Published online Jun 26, 2021. doi: 10.4330/wjc.v13.i6.177
Peer-review started: December 9, 2020
First decision: February 28, 2021
Revised: March 8, 2021
Accepted: March 31, 2021
Article in press: March 31, 2021
Published online: June 26, 2021
Processing time: 194 Days and 20.6 Hours
Coronary artery perforation is a rare but potentially life-threatening complication of percutaneous coronary intervention (PCI), however if recognized and managed promptly, its adverse consequences can be minimized. Risk factors include the use of advanced PCI technique (such as atherectomy and chronic total occlusion interventions) and treatment of severely calcified lesions. Large vessel perforation is usually treated with implantation of a covered stent, whereas distal and collateral vessel perforations are usually treated with embolization of coils, fat, thrombin, or collagen. We describe a novel and cost-effective method of embolisation using a cut remnant of a used angioplasty balloon that was successful in sealing a distal wire perforation. we advocate this method as a simple method of managing distal vessel perforation.
A 73-year-old male with previous coronary Bypass graft operation and recurrent angina on minimal exertion had undergone rotablation and PCI to his dominant left circumflex. At the end of the procedure there was evidence of wire perforation at the distal branch and despite prolonged balloon tamponade there continued to be extravasation and the decision was made to seal this perforation. A cut piece of an angioplasty balloon was used and delivered on the original angioplasty wire to before the perforation area and released which resulted in sealing of the perforation with no unwanted clinical consequences.
The use of a balloon remnant for embolization in coronary perforation presents a simple, efficient and cost-effective method for managing coronary perforations and may be an alternative for achieving hemostasis and preventing poor outcome. Prevention remains the most important part with meticulous attention to the distal wire position, particularly with hydrophilic wires.
Core Tip: The use of a remnant balloon for sealing a coronary perforation can be a cost-effective method of treating this complication using a readily available material. In cases where the sealing of the perforation is indicated, a careful and controlled approach for delivering the balloon remnant will ensure the safe and effective delivery and the sealing of the perforation which in turn will help stabilize and safe the patient by controlling any further bleeding.
- Citation: Abdalwahab A, McQuillan C, Farag M, Egred M. Novel economic treatment for coronary wire perforation: A case report. World J Cardiol 2021; 13(6): 177-182
- URL: https://www.wjgnet.com/1949-8462/full/v13/i6/177.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i6.177
The use of a balloon remnant for embolization in coronary perforation presents a simple, efficient and cost-effective method for managing coronary perforations and may be an alternative for achieving hemostasis and preventing poor outcome. Prevention remains the most important part with meticulous attention to the distal wire position, particularly with hydrophilic wires.
A 73-year-old male presented with recurrent angina on minimal exertion with poor functional capacity despite optimal medical treatment.
He suffered with recurrent angina for 3 mo before the procedure.
He has a history of previous coronary artery bypass grafting 16 years earlier, bronchiectasis, chronic kidney disease, Barrett's esophagus and hypertension.
No family history of ischemic heart disease.
Within normal limits.
Blood tests were normal.
Echocardiogram showed normal left ventricular function. He underwent coronary angiography which showed patent left internal mammary artery graft to left anterior descending artery (LAD), patent saphenous vein graft to right coronary artery (RCA), occluded LAD and RCA, severe long and calcific lesion in proximal to mid co-dominant left circumflex artery (LCX) with no visualized patent graft.
The final diagnosis of the presented case is distal wire coronary artery perforation sealed with an embolized cut angioplasty balloon.
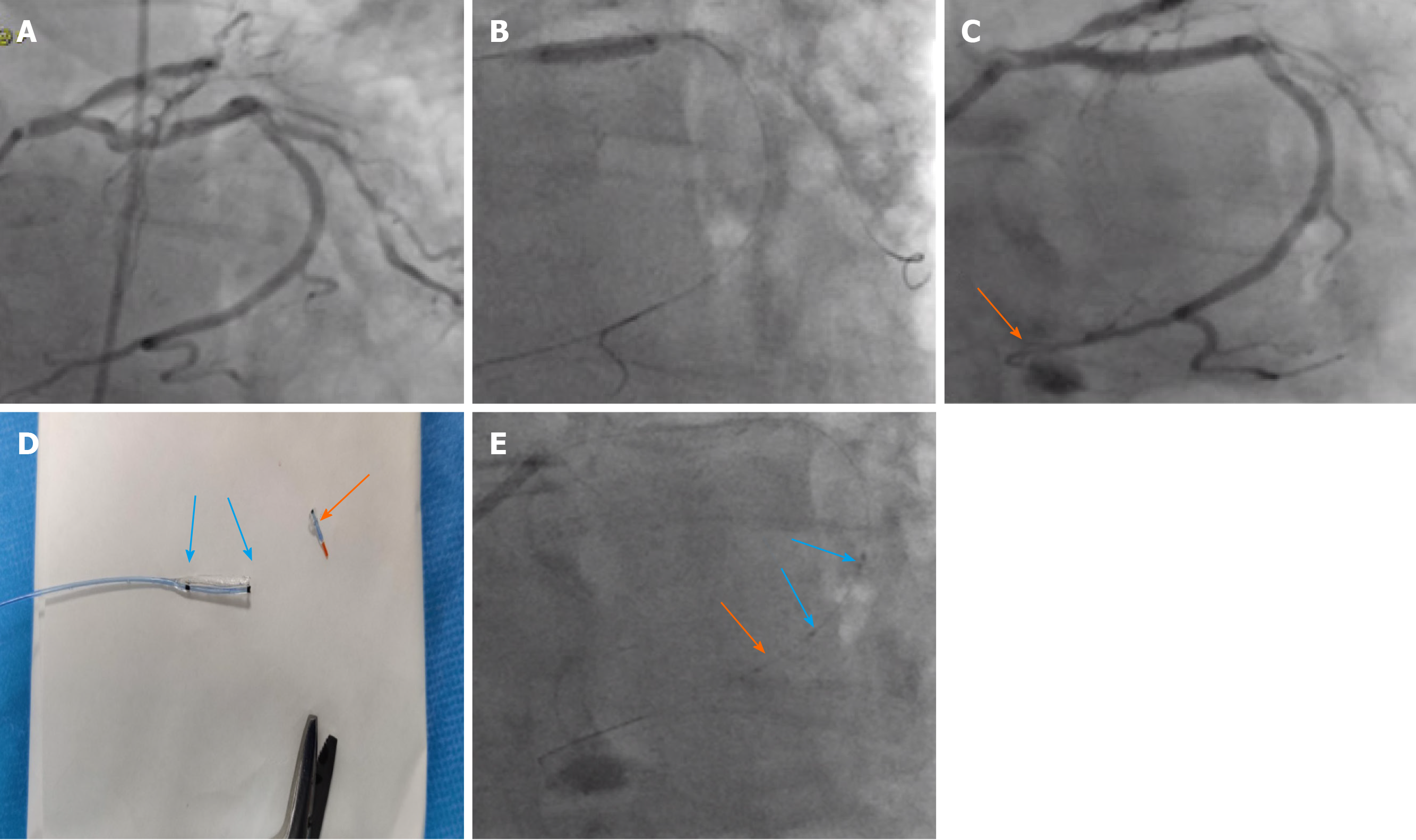
The procedure was performed from the right radial artery with planned rotablation. The proximal LCX was wired with a Gladius wire to the distal left posterior descending artery (LPDA) (Figure 1A). A Turnpike microcatheter was advanced over the Gladius wire and the wire exchanged for an extra-support rotablation wire. Rotablation was then performed with 1.25 mm then 1.75 mm burrs then a Sion black introduced with subsequent predilatation with 3.5 mm non-compliant balloon (Figure 1B). Following on a synergy drug eluting stent (DES) 4.0 mm × 24 mm was deployed and post dilated with 4.5 mm non-compliant balloon with excellent results (Figure 1C).
There was evidence of contrast staining and extravasation distally in the LPDA territory which appeared as a wire perforation. There was no evidence of hemody
A prolonged inflation of 2.0 mm balloon distally just before the site of perforation failed to stop the extravasation. Echocardiogram showed no evidence of tamponade.
At this stage, coil delivery was planned however and instead of delivering a coil, the operator thought that any compatible particle that can be delivered and block the distal artery should be helpful. The distal tip of the already used 2.0 mm balloon was cut (Figure 1D) and mounted on to the wire in the LPDA and then pushed with another intact balloon to the distal LPDA (Figure 1E) just before the perforation area then the wire and the pushing balloon were removed. There was no evidence of any further increase in the contrast staining. The OM branch was treated with 2 DES with excellent final angiographic results.
The patient had an uneventful postoperative clinical course and he was allowed home in a stable condition. He was doing well and asymptomatic on follow up 3 mo later.
Coronary perforations (large, distal, and collateral vessels) remain relatively rare[1,2], but have potentially increased with the higher use of adjunctive devices in calcified lesions[3-6]. Immediate recognition and rapid action will help prevent potential catastrophic outcome[3,7]. The balloon part, as was used in this case, is readily available and would substitute expensive equipment, and requires no specific expertise.
Rapid and clear management algorithms should be adopted. The first step is balloon tamponade with a 1/1 ratio for 5-10 min proximal or at the site of perforation. Repeated 5-10 min balloon inflation can be done till either successful sealing of the perforation or evidence of significant ischemia. Intravenous fluids and vasopressor may be needed and beneficial on occasions. Echocardiogram is important to rule out cardiac tamponade where pericardiocentesis should be performed immediately. X-Ray Fluoroscopy can show pericardial collection as the dye escapes into the pericardium. In our experience, pericardiocentesis can be performed under fluoroscopy using the pericardial dye collection as a guide without the use of echocardiography.
Furthermore, follow up echo is crucial especially in wire induced perforation as delayed pericardial effusion can occur hours later.
A crucial aspect of this complication is anticoagulation reversal which seems to be put forward as a first step approach. Perforation is a mechanical problem and reversal of anticoagulation will not solve it. It is not recommended to reverse anticoagulation as a first approach and should only be considered once the perforation is sealed and equipment removed from the coronary arteries. This is important to avoid any intracoronary thrombosis. The reversal is usually accomplished by protamine sulphate and occasionally with platelets transfusion[6].
More specific treatment lines may be needed if the previous measures were unsuccessful. In large vessel perforation, covered stents or occasionally even surgery may be needed[8]. Due to their bulkiness, deployment of covered stent may be difficult or may fail in tortuous and small vessels. In addition, these covered stents can also be used in the management of distal perforation by deployment across the side branch ostium. In distal vessel perforation, embolization or deployment of a covered stent across the ostium of the perforated branch to occlude it from the origin can be used[9].
Distal embolization can be done by different materials such as subcutaneous fat, thrombin and coils[5]. In addition, less commonly methods have been used such as injection of fibrin or synthetic glue through the lumen of microcatheter or an over-the-wire balloon[10]. Embolization of collagen, which is available commercially in femoral occlusion angioseal devices, can be used to occlude distal perforation[11]. Injection of polyvinyl alcohol particles through the lumen of inflated over the wire balloon has also been used to seal distal vessel perforation. Furthermore, injection of autologous blood clot or autologous subcutaneous fat particles through the micro catheter can occlude distal perforation.
The mechanism by which embolic material stop the bleeding is by the formation of artificial clot which trigger more clotting and occlude the vessel. After that, this embolic material will cause a foreign body granuloma which differs in its nature according to the embolized material.
In our case, we used part of a PCI balloon that is readily available in all PCI cases. This offers a rapid, simple and cost-effective way for managing coronary perforations.
There are several important points and cautions to be highlighted and considered.
Most wire perforations are self-contained and require no significant treatment. If the decision is made to treat, then this balloon remnant method can be considered.
It can be argued that fat embolization is cheaper and not a foreign material, but it is not as easy or straight forward to use as any other method and particularly this newly described balloon remnant method.
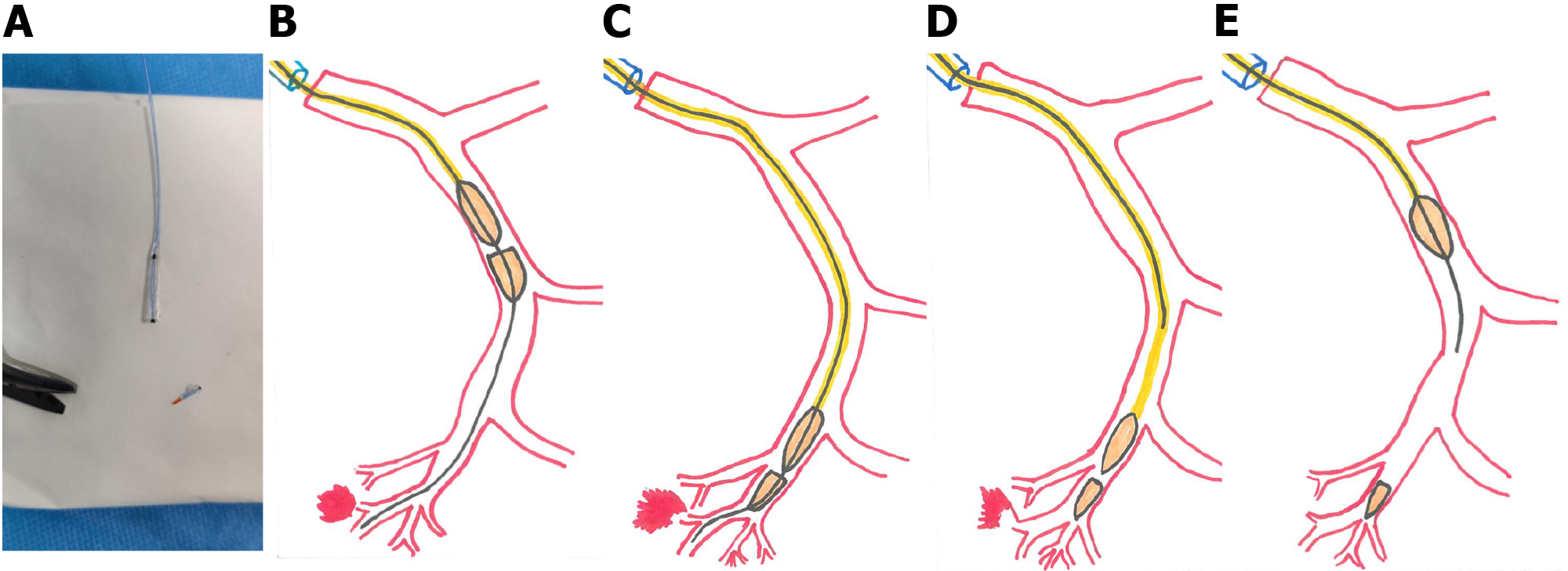
The delivery of the balloon remnant can be perceived as uncontrolled and if there is resistance and inability to deliver it, then it cannot be retrieved. Furthermore, it could also be perceived that this remnant can be advanced too distal and may exit through the perforation and cause more bleeding. This in fact is not the case. (Figure 2) The balloon remnant would be delivered after another normal balloon has passed and has been used and inflated to temporarily block the artery and stop the extravasation. This would indicate that the remnant balloon will pass too. In addition, the anatomy and the site of perforation would be clear to any experienced operator which in turn ensures that the release of the remnant is well before the perforation site itself and will have no chance of exiting through the perforation and making matters worse.
Since this case, we have used this method in a second wire perforation case that needed embolization with sealing of the perforation and excellent outcome. The patient in this case was seen in the outpatient clinic 3 mo later and he was angina free and doing well.
The use of a balloon remnant for embolization in coronary perforation presents a simple, efficient and cost-effective method for managing coronary perforations and may be an alternative for achieving hemostasis and preventing poor outcome. Prevention remains the most important part with meticulous attention to the distal wire position, particularly with hydrophilic wires.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: British Cardiac Interventional Society; European Society of Cardiology; European Association of Percutaneous Coronary Interventions; and British Cardiac Society.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Seto AH S-Editor: Fan JR L-Editor: A P-Editor: Wang LL
| 1. | Kinnaird T, Kwok CS, Kontopantelis E, Ossei-Gerning N, Ludman P, deBelder M, Anderson R, Mamas MA; British Cardiovascular Intervention Society and the National Institute for Cardiovascular Outcomes Research. Incidence, Determinants, and Outcomes of Coronary Perforation During Percutaneous Coronary Intervention in the United Kingdom Between 2006 and 2013: An Analysis of 527 121 Cases From the British Cardiovascular Intervention Society Database. Circ Cardiovasc Interv. 2016;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 2. | Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NL, Cowley MJ, Raymond RE, Safian RD, Whitlow PL. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994;90:2725-2730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 466] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 3. | Abdalwahab A, Farag M, Brilakis ES, Galassi AR, Egred M. Management of coronary artery perforation. Cardiovasc Revasc Med. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Kiernan TJ, Yan BP, Ruggiero N, Eisenberg JD, Bernal J, Cubeddu RJ, Witzke C, Don C, Cruz-Gonzalez I, Rosenfield K, Pomersantev E, Palacios I. Coronary artery perforations in the contemporary interventional era. J Interv Cardiol. 2009;22:350-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Klein LW. Coronary artery perforation during interventional procedures. Catheter Cardiovasc Interv. 2006;68:713-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Xenogiannis I, Brilakis ES. Advances in the treatment of coronary perforations. Catheter Cardiovasc Interv. 2019;93:921-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Teis A, Fernández-Nofrerías E, Rodríguez-Leor O, Tizón H, Salvatella N, Valle V, Mauri J. Coronary artery perforation by intracoronary guide wires: risk factors and clinical outcomes. Rev Esp Cardiol. 2010;63:730-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Lemmert ME, van Bommel RJ, Diletti R, Wilschut JM, de Jaegere PP, Zijlstra F, Daemen J, Van Mieghem NM. Clinical Characteristics and Management of Coronary Artery Perforations: A Single-Center 11-Year Experience and Practical Overview. J Am Heart Assoc. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Sandoval Y, Lobo AS, Brilakis ES. Covered stent implantation through a single 8-french guide catheter for the management of a distal coronary perforation. Catheter Cardiovasc Interv. 2017;90:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Goel PK. Delayed and repeated cardiac tamponade following microleak in RCA successfully treated with intra arterial sterile glue injection. Catheter Cardiovasc Interv. 2009;73:797-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Aleong G, Jimenez-Quevedo P, Alfonso F. Collagen embolization for the successful treatment of a distal coronary artery perforation. Catheter Cardiovasc Interv. 2009;73:332-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |