Published online Oct 26, 2021. doi: 10.4330/wjc.v13.i10.593
Peer-review started: January 24, 2021
First decision: February 28, 2021
Revised: March 7, 2021
Accepted: September 17, 2021
Article in press: September 17, 2021
Published online: October 26, 2021
Processing time: 269 Days and 10.3 Hours
We report a patient who was diagnosed with toxic myopericarditis secondary to hydrocarbon abuse using cardiac magnetic resonance imaging (CMR).
A 25-year-old male presented to emergency department with chest pain for 3 d. Patient also reported sniffing hydrocarbon containing inhalant for the last 1 year. Labs showed elevated troponin and electrocardiography was suggestive of acute pericarditis. Echocardiogram showed left ventricular (LV) ejection fraction (EF) of 40%. Given patient’s troponin elevation and reduced EF, cardiac catheterization was performed which showed normal coronaries. CMR was performed for myocardial infarction with non-obstructive coronary arteries evaluation. CMR showed borderline LV function with edema in mid and apical LV suggestive of myocarditis.
CMR can be used to diagnose toxic myopericarditis secondary to hydrocarbon abuse.
Core Tip: Inhalant abuse has been rampant in the United States population in the last 2 decades. Cardiac manifestations of hydrocarbon inhalant abuse are not well reported. We report a case of myopericarditis in a patient with inhalant abuse. We also describe the role of Cardiac Magnetic Resonance Imaging in diagnosis and treatment of these patients.
- Citation: Jolly G, Dacosta Davis S, Ali S, Bitterman L, Saunders A, Kazbour H, Parwani P. Cardiac involvement in hydrocarbon inhalant toxicity — role of cardiac magnetic resonance imaging: A case report. World J Cardiol 2021; 13(10): 593-598
- URL: https://www.wjgnet.com/1949-8462/full/v13/i10/593.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i10.593
Inhalant abuse has been rampant in the United States population in the last 2 decades[1,2]. Commonly used domestic and industrial items including hair spray, spot remover, PC cleaner and glues have hydrocarbon constituents like dimethyl ether and hydrofluorocarbons. We present our patient who has a longstanding history of huffing dust off, (the propellant cleaner which has difluoroethane as the active hydrocarbon ingredient) who developed myopericarditis with systolic dysfunction. We also discuss the role of Cardiac Magnetic Resonance Imaging in diagnosing and prognosticating in these patients.
Chest pain, nausea and vomiting × 3 d.
A 25-year-old male patient with no prior medical history presented to the emergency department with chest pain, nausea and vomiting × 3 d. He described sharp, intermittent chest pain that is sub sternal, radiating to the back and left arm for last 3 d. His pain is worse upon leaning forward and worse with deep inspiration. He also had multiple episodes of nausea and vomiting with an episode of coffee-ground emesis. Patient reported long-term abuse of hydrocarbon containing inhalant (PC keyboard dust off) for the last 1 year. He used to huff 2 cans of dust off at the same time to achieve a hallucinogenic effect along with marijuana use. One week prior to admission, he reported increased use (10 cans/d).
History of intracranial aneurysm rupture in father.
The patient’s heart rate was 112 bpm, respiratory rate was 15 breaths per minute, blood pressure was 114/73 mmHg and oxygen saturation on room air was 99%. His body mass index (BMI) was 37 kg/m2. Cardiac examination revealed a regular rate and rhythm, and no jugular venous distention with mild chest wall tenderness. Erythematous, non-scaling lesions were noted on the chest wall, arm and lips. Abdominal examination revealed right upper quadrant and bilateral flank tenderness.
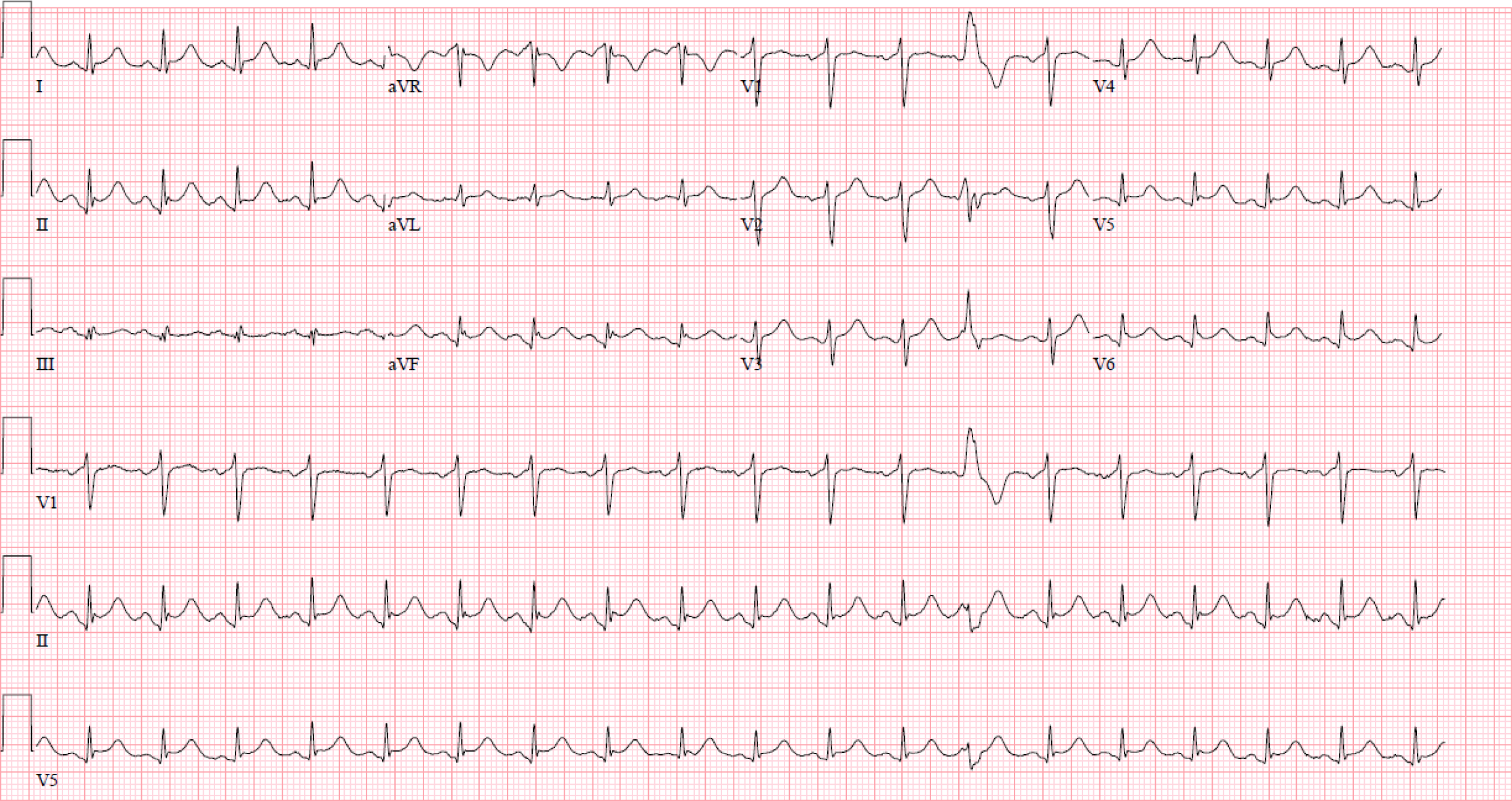
Initial laboratory evaluation showed leukocytosis (WBC-19.6 bil/L), acute kidney injury (Cr-3.4 mg/dL, BUN-54 mg/dL), elevated transaminases (AST-161 U/L, ALT-77 U/L), troponin-1.63 (ng/mL) peaked at 2.06 (ng/mL), CK-3000 ng/mL, CKMB-45 ng/mL. Urine drug screen was positive for cannabinoids. Initial electrocardiography (EKG) showed sinus tachycardia with diffuse inferolateral ST elevation, concerning for acute myopericarditis (Figure 1).
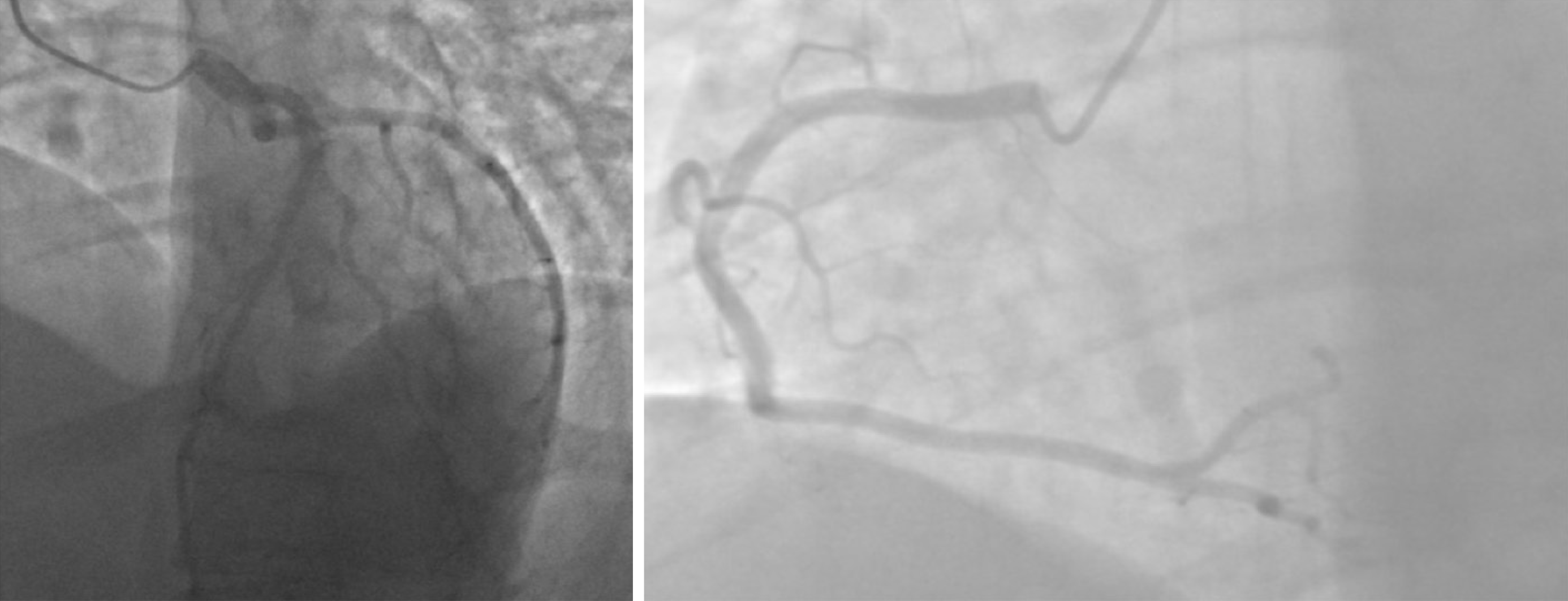
Echocardiogram showed left ventricular (LV) ejection fraction (EF) of 40% to 45% with severe aortic root dilation (5.0 cm) and trivial pericardial effusion. Given patient’s elevated troponins, cardiac catheterization was performed. Coronary angiogram showed no evidence of coronary artery disease (Figure 2). Working diagnosis of myocardial infarction with non-obstructive coronary arteries (MINOCA) was established and cardiac magnetic resonance imaging (CMR) was performed to evaluate the etiology further.
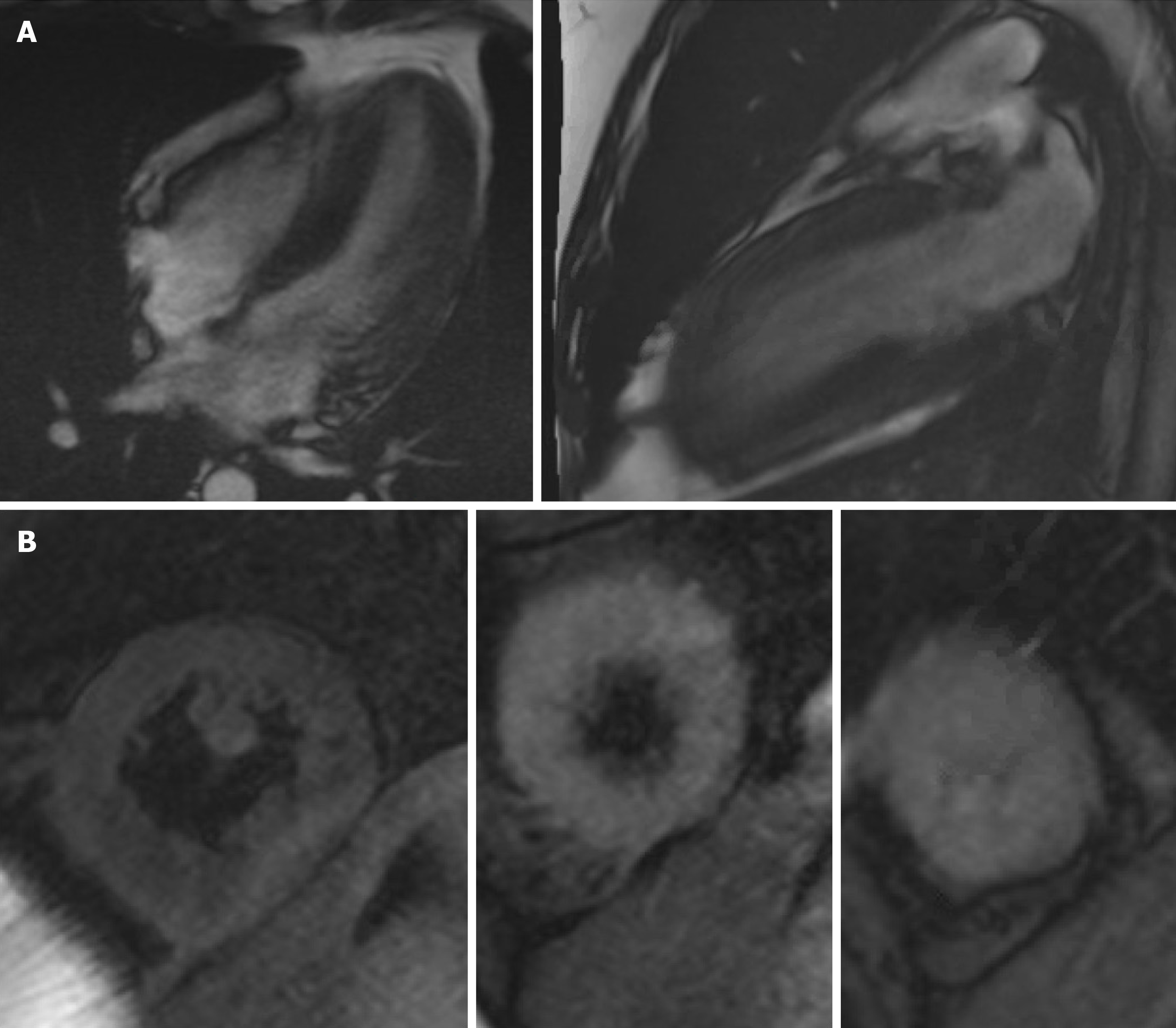
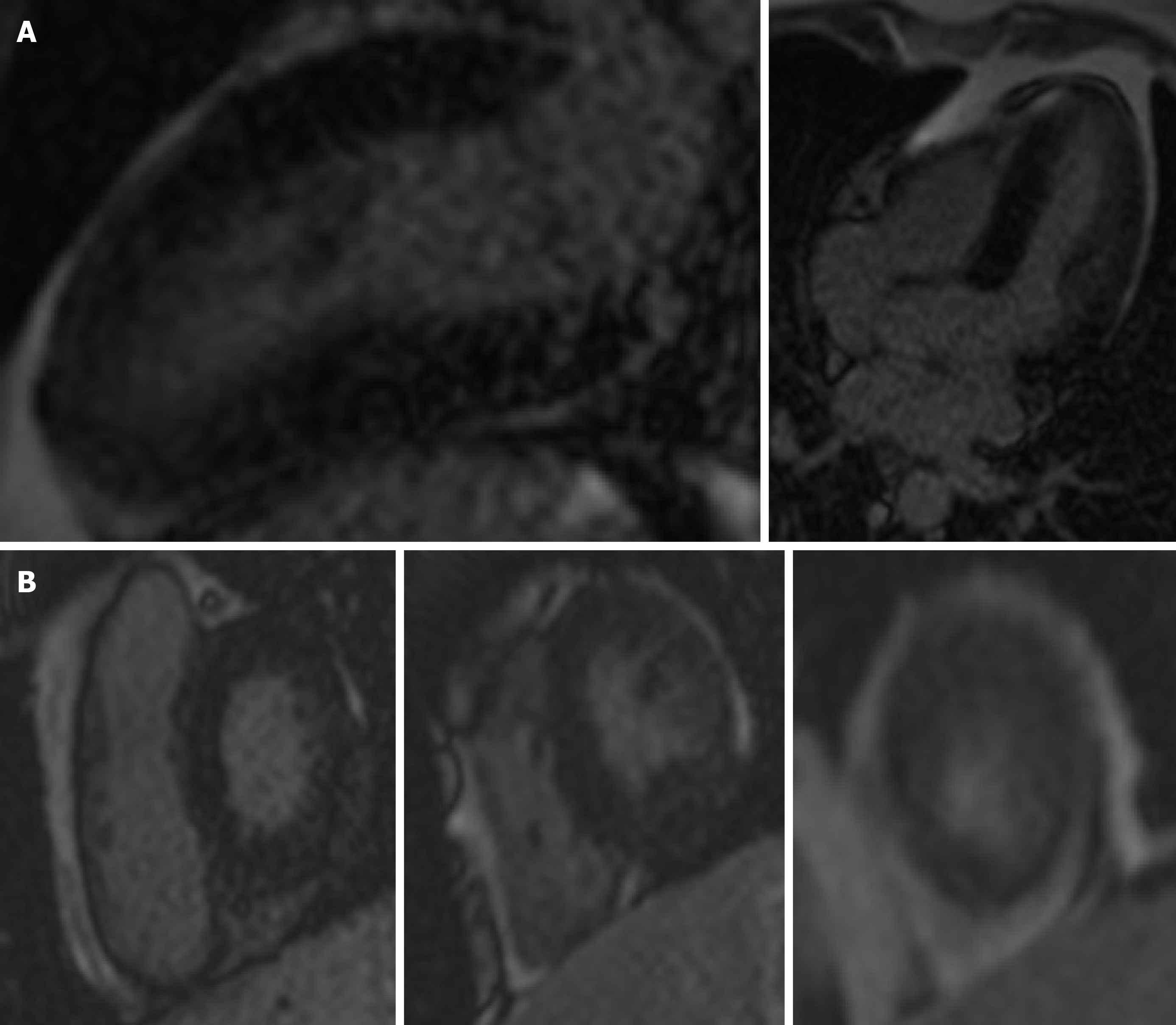
CMR showed borderline LV function with edema in the mid and apical LV suggestive of myocardial inflammation (Figure 3A and B). No delayed enhancement was seen in the myocardium or in the pericardium (Figure 4A and B). There was no evidence of pericardial effusion.
Based on the clinical presentation and imaging findings, patient was diagnosed with acute toxic myopericarditis secondary to hydrocarbon inhalant abuse. NSTEMI and MINOCA was ruled out based on coronary angiogram and CMR respectively.
Supportive management for pain control was initially initiated. Once renal function improved, colchicine 0.6 mg b.i.d. was initiated for ongoing chest pain and EKG findings.
Repeat echo obtained 6 wk after the index presentation revealed EF of 60%.
Hydrocarbon compounds have been previously reported to have multiple cardiotoxic effects. Cates and Cook[3] reported a case of severe cardiomyopathy complicated by significant reduction in EF (25%) and torsades de pointes in the patient with history of huffing dust off. Interestingly, patient in this case report, recovered normal ventricular function prior to discharge. Samson et al[4] reported a similar case of inhalant abuse with severe reduction in EF on presentation, which improved prior to discharge. Cao et al[5] reported a case of NSTEMI without significant reduction in EF in a patient with air duster huffing. This patient was noted to have significant hepatic and renal injury, similar to our patient. Life threatening arrhythmias including ventricular fibrillation causing sudden cardiac death has been reported previously[6-8]. Toxic myopericarditis have been previously diagnosed in these patients[2]. Dinsfriend et al[2] reported a case of recurrent myopericarditis diagnosed in a patient with inhalant abuse with CMR. CMR showed edema and late gadolinium enhancement (LGE) in base and mid lateral wall and in the mid anterior wall.
Myopericarditis refers to an inflammatory process affecting the pericardium and myocardium[9]. Myopericarditis is diagnosed based on clinical features defining pericardial and myocardial involvement. Diagnosis of acute pericarditis involves presence of 2 or more of the 4 criteria: Pleuritic chest pain, pericardial friction rub, suggestive ECG changes (widespread ST segment elevation, PR depression) and new or worsening pericardial effusion[10]. Myocardial involvement is defined by elevated serum cardiac enzymes levels (creatine kinase-MB fraction, or troponin I or T), or new onset of focal or diffuse reduced LV function by echocardiography in the absence of evidence of any other causes[11]. CMR can be utilized to make diagnosis of myopericarditis. CMR diagnosis of myocarditis can be made based on the modified Lake Louise criteria[12]. The three diagnostic targets proposed using this criterion include edema, hyperemia and necrosis or scar. If CMR images indicate 2 out of 3 criteria, there is a high likelihood for acute myocarditis.
We report a case of patient with diffuse ST elevations, chest pain, decreased ejection on CMR in absence of any LGE. Our patient demonstrated early CMR finding in hydrocarbon toxicity manifested predominantly by low EF and edema in absence of LGE. Our patient had BMI of 37 with high low-density lipoprotein and positive family history of CAD. We ruled out coronary artery disease by doing cardiac catheterization however given the modest troponin rise and hydrocarbon toxicity, per recent European Society of Cardiology NSTEMI guidelines and class I recommendation on role of CMR in MINOCA, CMR was performed. CMR was useful in establishing presence of edema without any LGE[13]. This finding although nonspecific, points more towards, myocardial involvement. The absence of LGE provided excellent prognostic information[14]. CMR thus was helpful in diagnosis, prognosis and treatment in this case of inhalant toxicity.
Patients with inhalant abuse can have various cardiovascular manifestations. In patients with hydrocarbon toxicity with myocarditis, CMR can provide diagnosis, prognosticate the overall illness and give treatment options.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Najafi M S-Editor: Gao CC L-Editor: A P-Editor: Li JH
| 1. | Howard MO, Bowen SE, Garland EL, Perron BE, Vaughn MG. Inhalant use and inhalant use disorders in the United States. Addict Sci Clin Pract. 2011;6:18-31. [PubMed] |
| 2. | Dinsfriend W, Rao K, Matulevicius S. Inhalant-Abuse Myocarditis Diagnosed by Cardiac Magnetic Resonance. Tex Heart Inst J. 2016;43:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Cates AL, Cook MD. Severe Cardiomyopathy after Huffing Dust-Off™. Case Rep Emerg Med. 2016;2016:9204790. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Samson R, Kado H, Chapman D. Huffing-induced cardiomyopathy: a case report. Cardiovasc Toxicol. 2012;12:90-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Cao SA, Ray M, Klebanov N. Air Duster Inhalant Abuse Causing Non-ST Elevation Myocardial Infarction. Cureus. 2020;12:e8402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Sakai K, Maruyama-Maebashi K, Takatsu A, Fukui K, Nagai T, Aoyagi M, Ochiai E, Iwadate K. Sudden death involving inhalation of 1,1-difluoroethane (HFC-152a) with spray cleaner: three case reports. Forensic Sci Int. 2011;206:e58-e61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Avella J, Wilson JC, Lehrer M. Fatal cardiac arrhythmia after repeated exposure to 1,1-difluoroethane (DFE). Am J Forensic Med Pathol. 2006;27:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. |
Ouali S, Guermazi O, Guermazi F, Halima MB, Boudiche S, Khedher N, Meghaieth F, Farhati A, Larbi N, Mourali MS.
Drug Abuse-Induced Cardiac Arrhythmias: Mechanisms and Management, Cardiac Arrhythmias, Umashankar Lakshmanadoss, |
| 9. | Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K, Linhart A, Maisch B, McKenna W, Mogensen J, Pinto YM, Ristic A, Schultheiss HP, Seggewiss H, Tavazzi L, Thiene G, Yilmaz A, Charron P, Elliott PM; European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636-2648, 2648a. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 2261] [Article Influence: 188.4] [Reference Citation Analysis (0)] |
| 10. | Imazio M, Spodick DH, Brucato A, Trinchero R, Markel G, Adler Y. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64:1384-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Imazio M, Trinchero R. Myopericarditis: Etiology, management, and prognosis. Int J Cardiol. 2008;127:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 12. | Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, Kindermann I, Gutberlet M, Cooper LT, Liu P, Friedrich MG. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J Am Coll Cardiol. 2018;72:3158-3176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 762] [Cited by in RCA: 1336] [Article Influence: 222.7] [Reference Citation Analysis (0)] |
| 13. | Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7073] [Cited by in RCA: 6623] [Article Influence: 946.1] [Reference Citation Analysis (0)] |
| 14. | Mahrholdt H, Greulich S. Prognosis in Myocarditis: Better Late Than (N)ever! J Am Coll Cardiol. 2017;70:1988-1990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |