Published online Apr 26, 2021. doi: 10.4330/wjc.v13.i4.95
Peer-review started: December 13, 2020
First decision: February 28, 2021
Revised: March 8, 2021
Accepted: March 22, 2021
Article in press: March 22, 2021
Published online: April 26, 2021
Processing time: 128 Days and 10.9 Hours
We performed a meta-analysis on observational studies since randomized control trials are not available. We studied intracoronary brachytherapy (ICBT) and recurrent drug eluting stent in-stent restenosis (DES-ISR) to evaluate the procedural success, target lesion revascularization (TLR), incidence of myocardial infarction (MI) and all-cause mortality at 2 years follow-up.
To perform meta-analysis for patients undergoing ICBT for recurrent DES-ISR.
We performed a systematic search of the PubMed/MEDLINE, Cochrane and DARE databases to identify relevant articles. Studies were excluded if intra-coronary brachytherapy was used as a treatment modality for initial ISR and studies with bare metal stents. We used a random-effect model with DerSimonian & Laird method to calculate summary estimates. Heterogeneity was assessed using I2 statistics.
A total of 6 observational studies were included in the final analysis. Procedural angiographic success following intra-coronary brachytherapy was 99.8%. Incidence of MI at 1-year was 2% and 4.1% at 2-years, respectively. The incidence of TLR 14.1% at 1-year and 22.7% at 2-years, respectively. All-cause mortality at 1- and 2-year follow-up was 3% and 7.5%, respectively.
Given the observational nature of the studies included in the analysis, heterogeneity was significantly higher for outcomes. While there are no randomized controlled trials or definitive guidelines available for recurrent ISR associated with DES, this analysis suggests that brachytherapy might be the alternative approach for recurrent DES-ISR. Randomized controlled trials are required to confirm results from this study.
Core Tip: Information is not readily available for the management of recurrent drug-eluting in-stent restenosis. There have been recent advances in the management of in-stent restenosis. While the use of a drug-eluting stent is still associated with in-stent restenosis, the use of intracoronary brachytherapy (ICBT) has resurged as one of the modalities in the management of such a complex problem. This analysis focuses on myocardial infarction and target lesion revascularization after the use of ICBT with a follow-up out to 2 years. Future studies with longer follow up are required to see if these benefits last longer.
- Citation: Ilyas I, Kumar A, Adalja D, Shariff M, Desai R, Sattar Y, Vallabhajosyula S, Gullapalli N, Doshi R. Intracoronary brachytherapy for the treatment of recurrent drug-eluting stent in-stent restenosis: A systematic review and meta-analysis. World J Cardiol 2021; 13(4): 95-102
- URL: https://www.wjgnet.com/1949-8462/full/v13/i4/95.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i4.95
As percutaneous coronary intervention has evolved, drug eluting stents (DES) have become the mainstay of therapy given their lower rates of in-stent restenosis (ISR) and other complications in comparison to bare metal stents (BMS). ISR occurs due to vascular remodeling and neointimal hyperplasia which can lead to the reoccurrence of anginal symptoms[1]. Various clinical factors, including stent type, other comorbidities and patient characteristics, contribute to the development of ISR. This makes it difficult to ascertain the exact incidence of ISR, however, with the advent of second-generation DES, ISR rates have decreased to approximately 8%[2]. Patients with ISR will often undergo revascularization with repeat stenting per guideline, however, the recommendations are less clear for 2 or more previously implanted stents[3,4]. There have been several modalities used for such lesion without clear benefits which includes but not limited to the use of laser atherectomy, intracoronary brachytherapy (ICBT), and drug coated balloons. The intracoronary irradiation may limit intravascular smooth muscle proliferation by promoting novel cell cycle regulation and eventually reduces the rate of ISR[5]. There have been promising results with the use of ICBT for recurrent DES-ISR[6-8]. Given the inherent limitations and logistic issues associated with the use of ICBT, the use has been very limited to a few centres in the United States. We performed a meta-analysis on observational studies studying ICBT in the absence of randomized controlled trials and recurrent DES-ISR to evaluate the procedural success, target lesion revascularization (TLR), incidence of myocardial infarction (MI) and all-cause mortality at 1- and 2-years follow-up.
We performed a systematic search of the PubMed/MEDLINE, Cochrane and DARE databases to identify relevant articles. The literature search was performed from the inception of the database to January 2019. Since studies included in the present meta-analysis were approved my institutional ethical committee, no additional ethical clearance was required for the present meta-analysis. The reporting of the present systematic review and meta-analysis was in accordance with the PRISMA guidelines[9].
Each of the three databases were searched using the search terms "Intra-coronary Brachytherapy", "ICBT" OR "Intra-vascular Brachytherapy" "Intravascular Brachytherapy", "Drug eluting stent", "Drug-eluting stent", DES, "In-stent restenosis", ISR, to identify citations without language restrictions (Supplementary Table 1). Studies were not excluded based on sample size. The identified studies were imported into Mendeley reference manager and checked for duplicates. The reference list of the relevant articles searched were reviewed to identify additional articles.
The inclusion criteria were (1) observational studies of ICBT; and (2) for recurrent ISR of DES reporting either one of the following event rates: Procedural success; TLR, MI and all-cause mortality at 1 and/or 2 years follow up. Studies were excluded if intra-coronary brachytherapy was used as a treatment modality for initial ISR and studies with BMS (Supplementary eMethod1).
The screening of searched citations was performed at two levels. At the first level, two reviewers independently screened the title and abstracts of citations searched. At the second level, full text of citations identified by first level of screening was reviewed by two independent reviewers and included if the studies met the inclusion criteria. Any disparity during the review process was rectified by mutual consensus. Data extraction from included studies was performed by two reviewers independently. The following information was extracted from each included study, author’s name, year, number of patients, mean age, percentage male, procedural angiographic success rates, TLR, MI and all-cause mortality rates at 1- and 2-year follow-up that were reported.
We used random effect model with DerSimonian & Laird method to calculate summary estimates. Heterogeneity was assessed using I2 statistics. Estimates with I2 > 50% was considered statistically heterogeneous. To allow for inclusion in the meta-analysis, a correction of 0.5 was added to the events of studies reporting event rate of 0%. All statistical analysis was carried out using R statistical software version 3.6.2.
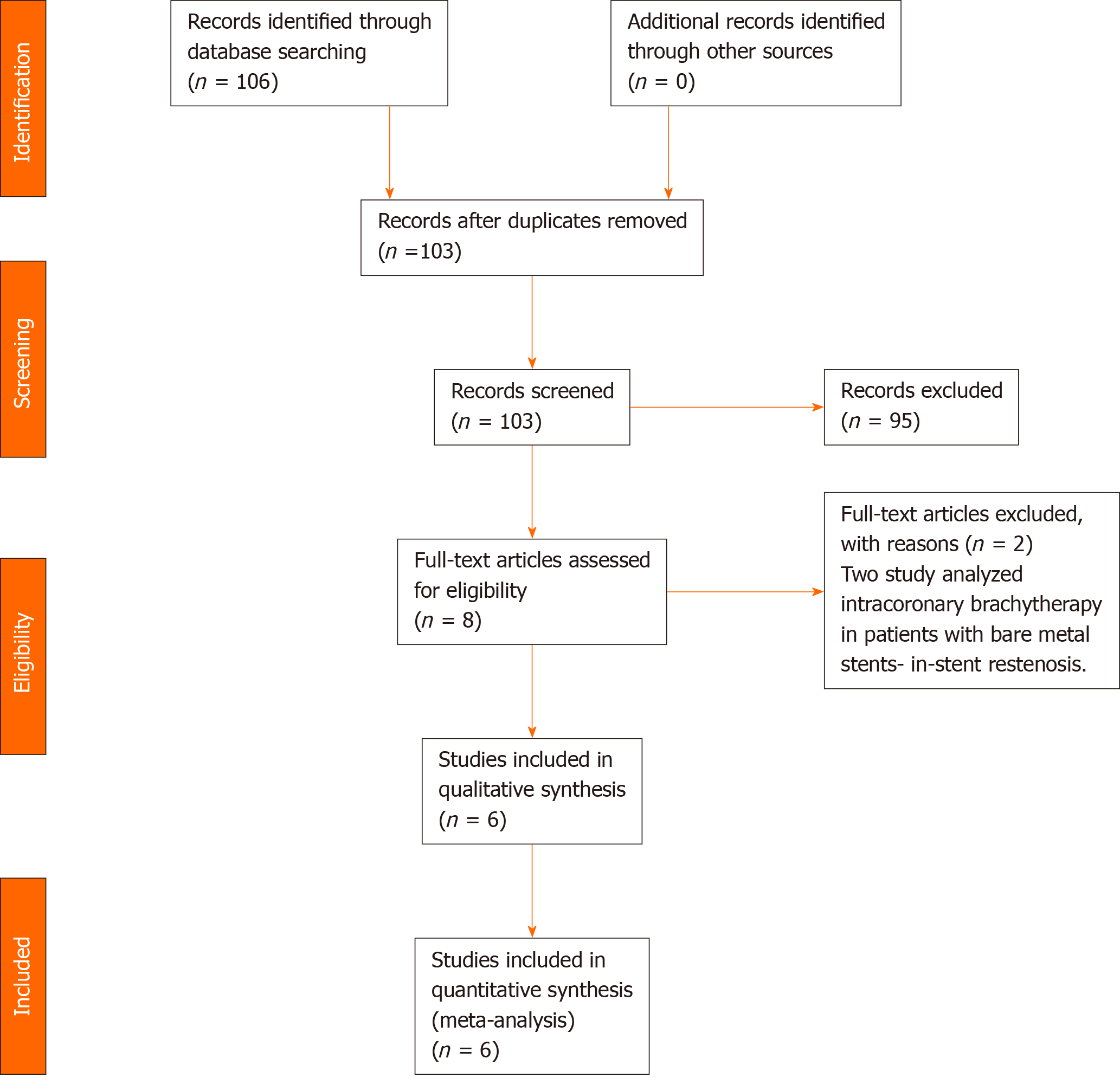
The database search identified a total of 26 citations. After applying the inclusion criteria, 6 studies were included in the final analysis[6,7,10-12]. The PRISMA flow chart for inclusion of studies is provided in Figure 1. All studies included in the present study analysed intra-coronary brachytherapy as treatment strategy in patients with recurrent ISR. The baseline characteristics of included studies are provided in Table 1. The mean age of the patients ranges from 65-67 years in all studies. All studies included patients with ≥ 2 stents. However, information regarding previous stent DES or BMS was not clear in any of the manuscript. Males were significantly higher in all studies. All studies utilized Strontium/yttrium-90 beta radiation system at the depth of 2 mm in almost all studies. Mean radiation dose was 18-23 gray in all studies. All the studies performed brachytherapy on DES as the most recent layer of the stent. Although studies did not mention which stent was utilized prior to this brachytherapy procedure, all studies included patients after calendar year 2011, and hence, we can safely assume that all studies utilized second generation DES stent after the procedure.
| Ref. | Year | Number of patients (n) | Mean age (years) | Percentage male (%) | DM (%) | Hypertension (%) | Type of brachytherapy | Mean/median radiation dose | |
| 1 | Negi et al[6] | 2016 | 186 | 65 | 62 | 47 | 95 | Strontium/yttrium-90 beta radiation | 23-25 Gray |
| 2 | Ohri et al[8] | 2016 | 134 | 65 | 75 | 59 | 99 | Strontium/yttrium-90 beta radiation | 18.4 or 23 Gray |
| 3 | Mangione et al[7] | 2017 | 101 | 66 | 67 | 53 | 98 | Strontium/yttrium-90 beta radiation | 18-23 Gray |
| 4 | Varghese et al[12] | 2018 | 197 | 65 | 75 | 60 | 99 | Strontium/yttrium-90 beta radiation | 22 Gray |
| 5 | Megaly et al[10] | 2021 | 116 | 66 | 69 | - | - | Strontium/yttrium-90 beta radiation | 22.6 Gray |
| 6 | Meraj et al[11] | 2021 | 290 | 67 | 66 | 58 | 97 | Strontium/yttrium-90 beta radiation | 23 Gray |
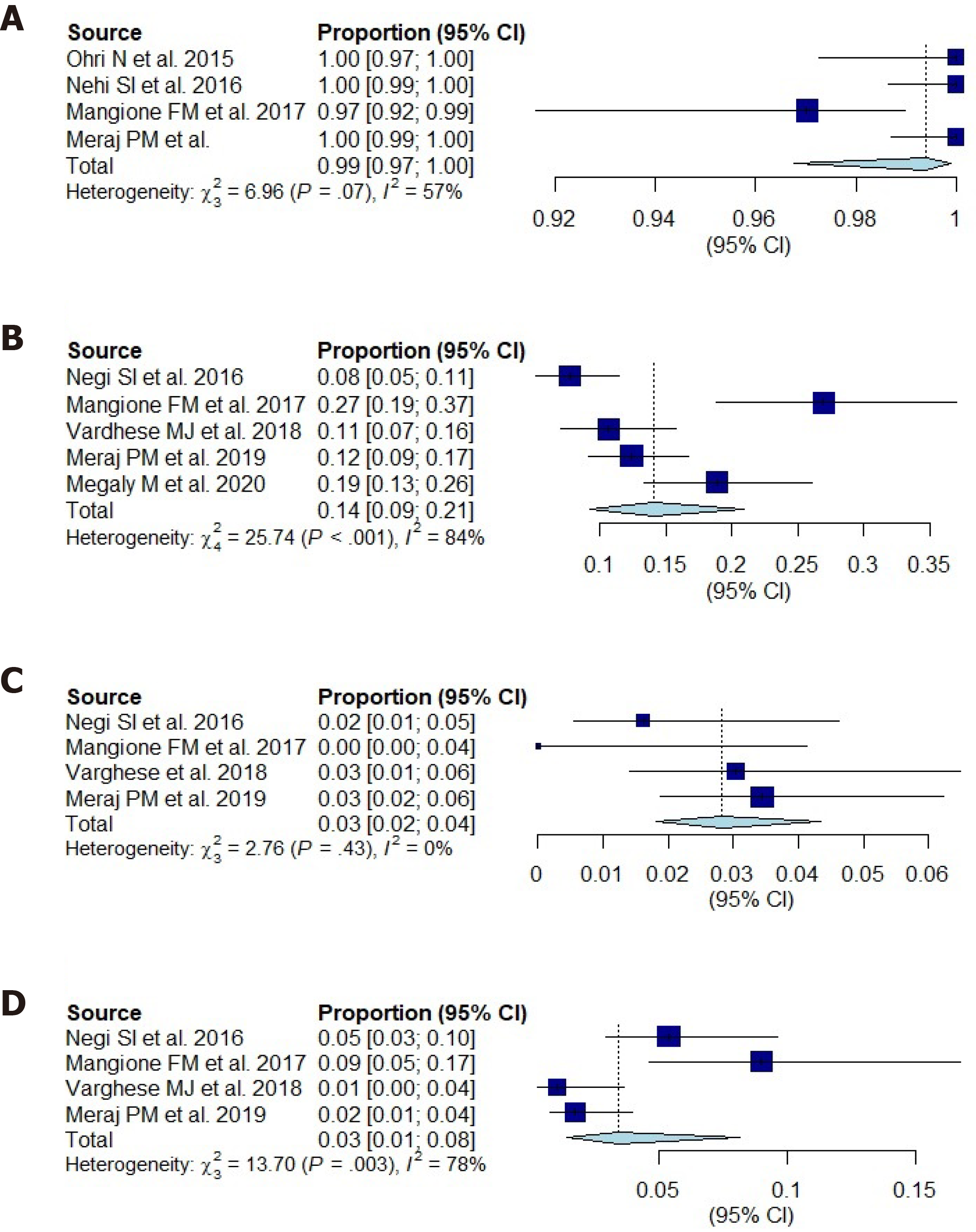
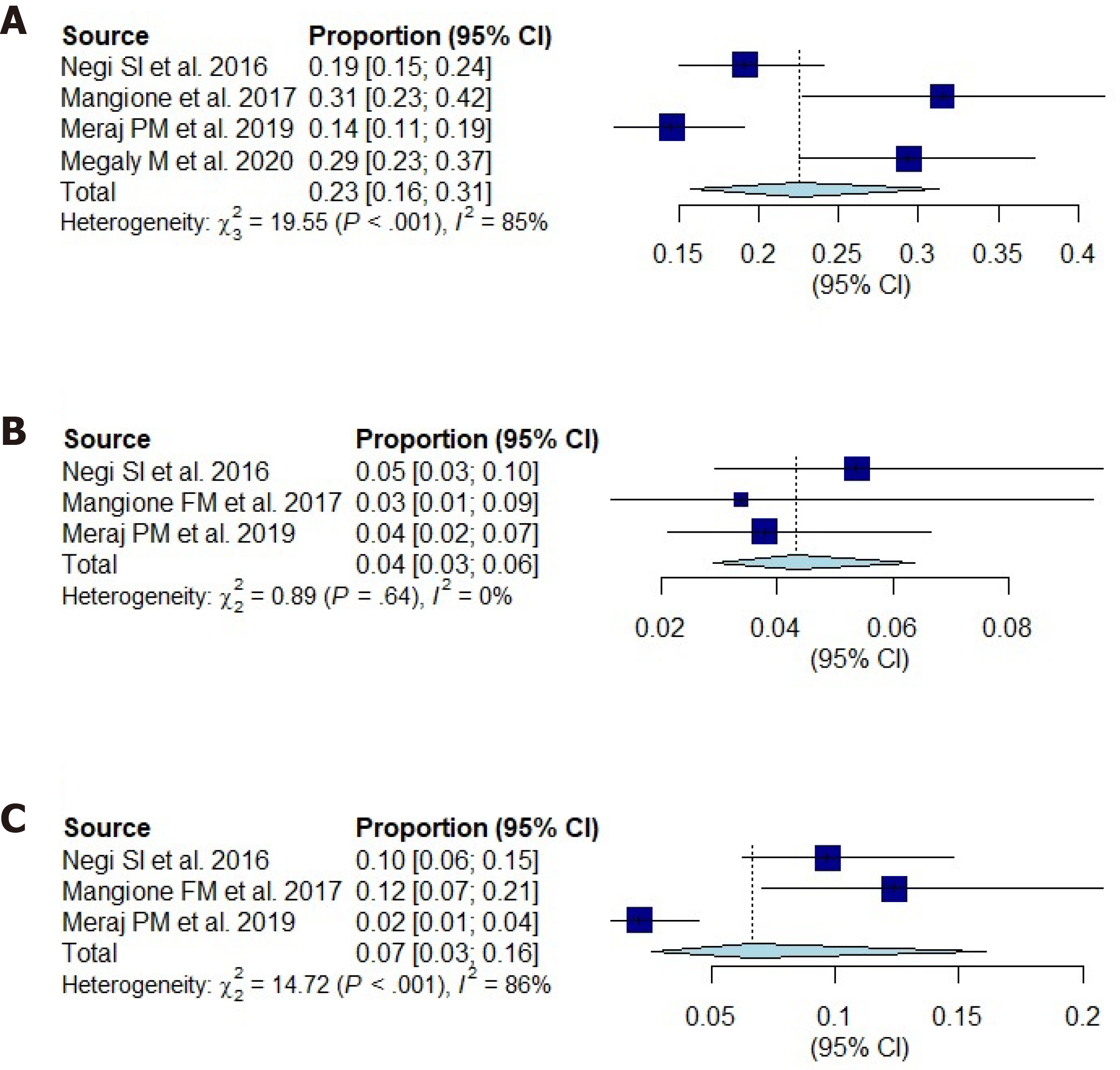
Procedural angiographic success following intra-coronary brachytherapy was 99.8% (95%CI: 99.5%-100.1%) (Figure 2A). TLR at 1-year follow-up was 14.1% (95%CI: 9.2%-19%) (Figure 2B) and at 2-year follow-up was 22.7% (95%CI: 15.4%-30%) (Figure 3A) following intra-coronary brachytherapy. MI at 1- and 2-year follow-up were 2% (95%CI: 0.6%-3.3%) and 4.1% (95%CI: 2.5%-5.8%) (Figures 2C and 3B), respectively. All-cause mortality rates were 3% (95%CI: 0.8%-5.3%) and 7.5% (95%CI: 0.8%-14.3%) (Figures 2D and 3C), at 1- and 2-year follow-up, respectively.
In the absence of randomized controlled trials, we analysed observational studies demonstrating the favourable outcomes of brachytherapy following DES-ISR. The findings demonstrate high rates of procedural success, with TLR (14.1%) at 1-year and (22.7%) at 2-years, respectively. Incidence of MI at 1-year was 2% and 4.1% at 2-years, respectively. All-cause mortality at 1- and 2-year follow-up was 3% and 7.5%, respectively.
Brachytherapy targets adventitial fibromyoblasts that is the main source for neoproliferation of the tissue and causes apoptosis. Since there is overall suppression of neointimal growth by DES, DES-ISR tends to be focal, predominantly occurring at the stent edge[13]. ICBT inhibits neointimal formation within the stent by delivering radioactive strontium-90 beta-radiation via a hydraulic mechanism. This may not be as effective at the stent edge which may account for the minority of patients requiring revascularization at the 1- and 2-year follow-up[14]. Between the 1- and 2-year marks, there has been a remarkable increase in TLR, 14.1% vs 22.7%, leading to increases in MI and all-cause mortality at the two-year mark. This suggests that radiation may delay but does not eliminate the development of restenosis, leading to higher occurrences of MI and all-cause mortality at the two-year mark.
Management of resistant DES-ISR remains challenging and the best therapeutic option is still unclear. Some experts suggested that combined use of excimer laser coronary atherectomy may improve further clinical outcomes, however, the data is limited. Another option would be to use drug coated balloons; however, more data is needed to determine use of this technology. The use of rotational and orbital atherectomy is also on the rise. As technology is growing, use of third generation DES stent would be helpful in reducing ISR rates itself. Intravascular imaging is another growing field which might help determine pathophysiology in the development of DES-ISR. Since stent under-expansion is thought to be the main reason for DES-ISR, this can probably be prevented with the use of intravascular ultrasonography.
There are some limitations to our analysis. Three of the six studies included data for all the seven endpoints we analysed. This may have led to a smaller data pool. Additionally, we did not analyse the vessel diameter of the targeted lesion as this information was not readily available. Though, it should be a matter that, it should be investigated further given that ICBT has the greatest benefit in small vessel diameters[15]. It has been previously established that patients with diabetes are more prone to develop ISR, yet it would be interesting to note the long-term procedural success in patients with co-morbid conditions following ICBT after DES-ISR[16]. The number of stent varied in different studies. With each additional layer of stent, chances of ISR and other outcomes may increase. Finally, we do not have enough randomized control trials and we have to rely on observational studies to guide management in such patients. Overall, our analysis shows that ICBT is a feasible treatment option for the treatment of DES-ISR, is associated with high rates of procedural success and favourable efficacy at the one and two-year marks.
Currently, United States Food and Drug Administration has approved intracoronary radiation as an adjunctive treatment for ISR. While there are no definitive guidelines or recommendations for the management of recurrent ISR associated with DES, this analysis on brachytherapy with DES-ISR demonstrated that ICBT could be an effective alternate modality for such complex lesions. However, heterogeneity was significantly higher given the observational nature of the studies included in the analysis which must be kept in mind. Analysis shows that the initial intra-coronary brachytherapy procedure is highly successful. Brachytherapy is a practical treatment option for difficult to treat DES-ISR in patients with limited life expectancy or multiple comorbid states who may not be able to tolerate alternative treatment options, though, further analysis is needed on the long-term effects following ICBT in medically complex patients.
There is no established strategy for the management of in-stent restenosis which is common even when using drug eluting stents. There is a resurgence of the use of intracoronary brachytherapy (ICBT) for the treatment of drug eluting stent in-stent restenosis (DES-ISR).
The use of ICBT was common in the late 1990s era. Even with the use of second and third generation drug-eluting stents, in-stent restenosis have remined a significant problem. There have been multiple strategies used to manage this complex problem. Along with other strategies, ICBT has re-emerged as a potential solution.
The main objective was to perform a meta-analysis for patients undergoing ICBT for recurrent DES-ISR and analyze clinically important outcomes.
We have reviewed PubMed/MEDLINE, Cochrane and DARE databases to identify studies that used ICBT for the management of in-stent restenosis. We used a random-effect model with DerSimonian & Laird method to calculate summary estimates. Heterogeneity was assessed using I2 statistics.
We included 6 observational studies in this meta-analysis. Procedural angiographic success following intra-coronary brachytherapy was 99.8%. The incidence of myocardial infarction and all-cause mortality was within acceptable range at 2 years. Incidence of target lesion revascularization (14.1%) at 1-year and (22.7%) at 2-years, respectively.
Brachytherapy should be one of the preferred approach for recurrent DES-ISR.
There is an unmet need for randomized control trial comparing brachytherapy vs another drug eluting stent with a longer follow-up.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ueda H S-Editor: Fan JR L-Editor: A P-Editor: Li JH
| 1. | Pleva L, Kukla P, Hlinomaz O. Treatment of coronary in-stent restenosis: a systematic review. J Geriatr Cardiol. 2018;15:173-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 33] [Reference Citation Analysis (0)] |
| 2. | Spaulding C, Daemen J, Boersma E, Cutlip DE, Serruys PW. A pooled analysis of data comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med. 2007;356:989-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 519] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 3. | Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:e574-e651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 788] [Cited by in RCA: 922] [Article Influence: 65.9] [Reference Citation Analysis (0)] |
| 4. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2722] [Cited by in RCA: 4482] [Article Influence: 896.4] [Reference Citation Analysis (0)] |
| 5. | Scott S, O'Sullivan M, Hafizi S, Shapiro LM, Bennett MR. Human vascular smooth muscle cells from restenosis or in-stent stenosis sites demonstrate enhanced responses to p53: implications for brachytherapy and drug treatment for restenosis. Circ Res. 2002;90:398-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Negi SI, Torguson R, Gai J, Kiramijyan S, Koifman E, Chan R, Randolph P, Pichard A, Satler LF, Waksman R. Intracoronary Brachytherapy for Recurrent Drug-Eluting Stent Failure. JACC Cardiovasc Interv. 2016;9:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Mangione FM, Jatene T, Badr Eslam R, Bergmark BA, Gallagher JR, Shah PB, Mauri L, Leopold JA, Sobieszczyk PS, Faxon DP, Croce KJ, Bhatt DL, Devlin PM. Usefulness of Intracoronary Brachytherapy for Patients With Resistant Drug-Eluting Stent Restenosis. Am J Cardiol. 2017;120:369-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Ohri N, Sharma S, Kini A, Baber U, Aquino M, Roy S, Sheu RD, Buckstein M, Bakst R. Intracoronary brachytherapy for in-stent restenosis of drug-eluting stents. Adv Radiat Oncol. 2016;1:4-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11206] [Cited by in RCA: 11012] [Article Influence: 688.3] [Reference Citation Analysis (0)] |
| 10. | Megaly M, Glogoza M, Xenogiannis I, Vemmou E, Nikolakopoulos I, Willson L, Monyak DJ, Sullivan P, Stanberry L, Sorajja P, Chavez I, Mooney M, Traverse J, Wang Y, Garcia S, Poulose A, Burke MN, Brilakis ES. Outcomes of intravascular brachytherapy for recurrent drug-eluting in-stent restenosis. Catheter Cardiovasc Interv. 2021;97:32-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Meraj PM, Patel K, Patel A, Doshi R, Srinivas G, Jauhar R, Kaplan B, Garzon R, Sharma A, Cao Y, Diaz Molina F, Sharma R. Northwell intracoronary brachytherapy for the treatment of recurrent drug eluting stent in-stent restenosis (NITDI study group). Catheter Cardiovasc Interv. 2021;97:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Varghese MJ, Bhatheja S, Baber U, Kezbor S, Chincholi A, Chamaria S, Buckstein M, Bakst R, Kini A, Sharma S. Intravascular Brachytherapy for the Management of Repeated Multimetal-Layered Drug-Eluting Coronary Stent Restenosis. Circ Cardiovasc Interv. 2018;11:e006832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Her AY, Shin ES. Current Management of In-Stent Restenosis. Korean Circ J. 2018;48:337-349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Mintz GS, Weissman NJ, Teirstein PS, Ellis SG, Waksman R, Russo RJ, Moussa I, Tripuraneni P, Jani S, Kobayashi Y, Giorgianni JA, Pappas C, Kuntz RA, Moses J, Leon MB. Effect of intracoronary gamma-radiation therapy on in-stent restenosis: An intravascular ultrasound analysis from the gamma-1 study. Circulation. 2000;102:2915-2918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Ajani AE, Waksman R, Cha DH, Gruberg L, Satler LF, Pichard AD, Kent KM. The impact of lesion length and reference vessel diameter on angiographic restenosis and target vessel revascularization in treating in-stent restenosis with radiation. J Am Coll Cardiol. 2002;39:1290-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Kastrati A, Schömig A, Elezi S, Schühlen H, Dirschinger J, Hadamitzky M, Wehinger A, Hausleiter J, Walter H, Neumann FJ. Predictive factors of restenosis after coronary stent placement. J Am Coll Cardiol. 1997;30:1428-1436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 478] [Article Influence: 17.1] [Reference Citation Analysis (0)] |