.2 | 0.688 | 68.2 ± 2.0 | 0.816 | 0.2 ± 1.1 | 0.726 |
| YKR | 68.7 ± 2.0 | 66.7 ± 2.3 | 67.5 ± 2.3 | 0.8 ± 1.3 | |||||
| Na, mmol/L | CTL | 140.9 ± 0.2 | 0.752 | 140.9 ± 0.3 | 0.269 | 140.7 ± 0.2 | 0.604 | -0.2 ± 0.3 | 0.101 |
| YKR | 140.8 ± 0.3 | 140.4 ± 0.3 | 140.9 ± 0.3 | 0.5 ± 0.3 | |||||
| K, mmol/L | CTL | 4.3 ± 0.0 | 0.768 | 4.1 ± 0.0 | 0.416 | 3.9 ± 0.0 | 0.792 | -0.1 ± 0.3 | 0.360 |
| YKR | 4.3 ± 0.0 | 4.1 ± 0.0 | 3.9 ± 0.0 | 0.2 ± 0.3 | |||||
| CRP, mg/dL | CTL | 0.3 ± 0.1 | 0.407 | 15.7 ± 4.4 | 0.176 | 3.8 ± 2.4 | 0.586 | -11.9 ± 4.0 | 0.233 |
| YKR | 0.4 ± 0.1 | 14.9 ± 4.4 | 3.7 ± 1.8 | -11.2 ± 4.1 | |||||
| BNP, pg/mL | CTL | 90.4 ± 15.8 | 0.692 | 346.0 ± 30.1 | 0.554 | 264.0 ± 23.6 | 0.881 | -72.0 ± 12.6 | 0.653 |
| YKR | 99.0 ± 13.3 | 321.6 ± 24.5 | 258.6 ± 27.4 | -63.0 ± 15.7 |
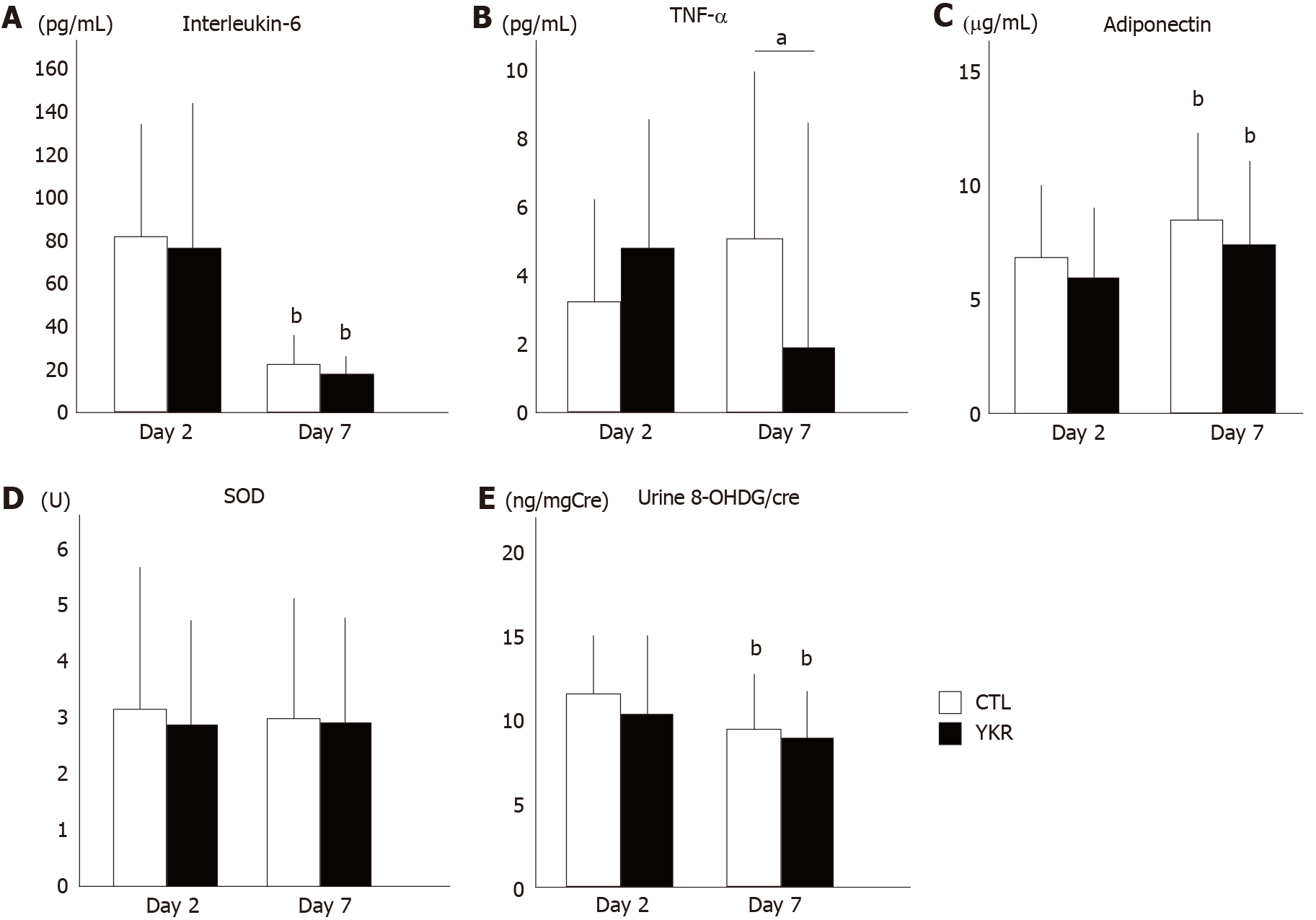
Next, the levels of inflammatory or stress-related cytokines (IL-6, TNF-α, adiponectin, and SOD, Figure 3A-D) and urinary stress hormones (8-OHDG/Cre ratio, Figure 3E) were measured on 2POD and 7POD. IL-6 Level significantly decreased in both groups (CTL: 81.5 ± 4.9 pg/mL to 21.5 ± 2.9 pg/mL, P < 0.01; YKR: 75.8 ± 7.2 pg/mL to 17.3 ± 2.7 pg/mL, P < 0.01, 2 POD to 7 POD, respectively). In addition, there were no significant differences between the two groups on 2 POD (P = 0.498) and on 7 POD (P = 0.301). A nonsignificant increasing trend was observed in TNF-α level in the CTL group, while a nonsignificant decreasing trend was observed in the YKR group (CTL: 3.2 ± 0.7 pg/mL to 5.0 ± 1.2 pg/mL, P = 0.686; YKR: 3.7 ± 0.9 pg/mL to 1.9 ± 0.2 pg/mL, P = 0.052, 2 POD to 7 POD, respectively). Notably, the TNF-α level in the YKR group was significantly lower than that in the CTL group (P < 0.01) on 7 POD, although no significant difference was observed on 2 POD (P = 0.623). Adiponectin level significantly increased in both groups (CTL: 6.8 ± 0.3 μg/mL to 8.5 ± 0.4 μg/mL, P < 0.01; YKR: 6.0 ± 0.3 μg/mL to 7.4 ± 0.4 μg/mL, P < 0.01, 2 POD to 7 POD, res
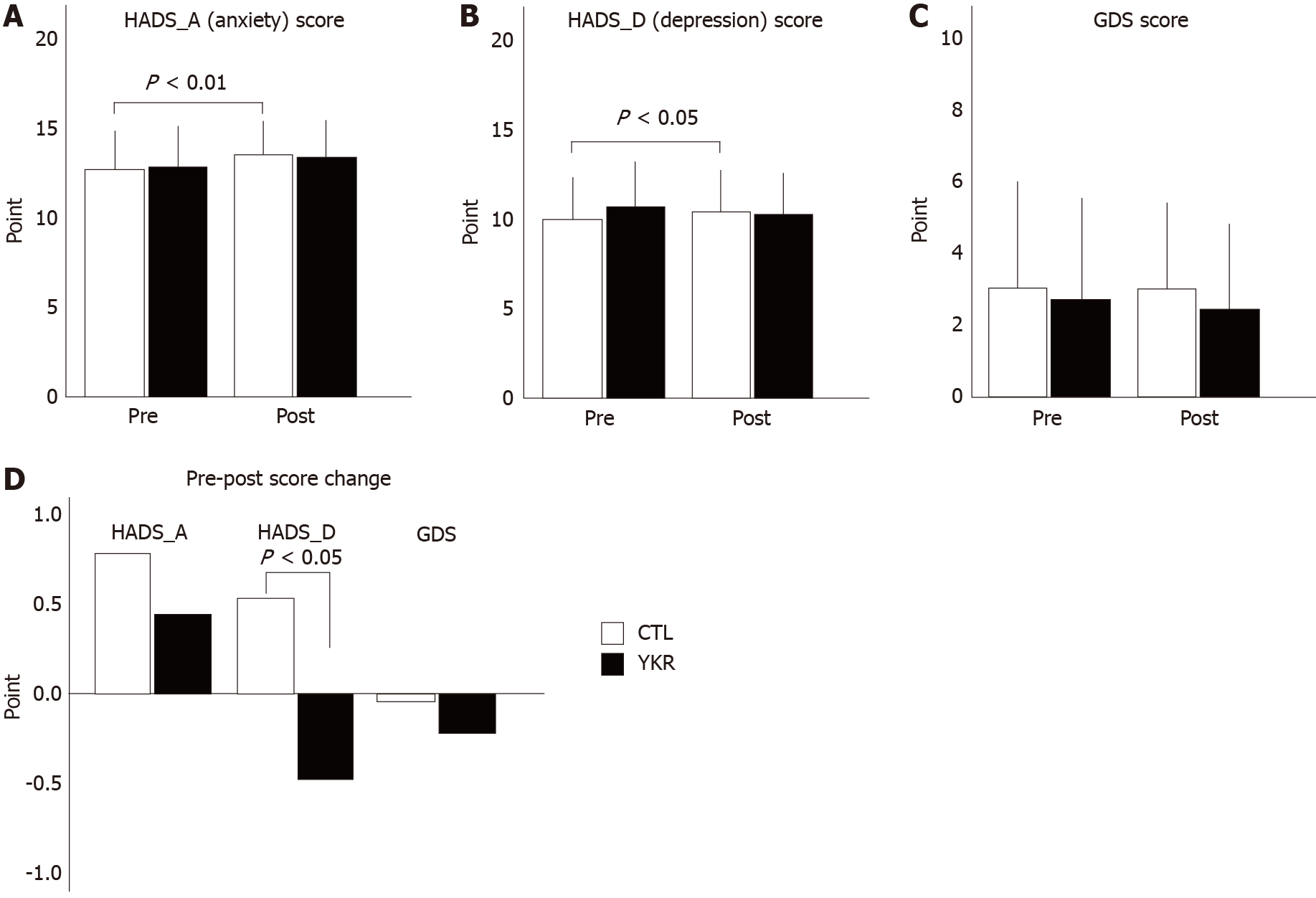
To assess anxiety and depression, the HADS and GDS were administered the patients were enrolled (preoperative) and on 7 POD. If the questionnaire was not completed, the sheet was considered as void and the answers were not included in the results. Finally, 144 of 229 (87 from the CTL group and 57 from the YKR group) HADS sheets and 151 of 229 (92 from the CTL group and 60 from the YKR group) GDS sheets were eligible for analyses. The HADS can assess both anxiety and depression. If each score was more than 11 points, the patients was considered “positive” for anxiety and depression. For GDS, a score of > 5 was considered as “positive” for anxiety and depression. The number of patients with positive anxiety and depression is shown in Table 4, while the actual points (Figure 4A-C) and changes in scores (Figure 4D) are shown in Figure 4. HADS_A (anxiety) significantly increased postoperatively in the CTL group (12.6 ± 0.2 points vs 13.4 ± 0.3 points, preoperative vs postoperative, P < 0.01). YKR also showed an increasing trend in HADS_A; however, the trend was not statistically significant (12.8 ± 0.3 points vs 13.3 ± 0.3 points, preoperative vs postoperative, P = 0.078; Figure 4A). In addition, as shown in Figure 4D, there was no significant difference in perioperative HADS_A between the two groups (0.8 vs 0.5, CTL vs YKR, respectively, P = 0.317).
| Group | Pre (%) | Post (%) | Pre vs post | Improve | Worsen | |
| HADS_A (≥ 11) | CTL | 74 (85.1) | 82 (94.3) | < 0.05 | 3 (3.4) | 11 (12.6) |
| YKR | 50 (87.7) | 50 (87.7) | 1.00 | 4 (7.0) | 4 (7.0) | |
| HADS_D (≥ 11) | CTL | 31 (35.6) | 43 (49.4) | < 0.05 | 7 (8.0) | 19 (21.8) |
| YKR | 29 (50.9) | 23 (40.4) | 14 (24.6) | 9 (15.8) | ||
| GDS (≥ 5) | CTL | 26 (28.3) | 25 (27.2) | 10 (10.9) | 9 (9.8) | |
| YKR | 14 (23.7) | 12 (20.3) | 6 (10.5) | 3 (5.3) |
Similarly, HADS_D (depression) significantly increased postoperatively in the CTL group (9.8 ± 0.3 points vs 10.3 ± 0.2 points, preoperative vs postoperative, P < 0.05, Figure 4B). In contrast, HADS_D decreased in the YKR group (10.5 ± 0.3 points vs 10.1 ± 0.3 points, preoperative vs postoperative, P = 0.192), and the change was statistically significant compared with that in the CTL group (Figure 4D, P = 0.018).
The GDS score in both groups showed a decreasing trend, although no significant difference was observed between the two groups (CTL: 3.0 ± 0.3 points vs 3.0 ± 0.3 points, preoperative vs postoperative, P = 0.849, YKR: 3.0 ± 0.3 points vs 3.0 ± 0.3 points, preoperative vs postoperative, P = 0.327). In addition, the change in HADS_D was not statistically different between the two groups (P = 0.588), although the YKR group seemed to show a more decreasing trend in score change.
In this study, we demonstrated that the daily intake of a nutritional supplement drink postoperatively has positive effects including enhancement of rehabilitation, reduction of inflammation, and improvement of anxiety score in patients who underwent OPCAB surgery.
Previous studies revealed that 30%-50% of patients who experience coronary artery disease are likely to show depression[10]. In our experiment, 41.7% of the patients experienced depression (HADS_D positive) and 86.1% felt anxious (HADS_A positive) preoperatively. Unexpectedly, the number of patients who expressed anxiety and depression increased after rather than before surgery in the CTL group. As the mean length of postoperative hospital stay was around 10 days, many patients at 7 POD might feel anxiety concerning their lives after returning to home in a few days. By contrast, the number of patients who experienced depression (HADS_D) decreased in the YKR group, which suggests that consuming the drink may alleviate depressive moods. In fact, some of the contents of the drink (Table 1) are reported to improve stress and depression. Crude medicines, such as the extract from Ginseng roots or leaves, Rehmannia root, or royal jelly, have been widely used as herbal medications, especially in East Asian countries. Although the mechanism of the effect has not been fully elucidated, it has been demonstrated that the administration of ginseng saponin (ginsenoside Rb1) reduced stress and anxiety in both animal[11] and human models after a few days[12]. Catalpol, a major compound found in Rehmannia roots, showed antidepressant properties in rat models[13]. In addition, consuming Melbrosia, a mixture of royal jelly and bee pollen, improved depression and irritability scores in postmenopausal women[14]. These findings suggest that consuming these contents can improve the anxiety score, although it was difficult to specify which content was effective or if ingestion of multiple contents may enhance the effect. In addition, another study reported that women were more likely experience depression; however, our analysis did not show sex differences in preoperative depression or anxiety as well as in score change (data not shown).
We evaluated the patients’ level of physical activity using an accelerometer. The device used in this study can measure both the number of steps and activity. Recently, MVPA (3 > METs × hour) has been shown to be important[15-17].
In this study, the number of steps was significantly increased postoperatively in the YKR group, but no significant differences were found between the groups preoperatively and postoperatively. In addition, the postoperative total activity increased in both groups. By contrast, the MVPA decreased in the postoperative period in both groups, indicating that vigorous movement was limited postoperatively owing to the presence of pain, intravenous catheters, or drains. However, the ratio of the MVPA to the total activity was increased in the YKR group, despite that it was decreased in the CTL group, indicating that the YKR group had more vigorous and quantitative movements than the CTL group. These results indicate that the YKR group can perform more favorable postoperative rehabilitation.
Inflammation plays an important role in maintaining homeostasis against injury, which can be due to surgical stress. Especially for cardiac surgery, extracorporeal perfusion is one of the important factors that can enhance inflammation due to exposure to artificial materials and non-physiological blood flow to the organs. Excessive activation and prolongation of inflammation may cause organ dysfunction. The expression of inflammatory cytokines, such as TNF-α and IL-6, is associated with postoperative complications[18,19]. Although the reports were controversial, the off-pump technique attenuates increase in inflammatory cytokine levels, such as TNF-α, IL-6, and IL-8[19-24], which may decrease the risk of renal dysfunction or surgical complications[25-28]. The levels of these inflammatory cytokines peaked during or within 48 h postoperatively in patients who underwent OPCAB, with an IL-6 Level of 35-400 pg/mL[25,26] and TNF-α level of 4-25 pg/mL[20,23,29].
In this study, we recruited patients who underwent OPCAB surgery, which was our standard procedure for isolated CABG cases (97.9% in last five years). We measured the cytokine levels on 2POD and 7POD; the average IL-6 level was 80 pg/mL, while the average TNF-α level was < 5 pg/mL. Compared with results of previous studies, our results exceeded the peak value. Under these conditions, the levels of one of the inflammatory markers, TNF-α, was significantly reduced in the YKR group (2 POD vs 7 POD), while they remained high in the CTL group. Some herbal medicines, contained in the drink, such as ginseng, Jiou, and royal jelly, have been reported to reduce the inflammation[12,30]. This result indicates that YKR prevents the prolongation of inflammation, although the level of other cytokines did not reach significance.
One of the most common complications after cardiac surgery is AF, which occurs in 20%-40% of patients postoperatively. The occurrence of AF has been shown to be associated with inflammation. In this study, despite the reduction in inflammation after consuming the supplement drink, no differences were observed in the occurrence of postoperative AF between the two groups. In addition, no differences were observed in the length of hospital stay and other postoperative complications. Importantly, results of perioperative blood tests suggest that the drink had no harmful effects on the kidney, liver, or other organs. In addition, a caffeine-free drink was used in this study since caffeine enhances sympathetic activity, which may increase the risk of arrhythmia.
This study has some limitations. First, the drink contains several crude medications; hence, it is difficult to detect which contents contributed to the effect. Furthermore, since no placebo group was included in this study, it was unclear whether the behavior of “consuming a special drink” affected the results. Second, although the characteristics of the patients were not different between the groups, the social backgrounds of the patients varied. This difference may have an effect on a patient’s level of anxiety or may motivate them to discharge early from the hospital. Third, we did not assess the seasonal effect of taking these medications in these patients. Last, we did not assess the long-term effect of the medications in the patients.
We demonstrated that consuming commercially available nutritional supplement drinks after OPCAB surgery reduced inflammation and mental deterioration. This may be associated with enhancement of postoperative rehabilitation as well as improvement of outcome and postoperative quality of life. Consuming the drink may be a novel option as a supplemental medication for high-risk patients.
Some patients who underwent coronary artery bypass graft surgery still suffered from depression and prolongation of hospital stay after surgery, although postoperative complications are reduced with the technical development such as the off-pump technique. Recently, patients with low cardiac function, high age, frail, or complicated conditions who often delayed postoperative rehabilitation are increased. These patients are potentially frail and exhibit systemic deterioration.
Consuming nutritional supplement drink when a person experiences fatigue or develops illnesses such a cold is a widely accepted practice in our society. Various kinds of nutritional supplement drinks are commercially available in Japan. These drink should be safe and useful for these patients after surgery.
We aimed to investigate the effect of taking an herbal medicine-containing, commercially available drink for postoperative rehabilitation in those patients.
Patients who underwent isolated off-pump coronary artery bypass (OPCAB) surgery were divided into two groups: (a) consumed one bottle of a caffeine-free nutritional supplement drink on a daily basis (YKR group), and (b) underwent regular rehabilitation (CTL group).
Although there were no differences in postoperative complications and the duration of postoperative hospital stay between the two groups, the YKR group had a significantly increased number of daily steps postoperatively (P < 0.05) and had significantly lower postoperative serum tumor necrosis factor-alpha levels (P < 0.01), while no significant differences were observed in the levels of other inflammatory or stress-related cytokines (interleukin-6, adiponectin, superoxide dismutase, and urine 8-hydroxy-2′-deoxyguanosine) between the two groups. Also, the YKR group showed a significant improvement in the Hospital Anxiety and Depression Score (P < 0.05).
The daily intake of an herbal medicine-containing drink after OPCAB surgery may have beneficial effects on cardiac rehabilitation by reducing inflammation markers and depression.
The drink contains herbal medicine, vitamin and other materials. We should investigate what contain works the most effectively.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng TH S-Editor: Gao CC L-Editor: A P-Editor: Liu JH
| 1. | Froelicher V, Jensen D, Sullivan M. A randomized trial of the effects of exercise training after coronary artery bypass surgery. Arch Intern Med. 1985;145:689-692. [PubMed] |
| 2. | Adachi H, Itoh H, Sakurai S, Takahashi T, Toyama T, Naito S, Hoshizaki H, Oshima S, Taniguchi K, Kato M, Fu LT, Kato K. Short-term physical training improves ventilatory response to exercise after coronary arterial bypass surgery. Jpn Circ J. 2001;65:419-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Nakai Y, Kataoka Y, Bando M, Hiasa Y, Taki H, Harada M, Maeda T, Aihara T. Effects of physical exercise training on cardiac function and graft patency after coronary artery bypass grafting. J Thorac Cardiovasc Surg. 1987;93:65-72. [PubMed] |
| 4. | Goodman JM, Pallandi DV, Reading JR, Plyley MJ, Liu PP, Kavanagh T. Central and peripheral adaptations after 12 wk of exercise training in post-coronary artery bypass surgery patients. J Cardiopulm Rehabil. 1999;19:144-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Dracup K, Moser DK, Marsden C, Taylor SE, Guzy PM. Effects of a multidimensional cardiopulmonary rehabilitation program on psychosocial function. Am J Cardiol. 1991;68:31-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Thomas JJ. Reducing anxiety during phase I cardiac rehabilitation. J Psychosom Res. 1995;39:295-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Yanatori M, Tomita S, Miura Y, Ueno Y. Feasibility of the fast-track recovery program after cardiac surgery in Japan. Gen Thorac Cardiovasc Surg. 2007;55:445-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Kornfeld DS, Heller SS, Frank KA, Wilson SN, Malm JR. Psychological and behavioral responses after coronary artery bypass surgery. Circulation. 1982;66:III24-III28. [PubMed] |
| 9. | Churchill JD, Gerson JL, Hinton KA, Mifek JL, Walter MJ, Winslow CL, Deyo RA. The nootropic properties of ginseng saponin Rb1 are linked to effects on anxiety. Integr Physiol Behav Sci. 2002;37:178-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Lee S, Rhee DK. Effects of ginseng on stress-related depression, anxiety, and the hypothalamic-pituitary-adrenal axis. J Ginseng Res. 2017;41:589-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 11. | Wang JM, Yang LH, Zhang YY, Niu CL, Cui Y, Feng WS, Wang GF. BDNF and COX-2 participate in anti-depressive mechanisms of catalpol in rats undergoing chronic unpredictable mild stress. Physiol Behav. 2015;151:360-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 12. | Georgiev DB, Metka M, Huber JC, Goudev AR, Manassiev N. Effects of an herbal medication containing bee products on menopausal symptoms and cardiovascular risk markers: results of a pilot open-uncontrolled trial. MedGenMed. 2004;6:46. [PubMed] |
| 13. | Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM, Troiano RP, Sprow K, Torres A, Piercy KL; 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE*. Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med Sci Sports Exerc. 2019;51:1270-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 360] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 14. | Ushio M, Kanaoka M, Kinoshita Y, Maeno S, Fujita K. Moderate-to-vigorous physical activity and the risk of stroke recurrence in patients with a history of minor ischemic stroke in Japan: a retrospective analysis. Top Stroke Rehabil. 2018;25:591-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Hamer M, Venuraju SM, Lahiri A, Rossi A, Steptoe A. Objectively assessed physical activity, sedentary time, and coronary artery calcification in healthy older adults. Arterioscler Thromb Vasc Biol. 2012;32:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Tønnesen E, Christensen VB, Toft P. The role of cytokines in cardiac surgery. Int J Cardiol. 1996;53 Suppl:S1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Greenberg JW, Lancaster TS, Schuessler RB, Melby SJ. Postoperative atrial fibrillation following cardiac surgery: a persistent complication. Eur J Cardiothorac Surg. 2017;52:665-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 230] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 18. | Matata BM, Sosnowski AW, Galiñanes M. Off-pump bypass graft operation significantly reduces oxidative stress and inflammation. Ann Thorac Surg. 2000;69:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 185] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 19. | Raja SG, Berg GA. Impact of off-pump coronary artery bypass surgery on systemic inflammation: current best available evidence. J Card Surg. 2007;22:445-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 20. | Andrási TB, Mertens F, Barabás B, Blázovics A. Effect of haemodynamic changes on epithelium-related intestinal injury in off-pump coronary surgery. Heart Lung Circ. 2014;23:144-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Chello M, Mastroroberto P, Quirino A, Cuda G, Perticone F, Cirillo F, Covino E. Inhibition of neutrophil apoptosis after coronary bypass operation with cardiopulmonary bypass. Ann Thorac Surg. 2002;73:123-129; discussion 129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Meng F, Ma J, Wang W, Lin B. Meta-analysis of interleukin 6, 8, and 10 between off-pump and on-pump coronary artery bypass groups. Bosn J Basic Med Sci. 2017;17:85-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Massoudy P, Wagner S, Thielmann M, Herold U, Kottenberg-Assenmacher E, Marggraf G, Kribben A, Philipp T, Jakob H, Herget-Rosenthal S. Coronary artery bypass surgery and acute kidney injury--impact of the off-pump technique. Nephrol Dial Transplant. 2008;23:2853-2860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Vallely MP, Bannon PG, Bayfield MS, Hughes CF, Kritharides L. Endothelial activation after coronary artery bypass surgery: comparison between on-pump and off-pump techniques. Heart Lung Circ. 2010;19:445-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Wippermann J, Albes JM, Brandes H, Kosmehl H, Bruhin R, Wahlers T. Acute effects of tourniquet occlusion and intraluminal shunts in beating heart surgery. Eur J Cardiothorac Surg. 2003;24:757-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Kowalewski M, Pawliszak W, Malvindi PG, Bokszanski MP, Perlinski D, Raffa GM, Kowalkowska ME, Zaborowska K, Navarese EP, Kolodziejczak M, Kowalewski J, Tarelli G, Taggart DP, Anisimowicz L. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: Meta-analysis. J Thorac Cardiovasc Surg. 2016;151:60-77.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 143] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 27. | Zawar BP, Mehta Y, Juneja R, Arora D, Raizada A, Trehan N. Nonanalgesic benefits of combined thoracic epidural analgesia with general anesthesia in high risk elderly off pump coronary artery bypass patients. Ann Card Anaesth. 2015;18:385-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Makino T, Hamanaka M, Yamashita H, Mizukami H. Effect of bakumijiogan, an herbal formula in traditional Chinese medicine, on atopic dermatitis-like skin lesions induced by mite antigen in NC/Jic mice. Biol Pharm Bull. 2008;31:2108-2113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Kohno K, Okamoto I, Sano O, Arai N, Iwaki K, Ikeda M, Kurimoto M. Royal jelly inhibits the production of proinflammatory cytokines by activated macrophages. Biosci Biotechnol Biochem. 2004;68:138-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 160] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 30. | Saboori S, Falahi E, Yousefi Rad E, Asbaghi O, Khosroshahi MZ. Effects of ginseng on C-reactive protein level: A systematic review and meta-analysis of clinical trials. Complement Ther Med. 2019;45:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |