Published online Aug 26, 2021. doi: 10.4330/wjc.v13.i8.298
Peer-review started: March 3, 2021
First decision: March 31, 2021
Revised: April 13, 2021
Accepted: August 5, 2021
Article in press: August 5, 2021
Published online: August 26, 2021
Processing time: 174 Days and 2.4 Hours
Coronavirus disease 2019 infection has spread worldwide and causing massive burden to our healthcare system. Recent studies show multiorgan involvement during infection, with direct insult to the heart. Worsening of the heart function serves as a predictor of an adverse outcome. This finding raises a particular concern in high risk population, such as those with history of preexisting heart failure with or without implantable device. Lower baseline and different clinical characteristic might raise some challenge in managing either exacerbation or new onset heart failure that might occur as a consequence of the infection. A close look of the inflammatory markers gives an invaluable clue in managing this condition. Rapid deterioration might occur anytime in this setting and the need of cardiopulmonary support seems inevitable. However, the use of cardiopulmonary support in this patient is not without risk. Severe inflammatory response triggered by the infection in combination with the preexisting condition of the worsening heart and implantable device might cause a hypercoagulability state that should not be overlooked. Moreover, careful selection and consideration have to be met before selecting cardiopulmonary support as a last resort due to limited resource and personnel. By knowing the nature of the disease, the interaction between the inflammatory response and different baseline profile in heart failure patient might help clinician to salvage and preserve the remaining function of the heart.
Core Tip: Coronavirus disease 2019 (COVID-19) infection might cause severe res
- Citation: Raffaello WM, Huang I, Budi Siswanto B, Pranata R. In-depth review of cardiopulmonary support in COVID-19 patients with heart failure. World J Cardiol 2021; 13(8): 298-308
- URL: https://www.wjgnet.com/1949-8462/full/v13/i8/298.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i8.298
Coronavirus disease 2019 (COVID-19) is an emerging viral infection which has caused global pandemic with resulting both high global economic burden and mortality rate[1,2]. It also caused an alteration and restructuration in our healthcare system, especially in treating patients with infection and chronic disease[3]. Patients with both condition of COVID-19 and prior cardiovascular disease have an increased risk of cardiovascular complications which severely affect the mortality rate.
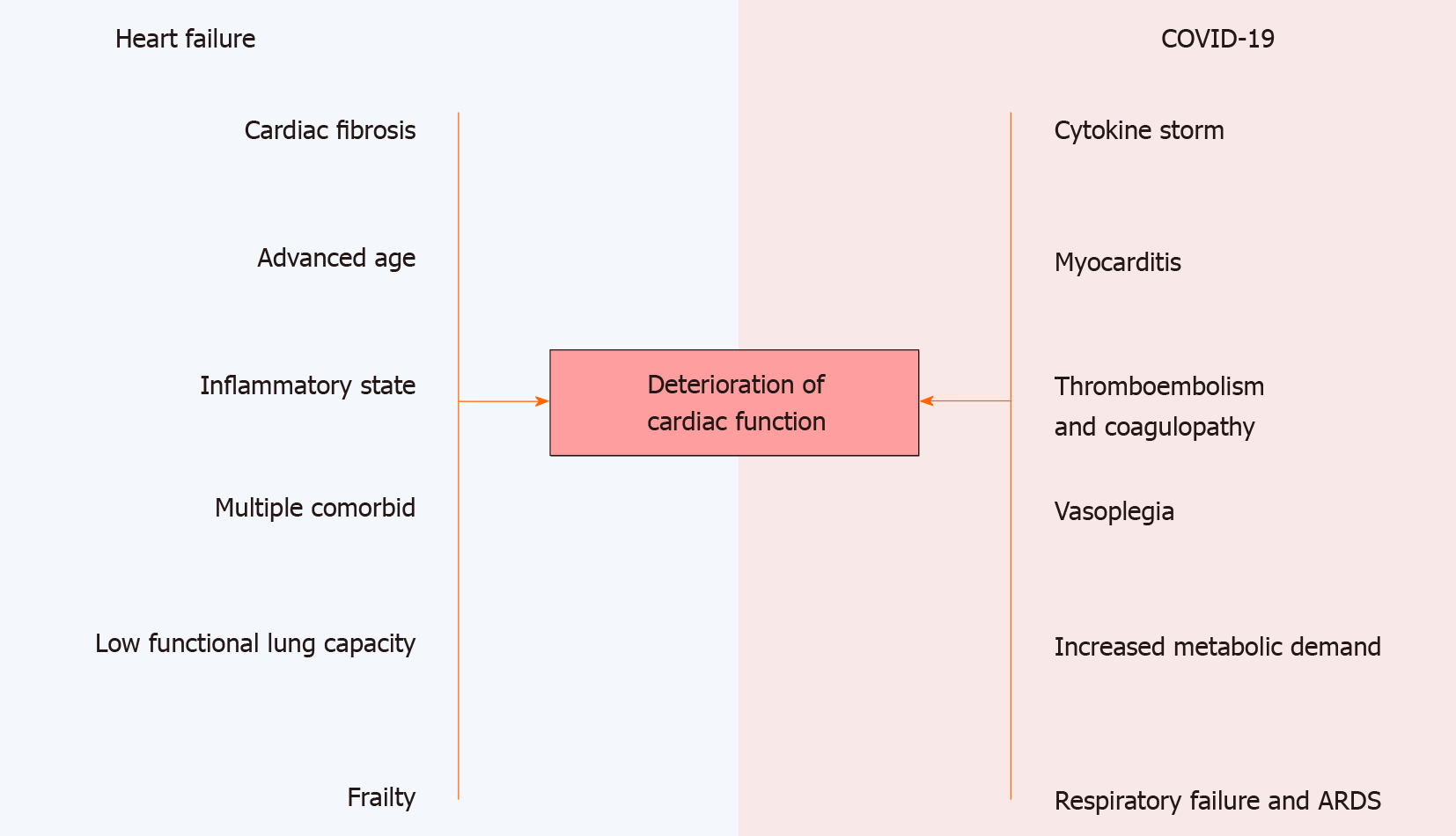
COVID-19 is also associated with higher incidence of cardiovascular complication in compare to previous coronavirus outbreaks[4,5]. Deterioration of the cardiac function is prominent in COVID-19 and those with lower baseline function are prone to further decline in cardiac function. A study demonstrate the preexistence of chronic heart failure (CHF) and high cardiac biomarkers is associated with worse outcome[6]. Recent study also shows that patient with heart failure (HF) is associated with an increased risk of mechanical ventilation and overall mortality regardless of left ventricular ejection fraction (LVEF)[7].
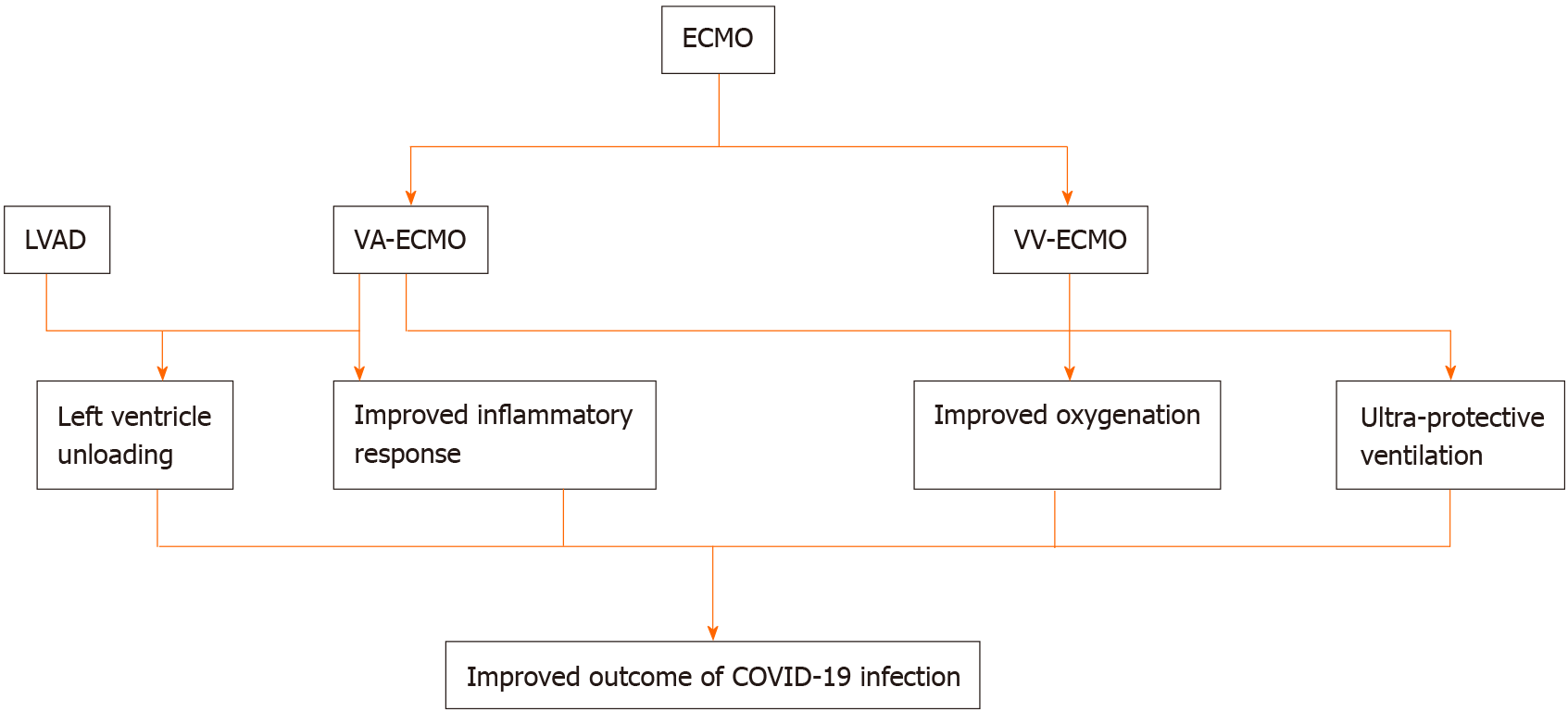
The use of cardiopulmonary support in COVID-19 shares the same prominent role in managing severe conditions such as severe respiratory distress and heart failure[3,8]. However, there are several distinct clinical characteristics of HF patients which may differ from non-pre-existing HF patients. These factors have to be considered before choosing cardiopulmonary support as a treatment of choice. Another challenging issue is the highly selective inclusion and exclusion criteria before a patient is eligible for the use of extracorporeal membranous oxygenation (ECMO). Therefore, the management of both HF and COVID-19 has to be tailored since the concept of one treatment fits all might not suitable in these patients.
The mechanism of cardiac function disturbance in COVID-19 is poorly understood and it is thought to be an interaction between several mechanisms including direct myocardial injury, cytokine release, prothrombotic state causing microvascular thrombosis and exacerbation of underlying cardiovascular disease[3,9-13]. In the context of COVID-19, CHF patients are vulnerable to acute exacerbation. These patients are at risk because of their lower baseline status which unable to cope with the increasing metabolic demand in systemic inflammation triggered by the infection[14]. In the settings of advanced HF with left ventricular assisted device (LVAD) support, functional capacity of the lung has already impaired and contributes even more to the decrease of the cardiopulmonary reserve[15,16].
Several studies have demonstrated more severe infections and higher mortality rate in patients with preexisting cardiovascular disease[6,7,14,17]. Older age along with other comorbid such as obesity, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, atrial fibrillation, chronic kidney disease and frailty are seems to be more prevalent in the HF group and might contribute to an increased rate of mortality and morbidity[7,18]. Moreover, these patients generally have a reduced immunity, general frailty, an tend to be in an inflammatory state[14,19].
A lower pulmonary function is commonly found in HF patients and is contributed mainly by chronic obstructive pulmonary disease (COPD)[20]. Combination of underlying parenchymal disease and elevated left ventricular filling pressure leads to the development of pulmonary hypertension[21]. In COVID-19 infection, respiratory failure and acute respiratory distress syndrome (ARDS) further exacerbates pulmonary vasoconstriction and interstitial edema. This condition is further worsened by pre-existing biventricular failure and ARDS that eventually lead to right ventricular function impairment.
Recent studies have shown that COVID-19 is associated with acute myocardial involvement which described as an acute cardiac injury[3,12,13]. A suspicion of cardiac involvement in COVID-19 is best described by an elevation in cardiac biomarker [high-sensitivity troponin (hs-TnI)] above 99th percentile upper reference limit[13,22]. Early reports had been analyzed, with notable findings suggest an increased level of cardiac troponin was associated with admission to intensive care and higher in hospital mortality[12,23-26]. A careful observation of endomyocardial biopsy in COVID-19 patients has revealed an evidence of acute myocardial inflammation through the presence of viral particles and a diffuse myocardial edema on cardiac magnetic resonance, therefore raising the suspicion of direct viral myocardial invasion[27]. Severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV2) binds with angiotensin-converting enzyme 2 (ACE2) receptor and with the help of transmembrane protease serine 2 (TMPRSS2), facilitates viral entry through the cell[28,29]. ACE2 and TMPRSS2 are widely expressed in various tissue, including the heart, and might explain the involvement of heart during the course of infection[29]. Viral inclusion bodies were found from the biopsy of myocardial tissue along with identification of SARS-CoV2 genomic RNA in patients with suspected COVID-19 myo
Myocardial infarction plays a significant role in the development of acute HF in COVID-19 infection. Both Type I and II myocardial infarction might occur in patient with COVID-19, worsening the function in an already impaired baseline function[3]. This may leads to worse outcome in patient with a history of HF[3].
Cardiac arrhythmia is a major concerning issue in the context of HF and COVID-19 infection. Careful observation of the heart rate and rhythm are vitals in the clinical settings. Atrioventricular block, atrial fibrillation, polymorphic ventricular tachycardia and pulseless electrical activity have been closely associated with COVID-19 despite of the unknown mechanism of how these rhythms abnormalities may develop[22,35]. QT prolongation is constantly a thread, considering that QT prolongation is an inde
Profound cytokine release in the setting of severe COVID-19 infection is commonly found. The release of proinflammatory cytokines, increased metabolic demand and coagulation disorder in sepsis may contribute to the development of new onset HF and decompensation episodes in CHF[41]. Cytokine storm is observed in viral induced infection such as influenzae and COVID-19 and in the setting of graft-versus-host disease. Lymphopenia, C-reactive protein, lactate dehydrogenase, ferritin, D-dimer and troponin are among the biomarkers that reflect the severity of the hyperinflammatory state[42,43]. In HF, the inflammation happened as a response to the myocardial stressors. Multiple preexisting comorbidities that might further contribute to the profound inflammatory response are coronary artery disease, hypertension, arrhythmia, diabetes, and obesity. Increased level of inflammatory cytokine directly linked to the deterioration of the heart function[44,45]. The increased level of several cytokines such as tumor necrosis-alpha (TNF-α), interleukin-1 beta (IL-1β), interleukin-6 (IL-6) and galectin-3 may predict worse outcome in HF patients[46,47]. Interestingly, an elevation of IL-6 Level is also seems to be correlated with mortality in COVID-19 infection[48]. Moreover, the systemic hyperinflammation state that might occur in the setting of COVID-19 has extrapulmonary involvement and causing additional burden to the heart. The effect of hyperinflammation is well reflected by an elevation of cardiac biomarkers such as troponin and N-terminal pro B-type natriuretic peptide[43]. In this stage, vasoplegia and myocarditis might also occur[43].
Pro-inflammatory response which is induced by the infection might worsen hypoxia which in turn causing more stress to the damaged heart[42]. Hypoxia serves as a risk factor of survival in COVID-19 patients and should not be overlooked since it has deleterious effect in patients with HF and COVID-19[49]. Acute respiratory distress syndrome and exaggerated inflammatory response contributes to the development of hypoxia which may cause cardiac lesion and further exacerbates HF[50-53].
Coagulopathy is a common disorder found in COVID-19 infection. It is thought that the interaction between host defense mechanism and coagulation system during COVID-19 infection may lead to hypercoagulability and a high prevalence of thrombotic events[54-56]. This finding is reinforced by an elevated D-dimer level which is often present in the setting of COVID-19 infection[5,55]. The combination of endothelial dysfunction, inflammatory state, oxidative stress and platelet activation are thought to be responsible for a hypercoagulable state[1,5,55]. The true nature of the course is remain unknown to date, however the role of endothelial activation cannot be overlooked. It is thought that ACE2 receptor that serves as an entry point for the SARS-CoV-2 into the cell, plays an important role[57,58]. The presence of ACE2 receptors on the endothelial cells as well as antithrombin (AT), heparin and other anticoagulation might play an important role in regulating the inflammatory response[57]. AT interacts with heparin-like glycosaminoglycan (GAG) on endothelial surface and therefore involved in the release of prostacyclin which will inhibit leukocyte activation by decreasing IL-6 Level[57,59]. The hypercoagulability state is also involved in the development of both micro- and macrovascular thrombus and may also plugs the extracorporeal circuits[5,55]. Grave consequence of thrombosis may occur in COVID-19 patients as it may present as pulmonary venous thrombosis leading to right heart failure and or microvascular thrombosis may leads to myocardial dysfunction, worsening the heart function[5,55,60-62].
Patients with a preexisting history of heart failure are already in an increased risk for developing thromboembolism due to venous stasis, endothelial injury, ischemic cardiomyopathy and atrial fibrosis[63,64]. This condition might be worsened by the presence of COVID-19 infection which may trigger coagulopathy and the presence of implantable device which also may trigger thrombosis[65,66]. The pre-existing cardiopulmonary support such as left ventricular assisted device (LVAD) alone might increase the risk of developing pump thrombosis, although the risk of stroke with co-existing COVID-19 infection has not been assessed yet[3,67].
Patient with COVID-19 might require mechanical circulatory support as a con
However, the use of these devices is remain in question since significant resources such as specialized equipment and trained personnel are needed to plant and maintain the device[4,42]. The decision of implanting the device might be considered for patients with ARDS and or cardiogenic shock refractory to traditional management with favorable outcome with the use of the device[68]. Close monitoring is also essential and health care workers exposure is also needed to be looked closely[42]. Still, despite the use of cardiopulmonary support, management of patients with HF and COVID-19 infection remain difficult due to complex interaction between the volume status and the biventricular dynamics[42]. There are also strict criterias have to be met before implanting ECMO in COVID-19 patient. While there are no difference for indication of ECMO between COVID-19 and non-COVID-19 patient, there are several things to be remembered[68]. First, careful selection is needed as patients with advanced age and significant comorbidities might not have much benefit from the use of ECMO. Also, patient with underlying CHF tend to be older, have multiple existing comorbidities and often fall into profound clinical status in the natural course of COVID-19 infection[6,7,14]. Therefore, the use of ECMO should be restricted in these patients unless there are a reasonable chance of recovery[5]. The use of ECMO should be carefully taken, considering that the hospital capacities and resources are limited in most settings and the possible outcome that the patient might achieve[5,42,68].
There are some small subset of patient who may choose another options in regard to the treatment of advanced HF. Patients who are not eligible for the heart transplant might use the left ventricular assist device (LVAD). However, the use of this device is not without risk, especially in the context of COVID-19 infection. These patients are known to have different types of HF that may produce different inflammatory profile in response to the implanted device[47]. To the best of our knowledge, until now there are no specific indication of when to implant ventricular assist device (VAD) in the context of severe COVID-19. First reported case of VAD implantation in patient with COVID-19 infection demonstrate the possibility of VAD as an alternative in a setting of prolonged cardiogenic shock and hemodynamical instability with modest chance of VA ECMO weaning[65]. Careful consideration and assessment of patient’s clinical status has to be put in top priority in determining when to implant the device. The indications and contraindications for ECMO in COVID-19 is described in Table 1.
| Indications for ECMO | Contraindications for ECMO |
| V-V ECMO; PaO2/FiO2 < 60 mmHg for > 6 h < 50 mmHg for > 3 h; pH < 7.2 with PaCO2 > 80 mmHg for > 6 h | Relative contraindications; Age ≥ 65 yr old; Body mass index ≥ 40; Immunocompromised status; No legal medical decision maker available; Advanced chronic underlying systolic heart failure; High dose vasopressor requirement (and not under consideration for VA or V-VA ECMO); Absolute contraindications; Advanced age; Clinical frailty scale category ≥ 3; Mechanical ventilation > 10 d; Significant comorbidities: Chronic kidney disease ≥ III; Cirrhosis; Dementia; Baseline neurological disease which might prohibit rehabilitation potential; Disseminated malignancy; Advanced lung disease; Uncontrolled diabetes with chronic end-organ dysfunction; Severe deconditioning; Protein-energy malnutrition; Severe peripheral vascular disease; Other preexisting life-limiting medical condition; Nonambulatory or unable to perform activities; Severe multiple organ failure; Severe acute neurologic injury (example: anoxic, stroke); Uncontrolled bleeding; Contraindications to anticoagulation; Inability to accept blood products; Ongoing cardiopulmonary resuscitation |
| V-A ECMO; Refractory cardiogenic shock; Persistent tissue hypoperfusion; Systolic blood pressure < 90 mmHg; Cardiac index < 2.2 L/min/m2 while receiving noradrenaline > 0.5 mcg/kg/min; Dobutamine > 20 mcq/kg/ min or equivalent |
The presence of hardware in the body and prolonged support such as LVAD may cause immune dysregulation, increase the risk of infection and cellular immunity impairment as prior studies had already demonstrated[47,66,73,74]. In COVID-19, severe inflammatory response might induce profound patient’s clinical status and worse outcome. The pre-existing LVAD in severe COVID-19 infection may raise some concerns in the context of management. The risk of pump thrombosis has to be kept in mind, as hypercoagulability state in COVID-19 infection and the pump itself may induce thrombosis[65]. Despite of severe hypoxemia might improve by prone position, there is a specific concern of the outflow graft compression, driveline damage and elevated pressure in the right ventricle with subsequent right ventricular failure[66,67]. Moreover, additional load to the right ventricle may predispose to right heart failure which is well known as a potential etiology of hypotension in the setting of LVAD use and inflammatory surge[66,67]. However, prone position in patients with LVADs is not contraindicated in the management of hypoxemic respiratory failure although more data are needed[3].
Anticoagulant use in LVAD patient has to be closely monitored due to a high risk of thrombosis in this population[3,14]. More interestingly, patient with COVID-19 infection may often shows a hypercoagulability state despite therapeutic dose of anticoagulation and to overcome this state, requires an increase dose which will carry the risk of life-threatening bleeding[75]. Still, thromboembolism carries a significant risk of adverse outcome and the use of closely monitored anticoagulation might have a beneficial role[55].
Several biomarkers that reflect the severity of hyperinflammation in COVID-19 might be obtained before the infection and serves as a baseline markers in patient with LVAD. Baseline lactate dehydrogenase (LDH), absolute lymphocyte count, troponin and natriuretic peptide that are taken prior the infection might bring an important information that should not be overlooked[42]. These indicators are valuable in following LVAD patients with COVID-19 infection[42]. The role of cardiopulmonary support in COVID-19 infection is illustrated in Figure 2.
As discussed above, COVID-19 infection has deleterious effect on the heart function. In addition, exaggerated inflammatory response in severe COVID-19 infection in combination with preexisting impairment of the heart function and multiple comorbid as seen in the HF patients may severely affect the outcome. Cardiac function in patient with HF should not be overlooked as deterioration of the heart function may occur rapidly as a consequence of the infection. Therefore prompt diagnosis and early monitoring of the heart function are critical in the management. Careful monitoring of inflammatory marker during the course of the disease might also play an important role, as patient with advanced HF often have their baseline checked regularly. Any elevation of the inflammatory marker might serve as a clue of worsening inflammation and the heart function.
Another thing needs to be considered is the use of anticoagulation in severe COVID-19 patients with heart failure might have beneficial effect. Hypercoagulability state is often found in the patient, it is possibly because of the inflammatory response and the implanted device that may induce coagulation. However the risk of bleeding has to be kept in mind since fluctuant international normalized ratio and overt bleeding is not uncommon[55,76-78].
The use of cardiopulmonary support in this patient remains an issue. A small subset of patients with implanted LVAD also need to be concerned as unfamiliarity of the healthcare personnel to the device and the possible manipulation of the patient’s position such as prone position might increase the right ventricular pressure and might lead to hypotension[66]. The use of ECMO and COVID-19 is very challenging due to its highly selective criteria and contraindicated in most patient with COVID-19 due to multiorgan dysfunction, significant comorbidities and the risk of bleeding[5,8].
Currently, supportive treatment remain the mainstay of treatment for COVID-19 infection. Focus is now directed on primary prevention and vaccination program. High burden and mortality rate was found in patient with preexisting cardiovascular disease, therefore American college of cardiology recommends to prioritize vaccination program in this high risk group[79].
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Indonesian Medical Association.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang MK S-Editor: Ma YJ L-Editor: A P-Editor: Liu JH
| 1. | Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global COVID-19 Thrombosis Collaborative Group; Endorsed by the ISTH, NATF, ESVM, and the IUA; Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950-2973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2178] [Cited by in RCA: 2190] [Article Influence: 438.0] [Reference Citation Analysis (0)] |
| 2. | Kabir M, Saqib MAN, Zaid M, Ahmed H, Afzal MS. COVID-19, economic impact and child mortality: A global concern. Clin Nutr. 2020;39:2322-2323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations for Heart Failure Care During the COVID-19 Pandemic. JACC Heart Fail. 2020;8:681-691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 86] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 4. | Chow J, Alhussaini A, Calvillo-Argüelles O, Billia F, Luk A. Cardiovascular Collapse in COVID-19 Infection: The Role of Venoarterial Extracorporeal Membrane Oxygenation (VA-ECMO). CJC Open. 2020;2:273-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | McLean DJ, Henry M. Con: Venoarterial ECMO Should Not Be Considered in Patients With COVID-19. J Cardiothorac Vasc Anesth. 2021;35:707-710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Dalia T, Lahan S, Ranka S, Acharya P, Gautam A, Goyal A, Mastoris I, Sauer A, Shah Z. Impact of congestive heart failure and role of cardiac biomarkers in COVID-19 patients: A systematic review and meta-analysis. Indian Heart J. 2021;73:91-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Alvarez-Garcia J, Lee S, Gupta A, Cagliostro M, Joshi AA, Rivas-Lasarte M, Contreras J, Mitter SS, LaRocca G, Tlachi P, Brunjes D, Glicksberg BS, Levin MA, Nadkarni G, Fayad Z, Fuster V, Mancini D, Lala A. Prognostic Impact of Prior Heart Failure in Patients Hospitalized With COVID-19. J Am Coll Cardiol. 2020;76:2334-2348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 151] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 8. | Bartlett RH, Ogino MT, Brodie D, McMullan DM, Lorusso R, MacLaren G, Stead CM, Rycus P, Fraser JF, Belohlavek J, Salazar L, Mehta Y, Raman L, Paden ML. Initial ELSO Guidance Document: ECMO for COVID-19 Patients with Severe Cardiopulmonary Failure. ASAIO J. 2020;66:472-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 238] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 9. | Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41:1798-1800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 464] [Cited by in RCA: 493] [Article Influence: 123.3] [Reference Citation Analysis (0)] |
| 10. | Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2352-2371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1381] [Cited by in RCA: 1366] [Article Influence: 273.2] [Reference Citation Analysis (0)] |
| 11. | Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020;5:831-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1095] [Cited by in RCA: 1249] [Article Influence: 249.8] [Reference Citation Analysis (2)] |
| 12. | Tersalvi G, Vicenzi M, Calabretta D, Biasco L, Pedrazzini G, Winterton D. Elevated Troponin in Patients With Coronavirus Disease 2019: Possible Mechanisms. J Card Fail. 2020;26:470-475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 220] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 13. | Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911-915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 608] [Cited by in RCA: 745] [Article Influence: 149.0] [Reference Citation Analysis (0)] |
| 14. | Bader F, Manla Y, Atallah B, Starling RC. Heart failure and COVID-19. Heart Fail Rev. 2021;26:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 150] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 15. | Moss N, Rakita V, Lala A, Parikh A, Roldan J, Mitter SS, Anyanwu A, Campoli M, Burkhoff D, Mancini DM. Hemodynamic Response to Exercise in Patients Supported by Continuous Flow Left Ventricular Assist Devices. JACC Heart Fail. 2020;8:291-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 16. | Lang CC, Agostoni P, Mancini DM. Prognostic significance and measurement of exercise-derived hemodynamic variables in patients with heart failure. J Card Fail. 2007;13:672-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Epidemiology Working Group for NCIP Epidemic Response; Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1341] [Reference Citation Analysis (0)] |
| 18. | Yonas E, Alwi I, Pranata R, Huang I, Lim MA, Gutierrez EJ, Yamin M, Siswanto BB, Virani SS. Effect of heart failure on the outcome of COVID-19 - A meta analysis and systematic review. Am J Emerg Med. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 19. | Riehle C, Bauersachs J. Key inflammatory mechanisms underlying heart failure. Herz. 2019;44:96-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 20. | Canepa M, Franssen FME, Olschewski H, Lainscak M, Böhm M, Tavazzi L, Rosenkranz S. Diagnostic and Therapeutic Gaps in Patients With Heart Failure and Chronic Obstructive Pulmonary Disease. JACC Heart Fail. 2019;7:823-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 21. | Vachiéry JL, Adir Y, Barberà JA, Champion H, Coghlan JG, Cottin V, De Marco T, Galiè N, Ghio S, Gibbs JS, Martinez F, Semigran M, Simonneau G, Wells A, Seeger W. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62:D100-D108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 453] [Cited by in RCA: 468] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 22. | Yasmin Kusumawardhani N, Huang I, Martanto E, Sihite TA, Nugraha ES, Prodjosoewojo S, Hamijoyo L, Hartantri Y. Lethal Arrhythmia (Torsade de Pointes) in COVID-19: An Event Synergistically Induced by Viral Associated Cardiac Injury, Hyperinflammatory Response, and Treatment Drug? Clin Med Insights Case Rep. 2020;13:1179547620972397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30114] [Article Influence: 6022.8] [Reference Citation Analysis (3)] |
| 24. | Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:811-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2516] [Cited by in RCA: 2842] [Article Influence: 568.4] [Reference Citation Analysis (0)] |
| 25. | Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2428] [Cited by in RCA: 3009] [Article Influence: 601.8] [Reference Citation Analysis (1)] |
| 26. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18196] [Article Influence: 3639.2] [Reference Citation Analysis (0)] |
| 27. | Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, De Cobelli F, Tresoldi M, Cappelletti AM, Basso C, Godino C, Esposito A. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J. 2020;41:1861-1862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 325] [Cited by in RCA: 406] [Article Influence: 81.2] [Reference Citation Analysis (0)] |
| 28. | Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res. 2020;126:1456-1474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1325] [Cited by in RCA: 1376] [Article Influence: 275.2] [Reference Citation Analysis (0)] |
| 29. | Liu PP, Blet A, Smyth D, Li H. The Science Underlying COVID-19: Implications for the Cardiovascular System. Circulation. 2020;142:68-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 509] [Cited by in RCA: 587] [Article Influence: 117.4] [Reference Citation Analysis (0)] |
| 30. | Kim IC, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020;41:1859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 229] [Cited by in RCA: 247] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 31. | Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1111] [Cited by in RCA: 1270] [Article Influence: 254.0] [Reference Citation Analysis (0)] |
| 32. | Wenzel P, Kopp S, Göbel S, Jansen T, Geyer M, Hahn F, Kreitner KF, Escher F, Schultheiss HP, Münzel T. Evidence of SARS-CoV-2 mRNA in endomyocardial biopsies of patients with clinically suspected myocarditis tested negative for COVID-19 in nasopharyngeal swab. Cardiovasc Res. 2020;116:1661-1663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 86] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 33. | Escher F, Pietsch H, Aleshcheva G, Bock T, Baumeier C, Elsaesser A, Wenzel P, Hamm C, Westenfeld R, Schultheiss M, Gross U, Morawietz L, Schultheiss HP. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail. 2020;7:2440-2447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 171] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 34. | Giustino G, Pinney SP, Lala A, Reddy VY, Johnston-Cox HA, Mechanick JI, Halperin JL, Fuster V. Coronavirus and Cardiovascular Disease, Myocardial Injury, and Arrhythmia: JACC Focus Seminar. J Am Coll Cardiol. 2020;76:2011-2023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 159] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 35. | Kochav SM, Coromilas E, Nalbandian A, Ranard LS, Gupta A, Chung MK, Gopinathannair R, Biviano AB, Garan H, Wan EY. Cardiac Arrhythmias in COVID-19 Infection. Circ Arrhythm Electrophysiol. 2020;13:e008719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 36. | Vrtovec B, Delgado R, Zewail A, Thomas CD, Richartz BM, Radovancevic B. Prolonged QTc interval and high B-type natriuretic peptide levels together predict mortality in patients with advanced heart failure. Circulation. 2003;107:1764-1769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 158] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 37. | Geleris J, Sun Y, Platt J, Zucker J, Baldwin M, Hripcsak G, Labella A, Manson DK, Kubin C, Barr RG, Sobieszczyk ME, Schluger NW. Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19. N Engl J Med. 2020;382:2411-2418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1226] [Cited by in RCA: 1153] [Article Influence: 230.6] [Reference Citation Analysis (0)] |
| 38. | Rosenberg ES, Dufort EM, Udo T, Wilberschied LA, Kumar J, Tesoriero J, Weinberg P, Kirkwood J, Muse A, DeHovitz J, Blog DS, Hutton B, Holtgrave DR, Zucker HA. Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA. 2020;323:2493-2502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 840] [Cited by in RCA: 794] [Article Influence: 158.8] [Reference Citation Analysis (0)] |
| 39. | Link MG, Yan GX, Kowey PR. Evaluation of toxicity for heart failure therapeutics: studying effects on the QT interval. Circ Heart Fail. 2010;3:547-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 40. | Tisdale JE, Jaynes HA, Kingery JR, Mourad NA, Trujillo TN, Overholser BR, Kovacs RJ. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6:479-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 259] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 41. |
Tufan A, Avanoğlu Güler A, Matucci-Cerinic M.
COVID-19, immune system response, hyperinflammation and repurposing antirheumatic drugs |
| 42. | Chau VQ, Oliveros E, Mahmood K, Singhvi A, Lala A, Moss N, Gidwani U, Mancini DM, Pinney SP, Parikh A. The Imperfect Cytokine Storm: Severe COVID-19 With ARDS in a Patient on Durable LVAD Support. JACC Case Rep. 2020;2:1315-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 43. | Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020;39:405-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1169] [Cited by in RCA: 1122] [Article Influence: 224.4] [Reference Citation Analysis (0)] |
| 44. | Aukrust P, Ueland T, Lien E, Bendtzen K, Müller F, Andreassen AK, Nordøy I, Aass H, Espevik T, Simonsen S, Frøland SS, Gullestad L. Cytokine network in congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1999;83:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 340] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 45. | Torre-Amione G, Kapadia S, Benedict C, Oral H, Young JB, Mann DL. Proinflammatory cytokine levels in patients with depressed left ventricular ejection fraction: a report from the Studies of Left Ventricular Dysfunction (SOLVD). J Am Coll Cardiol. 1996;27:1201-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 849] [Cited by in RCA: 855] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 46. | Deswal A, Petersen NJ, Feldman AM, Young JB, White BG, Mann DL. Cytokines and cytokine receptors in advanced heart failure: an analysis of the cytokine database from the Vesnarinone trial (VEST). Circulation. 2001;103:2055-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 711] [Cited by in RCA: 749] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 47. | Radley G, Pieper IL, Ali S, Bhatti F, Thornton CA. The Inflammatory Response to Ventricular Assist Devices. Front Immunol. 2018;9:2651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 48. | Silberstein M. Correlation between premorbid IL-6 Levels and COVID-19 mortality: Potential role for Vitamin D. Int Immunopharmacol. 2020;88:106995. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 49. | Mikami T, Miyashita H, Yamada T, Harrington M, Steinberg D, Dunn A, Siau E. Risk Factors for Mortality in Patients with COVID-19 in New York City. J Gen Intern Med. 2021;36:17-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 137] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 50. | Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, Amanullah A. Myocardial injury and COVID-19: Possible mechanisms. Life Sci. 2020;253:117723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 308] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 51. | Nan J, Jin YB, Myo Y, Zhang G. Hypoxia in acute cardiac injury of coronavirus disease 2019: lesson learned from pathological studies. J Geriatr Cardiol. 2020;17:221-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 52. | Rali AS, Ranka S, Shah Z, Sauer AJ. Mechanisms of Myocardial Injury in Coronavirus Disease 2019. Card Fail Rev. 2020;6:e15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 53. | Adeghate EA, Eid N, Singh J. Mechanisms of COVID-19-induced heart failure: a short review. Heart Fail Rev. 2021;26:363-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 54. | Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020;41:1858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 423] [Cited by in RCA: 474] [Article Influence: 94.8] [Reference Citation Analysis (0)] |
| 55. | Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of Coronavirus Disease 2019. Crit Care Med. 2020;48:1358-1364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 361] [Cited by in RCA: 350] [Article Influence: 70.0] [Reference Citation Analysis (0)] |
| 56. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18875] [Article Influence: 3775.0] [Reference Citation Analysis (7)] |
| 57. | Kowalewski M, Fina D, Słomka A, Raffa GM, Martucci G, Lo Coco V, De Piero ME, Ranucci M, Suwalski P, Lorusso R. COVID-19 and ECMO: the interplay between coagulation and inflammation-a narrative review. Crit Care. 2020;24:205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 58. | Permana H, Huang I, Purwiga A, Kusumawardhani NY, Sihite TA, Martanto E, Wisaksana R, Soetedjo NNM. In-hospital use of statins is associated with a reduced risk of mortality in coronavirus-2019 (COVID-19): systematic review and meta-analysis. Pharmacol Rep. 2021;73:769-780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 59. | Levy JH, Sniecinski RM, Welsby IJ, Levi M. Antithrombin: anti-inflammatory properties and clinical applications. Thromb Haemost. 2016;115:712-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 60. | Hendren NS, Drazner MH, Bozkurt B, Cooper LT Jr. Description and Proposed Management of the Acute COVID-19 Cardiovascular Syndrome. Circulation. 2020;141:1903-1914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 395] [Cited by in RCA: 405] [Article Influence: 81.0] [Reference Citation Analysis (0)] |
| 61. | Park JF, Banerjee S, Umar S. In the eye of the storm: the right ventricle in COVID-19. Pulm Circ. 2020;10:2045894020936660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 62. | Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani L, Schwartz A, Uriel N. COVID-19 and Cardiovascular Disease. Circulation. 2020;141:1648-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1022] [Cited by in RCA: 1220] [Article Influence: 244.0] [Reference Citation Analysis (0)] |
| 63. | Goldhaber SZ. Venous Thromboembolism in Heart Failure Patients: Pathophysiology, Predictability, Prevention. J Am Coll Cardiol. 2020;75:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 64. | Fanola CL, Norby FL, Shah AM, Chang PP, Lutsey PL, Rosamond WD, Cushman M, Folsom AR. Incident Heart Failure and Long-Term Risk for Venous Thromboembolism. J Am Coll Cardiol. 2020;75:148-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 65. | Rassaf T, Totzeck M, Mahabadi AA, Hendgen-Cotta U, Korste S, Settelmeier S, Luedike P, Dittmer U, Herbstreit F, Brenner T, Klingel K, Hasenberg M, Walkenfort B, Gunzer M, Schlosser T, Weymann A, Kamler M, Schmack B, Ruhparwar A. Ventricular assist device for a coronavirus disease 2019-affected heart. ESC Heart Fail. 2021;8:162-166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 66. | Singh R, Domenico C, Rao SD, Urgo K, Prenner SB, Wald JW, Atluri P, Birati EY. Novel Coronavirus Disease 2019 in a Patient on Durable Left Ventricular Assist Device Support. J Card Fail. 2020;26:438-439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 67. | Sobol I, Yuzefpolskaya M, Roth Z, Colombo PC, Horn E, Takeda K, Sayer G, Uriel N, Naka Y. Characteristics and Outcomes of Patients With a Left Ventricular Assist Device With Coronavirus Disease-19. J Card Fail. 2020;26:895-897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 68. | Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, Forel JM, Guérin C, Jaber S, Mekontso-Dessap A, Mercat A, Richard JC, Roux D, Vieillard-Baron A, Faure H. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 292] [Cited by in RCA: 466] [Article Influence: 77.7] [Reference Citation Analysis (0)] |
| 69. | Thompson BT, Chambers RC, Liu KD. Acute Respiratory Distress Syndrome. N Engl J Med. 2017;377:1904-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 102] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 70. | Hardin CC, Hibbert K. ECMO for Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2018;379:1092-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 71. | Goligher EC, Tomlinson G, Hajage D, Wijeysundera DN, Fan E, Jüni P, Brodie D, Slutsky AS, Combes A. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome and Posterior Probability of Mortality Benefit in a Post Hoc Bayesian Analysis of a Randomized Clinical Trial. JAMA. 2018;320:2251-2259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 363] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 72. | Bunge JJH, Caliskan K, Gommers D, Reis Miranda D. Right ventricular dysfunction during acute respiratory distress syndrome and veno-venous extracorporeal membrane oxygenation. J Thorac Dis. 2018;10:S674-S682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 73. | Ankersmit HJ, Tugulea S, Spanier T, Weinberg AD, Artrip JH, Burke EM, Flannery M, Mancini D, Rose EA, Edwards NM, Oz MC, Itescu S. Activation-induced T-cell death and immune dysfunction after implantation of left-ventricular assist device. Lancet. 1999;354:550-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 150] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 74. | Kimball PM, Flattery M, McDougan F, Kasirajan V. Cellular immunity impaired among patients on left ventricular assist device for 6 mo. Ann Thorac Surg. 2008;85:1656-1661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 75. | Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. JAMA. 2020;324:799-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 589] [Article Influence: 117.8] [Reference Citation Analysis (0)] |
| 76. | Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023-1026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1289] [Cited by in RCA: 1312] [Article Influence: 262.4] [Reference Citation Analysis (0)] |
| 77. | Ortega-Paz L, Capodanno D, Montalescot G, Angiolillo DJ. Coronavirus Disease 2019-Associated Thrombosis and Coagulopathy: Review of the Pathophysiological Characteristics and Implications for Antithrombotic Management. J Am Heart Assoc. 2021;10:e019650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 109] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 78. | Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094-1099. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2447] [Cited by in RCA: 2509] [Article Influence: 501.8] [Reference Citation Analysis (1)] |
| 79. | Driggin E, Maddox TM, Ferdinand KC, Kirkpatrick JN, Ky B, Morris AA, Mullen JB, Parikh SA, Philbin DM Jr, Vaduganathan M. ACC Health Policy Statement on Cardiovascular Disease Considerations for COVID-19 Vaccine Prioritization: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77:1938-1948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |