Published online Jun 26, 2021. doi: 10.4330/wjc.v13.i6.170
Peer-review started: March 11, 2021
First decision: March 31, 2021
Revised: April 3, 2021
Accepted: May 21, 2021
Article in press: May 21, 2021
Published online: June 26, 2021
Processing time: 103 Days and 2.8 Hours
Cardiogenic shock in the setting of acute myocardial infarction (AMI) carries significant morbidity and mortality, despite advances in pharmacological, mechanical and reperfusion therapies. Studies suggest that there is evidence of sex disparities in the risk profile, management, and outcomes of cardiogenic shock complicating AMI. Compared with men, women tend to have more comorbi
Core Tip: Sex disparities exist among different cardiovascular diseases and therapies. Cardiogenic shock is a leading cause of death among patients with acute myocardial infarction. Although some studies suggest that cardiogenic shock is more prevalent among women, women are less likely to receive guideline-recommended management including revascularization, which might explain why are more likely to experience worse outcomes.
- Citation: Bukhari S, Fatima S, Elgendy IY. Cardiogenic shock in the setting of acute myocardial infarction: Another area of sex disparity? World J Cardiol 2021; 13(6): 170-176
- URL: https://www.wjgnet.com/1949-8462/full/v13/i6/170.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i6.170
Acute myocardial infarction (AMI) is the one of the leading causes of death in the United States and worldwide[1]. In recent years, there has been a decline in the incidence and case fatality of AMI, which is partly attributed to the advancements in management including timely reperfusion and medical therapies[2,3]. Despite these improvements, sex disparity still has an impact on AMI management and outcomes[3].
Cardiogenic shock is the most common cause of death in patients with AMI, resulting from left ventricular pump failure or as a consequence of post-MI mechanical complications such as papillary muscle rupture, ventricular septal rupture, free wall rupture or right ventricular failure[4,5]. Cardiogenic shock affects 5%-10% of AMI cases and is associated with high mortality (up to 30%-40%), despite advances in pharmacological, mechanical and reperfusion endeavors[6,7]. Similar to AMI without cardiogenic shock, sex differences exist in management and outcomes among those with cardiogenic shock[8]. In this review, we discuss the sex disparities in the risk profile, management, and outcomes of cardiogenic shock in the setting of AMI, and present few solutions to the existing challenges.
Women with AMI tend to have a higher cardiovascular risk profile on presentation, as they are likely older and have a higher prevalence of traditional cardiovascular risk factors such as hypertension, diabetes, hyperlipidemia, and obesity, compared with men[9,10]. Women also have greater variability in symptom presentation, since they often present with fatigue, dyspnea, dizziness, nausea, and upper back pain, while men usually complain of chest pain and diaphoresis[11]. This difference in presen
Some studies have suggested that cardiogenic shock in the setting of AMI occurs more frequently among women[9,15,16]. For example, data from the French Registry of acute ST-elevation or non-ST-elevation myocardial infarction (FAST-MI), that included > 10000 patients between 1995 and 2010, showed that the rate of cardiogenic shock was significantly higher among women compared with men (8.2% vs 4.8%; P < 0.001)[9]. Female sex was independently associated with an increased risk of developing car
Similar to AMI without cardiogenic shock, women with cardiogenic shock tend to have a higher cardiovascular risk profile than men. Women usually have a higher co-morbidity burden including hypertension, diabetes, hyperlipidemia, and metabolic syndrome[9,16]. Women are less likely to have a history of prior MI, percutaneous coronary intervention (PCI) or coronary artery bypass graft[15]. These findings have also been observed even among younger patients. An analysis of the National Inpatient Sample (NIS) (the largest inpatient administrative database in the United States) of AMI complicated by cardiogenic shock admissions aged 18-55 years, between 2000 to 2017, found that younger women also tend to have higher burden of comorbidities[17]. Table 1 summarizes the studies comparing the prevalence and risk profile between women and men.
| Ref. | Country | Prevalence of cardiogenic shock (%) | Mean age, yr | Hypertension (%) | Diabetes (%) | Prior myocardial infarction (%) | Prior percutaneous coronary intervention (%) | Smoking (%) | |||||||
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | ||
| Isorni et al[9] | France | 4.8 | 8.2 | 68.9 | 80.2 | 57 | 80 | 31 | 44 | 21 | 18.5 | 21 | 13 | 25 | 7 |
| Koeth et al[15] | Germany | 9.3 | 12.9 | 68 | 76.3 | 37 | 45.3 | 25.2 | 39.1 | 25.6 | 19.9 | 13.2 | 6.7 | 36 | 17.9 |
| Abdel-Qadir et al[16] | Canada | 2.7 | 3.7 | 71.1 | 75.5 | NA | NA | 24.4 | 26.9 | NA | NA | NA | NA | NA | NA |
| Vallabhajosyula et al[8] | United States | NA | NA | 82 | 83.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Vallabhajosyula et al[17] | United States | NA | NA | 48.8 | 48.3 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Wong et al[19] | United States, Canada | NA | NA | 66.8 | 71.4 | 45.6 | 62.1 | 28.3 | 40.8 | 44.7 | 32 | 7.6 | 5.1 | 57.5 | 40.7 |
| Fengler et al[20] | Germany | NA | NA | 68 | 74 | 66 | 76 | 29 | 40 | 25 | 16 | 31 | 15 | 39 | 25 |
| Gimenez et al[21] | Switzerland, Germany, Poland, Austria, France, Italy | NA | NA | 67 | 75 | 58.3 | 66.7 | 30.3 | 39.4 | 18.5 | 11.3 | 20.2 | 14.4 | 29 | 18.1 |
Timely reperfusion remains the cornerstone in the management of AMI complicated by cardiogenic shock[18]. Studies examining AMI complicated by cardiogenic shock reveal that significant sex-based differences still exist. In an analysis of the NIS database, including > 134000 older (≥ 75 years) patients who were hospitalized between 2000 and 2014, women were less likely to undergo coronary angiography (55.4% vs 49.2%; P < 0.001), PCI (36.3% vs 34.4%; P < 0.001), and receive mechanical circulatory support devices (34.3% vs 27.2%; P < 0.001) compared with men[8]. Similar results were reflected in another NIS analysis of younger adults (18-55 years), which showed that women less frequently received coronary angiography (78.3% vs 81.4%), early coronary angiography (defined as angiography performed on the day of admission) (49.2% vs 54.1%), PCI (59.2% vs 64.0%), and mechanical circulatory support devices (50.3% vs 59.2%; all P < 0.001) compared with younger men[17]. The Canadian-based Ontorio Myocardial Infarction Database also showed that women were less likely to be revascularized (12.6% vs 17.6%; P < 0.001) and less likely to be transferred when they presented to non-revascularization sites (11.3% vs 14.2%; P < 0.001)[16].
Notably, some sex disparities were observed in randomized trials of interventions for patients with cardiogenic shock in the setting of AMI. An exploratory analysis of the Should we emergently revascularize occluded coronaries for cardiogenic shock? (SHOCK) trial of 1190 patients showed that although the rates of thrombolytic treatment, PCI and surgical revascularization were not different between both sexes, intra-aortic balloon pump (IABP) use was less frequent among women (48% vs 55%; P = 0.05), despite exhibiting lower cardiac index[19]. In another trial, Intra-aortic Balloon Pump in Cardiogenic Shock II (IABP-SHOCK II) that included 600 patients under
| Studies | Percutaneous coronary intervention (%) | Coronary artery bypass graft (%) | Mechanical circulatory support (%) | |||
| Men | Women | Men | Women | Men | Women | |
| Isorni et al[9] | 76.5 | 68.5 | NA | NA | NA | NA |
| Koeth et al[15] | 18 | 11 | NA | NA | NA | NA |
| Abdel-Qadir et al[16] | 14 | 10.6 | 4.3 | 2.3 | NA | NA |
| Vallabhajosyula et al[8] | 36.3 | 34.4 | 12 | 8.1 | 34.3 | 27.2 |
| Vallabhajosyula et al[17] | 64 | 59.2 | 20.1 | 18.3 | 59.2 | 50.3 |
| Wong et al[19] | 31.1 | 35.4 | 17.3 | 12.1 | 55.2 | 48.1 |
| Fengler et al[20] | 96.6 | 94.1 | 0.7 | 1.6 | 52 | 48 |
| Gimenez et al[21] | 100 | 100 | - | - | 28.6 | 27.2 |
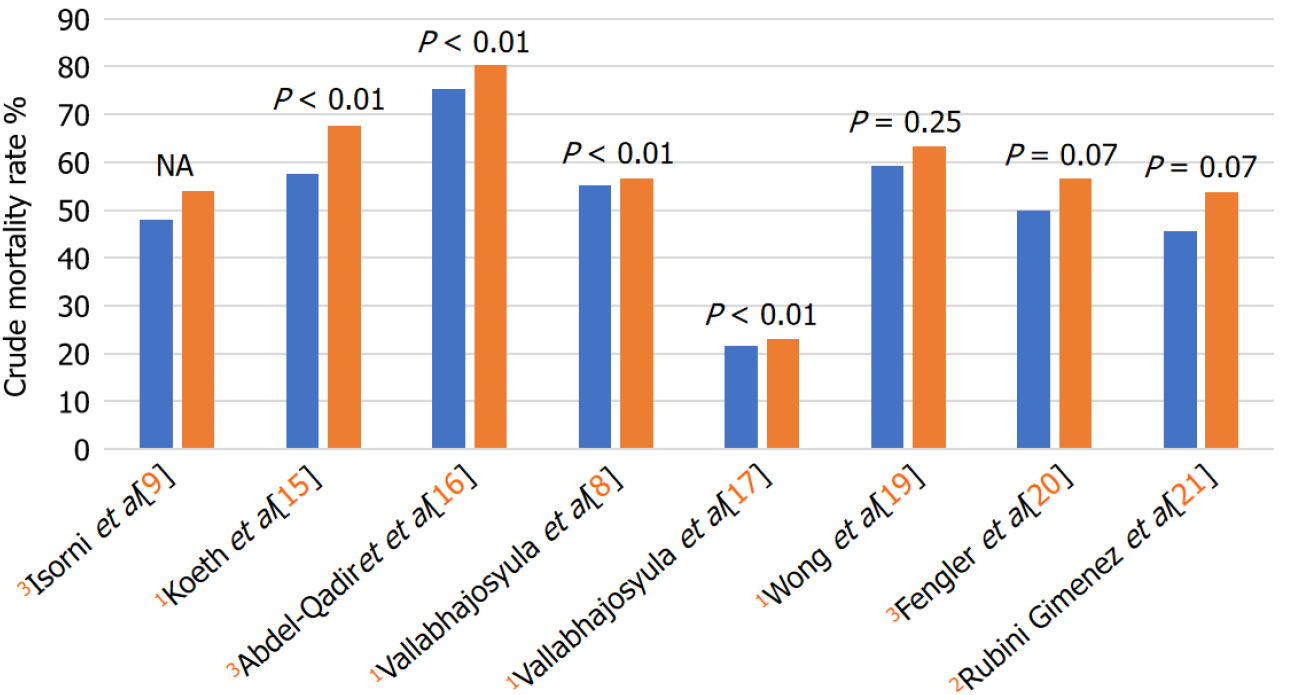
Many studies have indicated that women have higher unadjusted mortality rates compared with men, primarily explained by older age, higher co-morbidity burden and lower likelihood of receiving reperfusion therapy and mechanical circulatory support devices. Data from the NIS database for older patients (≥ 75 years) revealed that despite a steady decrease in in-hospital mortality during the study period between 2000 and 2014, adjusted trends showed consistently higher in-hospital mortality among women compared with men[8]. Female sex remained an independent predictor of higher in-hospital mortality (adjusted OR 1.05; 95%CI: 1.02-1.08; P < 0.001)[8]. Similarly, NIS data for younger patients (18-55 years) also showed that women experienced higher hospital mortality, and that female sex was an independent predictor of in-hospital mortality (adjusted OR 1.11, 95%CI: 1.07-1.16; P < 0.001)[17] (Figure 1). The timely use of reperfusion strategies could potentially improve survival among women. For example, data from the French FAST-MI registry showed that although 1-year mortality was significantly decreased for both men and women due to primary PCI, primary PCI was an independent predictor of 1-year survival among women (hazard ratio [HR] 0.55, 95%CI: 0.37-0.81), but not men (HR 0.85, 95%CI: 0.61-1.19)[9]. Although these studies showed that women were less likely to receive reperfusion therapy and mechanical circulatory support devices, data about the angiographic findings and other clinical variables were not available in these studies.
Secondary analyses of randomized trials of cardiogenic shock in the setting of AMI have also suggested that there was no difference in treatment effect based on sex[19-21]. As such, these findings support the notion that women should be treated similar to men (i.e. timely reperfusion, and consideration of mechanical circulatory support devices if indicated). Noteworthy, despite the higher prevalence of cardiogenic shock among women in many studies, women have consistently been underrepresented in these interventional trials. While women in the SHOCK and IABP-SHOCK-II trials comprised 32% and 31% of the participants, respectively, women constituted only 24% of the study population in the CULPRIT SHOCK trial that was conducted about 2 decades later.
Sex-based differences exist in the clinical presentation of AMI and might subsequently result in treatment delays. Women often present late and with non-classical symptoms of AMI and thus are often misdiagnosed resulting in delays in care, and potentially preventable adverse outcomes. This highlights the importance of using objective measures of risk stratification among patients with suspected AMI. Minimizing provider bias together with focusing on educating women at risk about the symptoms of AMI warrant priority.
With regards to clinical trials pertinent to cardiogenic shock in the setting of AMI, women continue to be underrepresented despite a higher incidence of cardiogenic shock among women in many studies. Clinical trials form the foundation for guide
Women, despite having higher comorbidity and varied symptom manifestation, derive similar benefit with guideline-directed management as men. This important message needs to be translated into action and reflected in our clinical practice, where unfortunately women are seen more often to be misdiagnosed and undertreated than men, resulting in worse outcomes. In the real world, there is a need to identify and address individual-based and system-based factors that trigger unconscious biases and impede the provision of high-quality and equitable healthcare irrespective of the sex differences. Since women with AMI have a higher cardiovascular risk profile and sometimes delayed presentations than men, clinicians are encouraged to keep a lower threshold for initiating work-up for diagnosis, and institute prompt delivery of care and employ aggressive treatment strategies when indicated.
In the meantime, there is a need to increase awareness among women to identify symptoms, and to seek immediate care. It is essential to emphasize both primary and secondary preventative strategies that are appropriate for women from numerous backgrounds, and could be applicable in various clinical settings. The foremost step towards personalized medicine involves paying attention to sex-specific details and recognizing sex-disparity in the clinical settings, which will help improve awareness, diagnosis, treatment and eventually outcomes in women.
Cardiogenic shock is the leading cause of death among AMI patients. Sex disparity in the management and outcomes of patients with cardiogenic shock in the setting of AMI exist. Although some studies indicate that cardiogenic shock occurs more frequently among women, women do not receive adequate management as evidenced by the lower rates compared of revascularization and mechanical circulatory support devices. Given these differences, women continue to experience worse outcomes. Future studies are needed to understand the reasons behind these differences and efforts are needed to minimize these disparities.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tung TH S-Editor: Liu M L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143:e254-e743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3854] [Cited by in RCA: 3598] [Article Influence: 899.5] [Reference Citation Analysis (0)] |
| 2. | Reynolds K, Go AS, Leong TK, Boudreau DM, Cassidy-Bushrow AE, Fortmann SP, Goldberg RJ, Gurwitz JH, Magid DJ, Margolis KL, McNeal CJ, Newton KM, Novotny R, Quesenberry CP Jr, Rosamond WD, Smith DH, VanWormer JJ, Vupputuri S, Waring SC, Williams MS, Sidney S. Trends in Incidence of Hospitalized Acute Myocardial Infarction in the Cardiovascular Research Network (CVRN). Am J Med. 2017;130:317-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Pedersen F, Butrymovich V, Kelbæk H, Wachtell K, Helqvist S, Kastrup J, Holmvang L, Clemmensen P, Engstrøm T, Grande P, Saunamäki K, Jørgensen E. Short- and long-term cause of death in patients treated with primary PCI for STEMI. J Am Coll Cardiol. 2014;64:2101-2108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 312] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 4. | Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, Jain D, Gotsis W, Ahmed A, Frishman WH, Fonarow GC. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc. 2014;3:e000590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 463] [Cited by in RCA: 458] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 5. | Elbadawi A, Elgendy IY, Mahmoud K, Barakat AF, Mentias A, Mohamed AH, Ogunbayo GO, Megaly M, Saad M, Omer MA, Paniagua D, Abbott JD, Jneid H. Temporal Trends and Outcomes of Mechanical Complications in Patients With Acute Myocardial Infarction. JACC Cardiovasc Interv. 2019;12:1825-1836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 207] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 6. | Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM. Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med. 1999;340:1162-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 378] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 7. | Wayangankar SA, Bangalore S, McCoy LA, Jneid H, Latif F, Karrowni W, Charitakis K, Feldman DN, Dakik HA, Mauri L, Peterson ED, Messenger J, Roe M, Mukherjee D, Klein A. Temporal Trends and Outcomes of Patients Undergoing Percutaneous Coronary Interventions for Cardiogenic Shock in the Setting of Acute Myocardial Infarction: A Report From the CathPCI Registry. JACC Cardiovasc Interv. 2016;9:341-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 204] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 8. | Vallabhajosyula S, Vallabhajosyula S, Dunlay SM, Hayes SN, Best PJM, Brenes-Salazar JA, Lerman A, Gersh BJ, Jaffe AS, Bell MR, Holmes DR Jr, Barsness GW. Sex and Gender Disparities in the Management and Outcomes of Acute Myocardial Infarction-Cardiogenic Shock in Older Adults. Mayo Clin Proc. 2020;95:1916-1927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 9. | Isorni MA, Aissaoui N, Angoulvant D, Bonello L, Lemesle G, Delmas C, Henry P, Schiele F, Ferrières J, Simon T, Danchin N, Puymirat É; FAST-MI investigators. Temporal trends in clinical characteristics and management according to sex in patients with cardiogenic shock after acute myocardial infarction: The FAST-MI programme. Arch Cardiovasc Dis. 2018;111:555-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L; Get With the Guidelines Steering Committee and Investigators. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803-2810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 418] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 11. | Brush JE Jr, Krumholz HM, Greene EJ, Dreyer RP. Sex Differences in Symptom Phenotypes Among Patients With Acute Myocardial Infarction. Circ Cardiovasc Qual Outcomes. 2020;13:e005948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, Griffith JL, Selker HP. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342:1163-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1327] [Cited by in RCA: 1228] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 13. | Arora S, Stouffer GA, Kucharska-Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, Caughey MC. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation. 2019;139:1047-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 488] [Article Influence: 81.3] [Reference Citation Analysis (0)] |
| 14. | Mehilli J, Kastrati A, Dirschinger J, Pache J, Seyfarth M, Blasini R, Hall D, Neumann FJ, Schömig A. Sex-based analysis of outcome in patients with acute myocardial infarction treated predominantly with percutaneous coronary intervention. JAMA. 2002;287:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 111] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Koeth O, Zahn R, Heer T, Bauer T, Juenger C, Klein B, Gitt AK, Senges J, Zeymer U. Gender differences in patients with acute ST-elevation myocardial infarction complicated by cardiogenic shock. Clin Res Cardiol. 2009;98:781-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Abdel-Qadir HM, Ivanov J, Austin PC, Tu JV, Džavík V. Sex differences in the management and outcomes of Ontario patients with cardiogenic shock complicating acute myocardial infarction. Can J Cardiol. 2013;29:691-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Vallabhajosyula S, Ya'Qoub L, Singh M, Bell MR, Gulati R, Cheungpasitporn W, Sundaragiri PR, Miller VM, Jaffe AS, Gersh BJ, Holmes DR Jr, Barsness GW. Sex Disparities in the Management and Outcomes of Cardiogenic Shock Complicating Acute Myocardial Infarction in the Young. Circ Heart Fail. 2020;13:e007154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 18. | Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Ting HH, O'Gara PT, Kushner FG, Ascheim DD, Brindis RG, Casey DE Jr, Chung MK, de Lemos JA, Diercks DB, Fang JC, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2016;67:1235-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 509] [Cited by in RCA: 610] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 19. | Wong SC, Sleeper LA, Monrad ES, Menegus MA, Palazzo A, Dzavik V, Jacobs A, Jiang X, Hochman JS; SHOCK Investigators. Absence of gender differences in clinical outcomes in patients with cardiogenic shock complicating acute myocardial infarction. A report from the SHOCK Trial Registry. J Am Coll Cardiol. 2001;38:1395-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Fengler K, Fuernau G, Desch S, Eitel I, Neumann FJ, Olbrich HG, de Waha A, de Waha S, Richardt G, Hennersdorf M, Empen K, Hambrecht R, Fuhrmann J, Böhm M, Poess J, Strasser R, Schneider S, Schuler G, Werdan K, Zeymer U, Thiele H. Gender differences in patients with cardiogenic shock complicating myocardial infarction: a substudy of the IABP-SHOCK II-trial. Clin Res Cardiol. 2015;104:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 21. | Rubini Gimenez M, Zeymer U, Desch S, de Waha-Thiele S, Ouarrak T, Poess J, Meyer-Saraei R, Schneider S, Fuernau G, Stepinska J, Huber K, Windecker S, Montalescot G, Savonitto S, Jeger RV, Thiele H. Sex-Specific Management in Patients With Acute Myocardial Infarction and Cardiogenic Shock: A Substudy of the CULPRIT-SHOCK Trial. Circ Cardiovasc Interv. 2020;13:e008537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 22. | Elgendy IY, Van Spall HGC, Mamas MA. Cardiogenic Shock in the Setting of Acute Myocardial Infarction: History Repeating Itself? Circ Cardiovasc Interv. 2020;13:e009034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |