Published online Oct 26, 2020. doi: 10.4330/wjc.v12.i10.492
Peer-review started: November 26, 2019
First decision: March 18, 2020
Revised: June 8, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: October 26, 2020
Processing time: 331 Days and 12.3 Hours
Although early abdominal complications after coronary artery bypass grafting (CABG) with cardiopulmonary bypass (CPB) are rare, the associated mortality remains high.
To develop a risk score for the prediction of early abdominal complications after CABG with CPB.
This retrospective study was performed in the Federal State Budgetary Establishment “Federal Center of Cardiovascular Surgery” of the Ministry of Health of Russia (the city of Chelyabinsk) and included data of 6586 patients who underwent CABG with CPB during 2011-2017. The risk factors taken for evaluation were compared between patients with early abdominal complications (n = 73) and without them (n = 6513). We identified the most important risk factors and their influence on the development of early abdominal complications after CABG with CPB.
Gender and the presence of postinfarction cardiosclerosis, chronic kidney disease, or diabetes in the anamnesis did not affect the occurrence of abdominal complications. The leading risk factors of the early abdominal complications after CABG with CPB were multifocal atherosclerosis, extracorporeal membrane oxygenation, intra-aortic balloon pump, atrial fibrillation, perioperative myocardial infarction, and the need for resternotomy in the postoperative period. The average value of the predicted probability was 0.087 ± 0.015 in patients with early abdominal complications after CABG with CPB and 0.0094 ± 0.0003 in patients without these complications. The percentage of correct classification turned out to be 98.9%. After calculating a score for each of the leading risk factors, we counted a total score for each particular patient. The highest risk was noted in patients with a total score of 7 or more.
The developed score predicts the risk of early abdominal complications after CABG with CPB and makes it possible to stratify patients by risk groups.
Core Tip: Although early abdominal complications after coronary artery bypass grafting (CABG) with cardiopulmonary bypass (CPB) are rare, the associated mortality remains high. We developed a score for the prediction of early abdominal complications after CABG with CPB. The leading risk factors were multifocal atherosclerosis, extracorporeal membrane oxygenation, intra-aortic balloon pump, atrial fibrillation, perioperative myocardial infarction, and the need for resternotomy in the postoperative period. A risk score that involves these factors makes it possible to stratify patients, which is important for timely treatment and diagnosis and, ultimately, will help to reduce postoperative mortality.
- Citation: Belov DV, Garbuzenko DV, Abramovskikh KA, Arefyev NO. Risk score for predicting abdominal complications after coronary artery bypass grafting. World J Cardiol 2020; 12(10): 492-500
- URL: https://www.wjgnet.com/1949-8462/full/v12/i10/492.htm
- DOI: https://dx.doi.org/10.4330/wjc.v12.i10.492
Abdominal complications in patients who underwent coronary artery bypass grafting (CABG) with cardiopulmonary bypass (CPB) are rare (1.1%) but associated with high mortality, which reaches 90%[1,2]. Predicting the risk of their development may be one of the ways to solve this problem.
One way to reduce mortality in this category of patients is to predict the risk of abdominal complications[3]. Our aim was to develop a score for predicting early abdominal complications after CABG with CPB.
We retrospectively analyzed individual medical records of 6586 patients who underwent CABG with CPB in the Federal Center of Cardiovascular Surgery of the Ministry of Health of Russia (the city of Chelyabinsk) during 2011-2017. Cases of acute cholecystitis, acute pancreatitis, acute mesenteric ischemia, intestinal necrosis, and acute intestinal obstruction that developed prior to discharge of the patient were referred to as early abdominal complications.
Some patients had postinfarction cardiosclerosis, chronic kidney disease, or type 1 or type 2 diabetes in the anamnesis.
Diabetes was diagnosed using one of the following diagnostic criteria: (1) Classic symptoms of diabetes (polyuria, polydipsia, ketonuria, and rapid weight loss) and a random venous plasma glucose concentration of ≥ 11.1 mmol/L; (2) Fasting glucose concentration of ≥ 7.0 mmol/L in venous plasma or ≥ 6.1 mmol/L in whole blood; and (3) 2-h plasma glucose concentration of ≥ 11.1 mmol/L during a 75-g oral glucose tolerance test.
In each case, measurement of glucose concentration was repeated on a second occasion to confirm the diagnosis[4].
Chronic kidney disease was diagnosed if either of the following was present for > 3 mo: Glomerular filtration rate of < 60 mL/min/1.73 m2; One or more markers of kidney damage: (1) Albuminuria (ACR ≥ 30 mg/g), (2) Urine sediment abnormalities, (3) Electrolyte and other abnormalities due to tubular disorders, (4) Abnormalities detected by histology, (5) Structural abnormalities detected by imaging, and (6) History of kidney transplantation[5].
Each medical record contained a completed and signed informed voluntary consent of the patient to the processing and use of his/her personal data and written consent to treatment. Information that was taken into account to evaluate the risk factors for abdominal complications is presented in Table 1.
| Factor | Indicator | Mean (95%CI) or n (%) |
| Male sex | 1–Presence/0-Absence | 5164 (78.4) |
| Age in years | Number | 61 (56 to 66) |
| Weight, kg | Number | 82 (73 to 93) |
| Height, cm | Number | 169 (161 to 174) |
| Body mass index, kg/m2 | Number | 29.27 (26.35 to 32.56) |
| Left ventricular ejection fraction, % | Number | 55.69 (47.74 to 61) |
| Post-infarction cardiosclerosis | 1–Presence/0-Absence | 4429 (67.2) |
| Cerebrovascular accident in the anamnesis | 1–Presence/0-Absence | 359 (5.5) |
| Chronic kidney disease | 1–Presence/0-Absence | 917 (13.9) |
| Multifocal atherosclerosis | 1–Presence/0-Absence | 673 (10.2) |
| Diabetes | 1–Presence/0-Absence | 1452 (22) |
| The duration of cardiopulmonary bypass in min | Number | 77 (60 to 107) |
| Aortic clamping time in min | Number | 41 (31 to 61) |
| Combination of coronary artery bypass grafting with valve correction | 1–Presence/0-Absence | 1049 (15.9) |
| Resternotomy | 1–Presence/0-Absence | 294 (4.5) |
| Postoperative bleeding requiring resternotomy | 1–Presence/0-Absence | 182 (2.8) |
| Other reasons for resternotomy | 1–Presence/0-Absence | 100 (1.52) |
| Atrial fibrillation in the postoperative period | 1–Presence/0-Absence | 695 (10.6) |
| Intra- and postoperative myocardial infarction | 1–Presence/0-Absence | 90 (1.37) |
| Intra- and postoperative cerebrovascular accident | 1–Presence/0-Absence | 74 (1.12) |
| Intra-aortic balloon pump | 1–Presence/0-Absence | 13 (0.19) |
| Extracorporeal membrane oxygenation | 1–Presence/0-Absence | 30 (0.45) |
The anamnestic risk factors and the risk factors that occurred within 2 d from the date of surgery were taken for evaluation and compared between patients with early abdominal complications (n = 73) and without them (n = 6513), and the relative risks (RRs) were calculated. Statistical data processing was performed using Statistica 10.0 (Statsoft, Tulsa, OK, United States) and SPSS 23.0 (IBM Corp., Armonk, NY, United States). In order to describe the risks, contingency tables were used to calculate the RR and the odds ratio.
An integrated score for assessing the risk of early abdominal complications was created on the basis of the above-mentioned factors by using multivariate logistic regression analysis. The presence or absence of complications was a dependent variable, while the above-mentioned factors were independent variables. Then, the obtained risk score was evaluated by using a receiver operating characteristic (ROC) curve analysis. The presence or absence of early abdominal complications was an outcome variable. The ordinate axis (sensitivity) corresponded to the true positive rate; the abscissa axis (1-specificity) corresponded to the false positive rate. It is generally supposed that the area under the ROC curve that is in the range of 0.9-1.0 should be considered as an indicator of the highest informativeness of the diagnostic method. The range of 0.8-0.9 is good, 0.7-0.8 is acceptable, 0.6-0.7 is weak, and 0.5-0.6 is extremely weak.
In order to determine the probability of early abdominal complications after CABG with CPB, the RRs of their development were analyzed according to the presence and absence of the factors included in the study. Gender and the presence of postinfarction cardiosclerosis, chronic kidney disease, or type 1 or type 2 diabetes in the anamnesis did not affect the occurrence of abdominal complications.
At the same time, abdominal complications most often occurred in patients with extracorporeal membrane oxygenation (RR = 38.7), intra-aortic balloon pump (RR = 29.3), and acute myocardial infarction diagnosed after surgery (RR = 21.9). In addition, the development of early abdominal complications was possible in patients who had the following risk factors: Resternotomy (RR = 14.1); ischemic and hemorrhagic brain stroke (RR = 9.4); atrial fibrillation (RR = 8.2); multifocal atherosclerosis, namely the presence of hemodynamically significant stenoses, not only in coronary arteries but also in the brachiocephalic arteries, arteries of the upper and lower extremities, and renal arteries (RR = 4.0); CPB with the duration of more than 125 min (RR = 3.19); a combination of CABG with valve correction (RR = 3.4); aortic clamping time of more than 70 min (RR = 2.5); and age over 70 years (RR = 2.3) (Table 2).
| Factor | Patients with the presence of a studied factor | Patients with the absence of a studied factor | Relative risk | Р value | ||
| n | Risk of abdominal complications, n (%) | n | Risk of abdominal complications, n (%) | |||
| Extracorporeal membrane oxygenation | 30 | 11 (36.67) | 6556 | 62 (0.95) | 38.7 | < 0.001 |
| Intra-aortic balloon pump | 13 | 4 (30.77) | 6573 | 69 (1.05) | 29.3 | < 0.001 |
| Perioperative myocardial infarction | 90 | 17 (18.89) | 6496 | 56 (0.86) | 21.9 | < 0.001 |
| Resternotomy | 294 | 29 (9.86) | 6292 | 44 (0.7) | 14.1 | < 0.001 |
| Cerebrovascular accident in the perioperative period | 74 | 7 (9.46) | 6512 | 65 (1.0) | 9.4 | < 0.001 |
| Atrial fibrillation in the postoperative period | 695 | 36 (5.18) | 5891 | 37 (0.63) | 8.2 | < 0.001 |
| Multifocal atherosclerosis | 673 | 23 (3.42) | 5913 | 50 (0.85) | 4.0 | < 0.001 |
| Combination of coronary artery bypass grafting with valve correction | 1049 | 29 (2.76) | 5537 | 44 (0.79) | 3.4 | < 0.001 |
| Cardiopulmonary bypass with the duration of more than 125 min | 1238 | 31 (2.5) | 5348 | 42 (0.79) | 3.19 | < 0.001 |
| Aortic clamping time of more than 70 min | 1374 | 29 (2.11) | 5212 | 44 (0.84) | 2.5 | < 0.001 |
| Age over 70 yr | 830 | 18 (2.17) | 5756 | 55 (0.96) | 2.3 | 0.0018 |
| Cerebrovascular accident in the anamnesis | 359 | 8 (2.23) | 6227 | 65 (1.04) | 2.1 | 0.037 |
| Chronic kidney disease | 917 | 14 (1.53) | 5669 | 59 (1.04) | 1.4 | 0.19 |
| Male sex | 5164 | 60 (1.16) | 1422 | 13 (0.91) | 1.3 | 0.43 |
| Postinfarction cardiosclerosis | 4429 | 48 (1.08) | 2157 | 25 (1.16) | 0.94 | 0.78 |
| Diabetes | 1452 | 10 (0.69) | 5134 | 63 (1.23) | 0.56 | 0.084 |
Based on the data obtained, a multivariate logistic regression model analysis was done in order to create an integrated score for assessing the risk of early abdominal complications after CABG with CPB. The presence or absence of complications was a dependent variable and the six most significant risk factors were independent variables (Table 3).
| Risk factor | B ± SE | Exp (B) | P value |
| Multifocal atherosclerosis | 0.74 ± 0.28 | 2.10 | 0.001 |
| Extracorporeal membrane oxygenation | 2.323 ± 0.546 | 10.207 | < 0.001 |
| Intra-aortic balloon pump | 1.762 ± 0.887 | 5.824 | 0.047 |
| Resternotomy | 1.922 ± 0.316 | 6.833 | < 0.001 |
| Atrial fibrillation in the postoperative period | 1.62 ± 0.262 | 5.054 | < 0.001 |
| Perioperative myocardial infarction | 1.384 ± 0.415 | 3.991 | 0.001 |
| Constant | 5.508 ± 0.193 | 0.004 | < 0.001 |
It was found that the most significant independent risk factors were extracorporeal membrane oxygenation, intra-aortic balloon pump, and resternotomy in the postoperative period, followed by atrial fibrillation, perioperative acute myocardial infarction, and multifocal atherosclerosis. The average value of the predicted probability was 0.087 ± 0.015 in patients with early abdominal complications after CABG with CPB and 0.0094 ± 0.0003 in patients without these complications. The percentage of correct classification turned out to be 98.9%.
To facilitate the use of this model in practice, each factor was assigned a specific score reflecting its contribution to the total risk of early abdominal complications after CABG with CPB (Table 4).
| Risk factor | Score |
| Multifocal atherosclerosis | 3 |
| Extracorporeal membrane oxygenation | 10 |
| Intra-aortic balloon pump | 6 |
| Atrial fibrillation in the postoperative period | 5 |
| Perioperative myocardial infarction | 4 |
| The need to perform postoperative resternotomy (excluding patients with extracorporeal membrane oxygenation) | 7 |
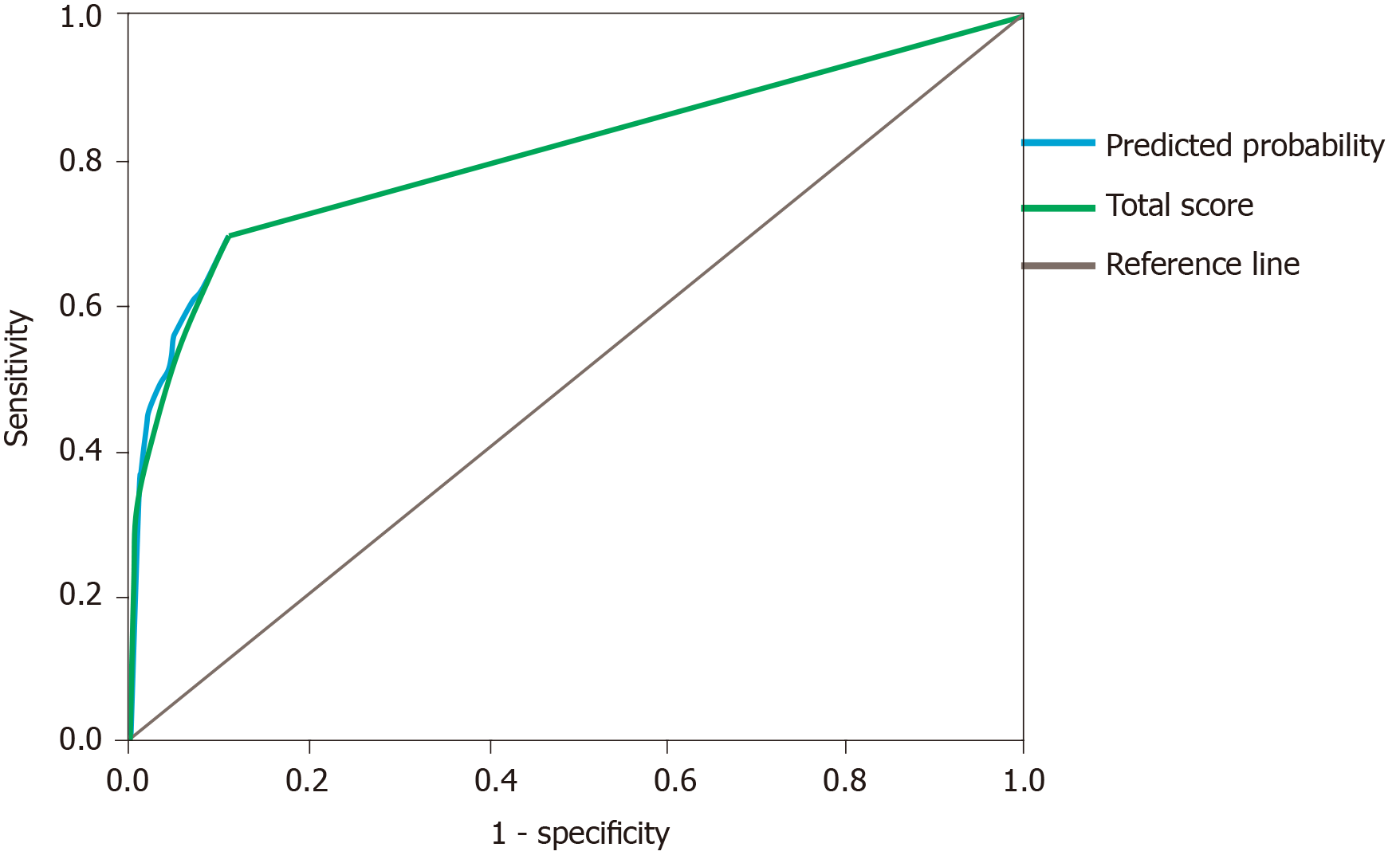
To evaluate the probability of early abdominal complications for each patient, we calculated the exact predicted probability by using the created logistic regression model and the sum of scores. Next, both of them were compared by using a ROC analysis. The criterion “presence/absence” of complications was used as an outcome variable (Table 5 and Figure 1).
| Factor | AUC | SE (AUC) | 95%CI | P value |
| The exact predicted probability | 0.805 | 0.033 | 0.739-0.869 | < 0.001 |
| Total score | 0.805 | 0.033 | 0.740-0.871 | < 0.001 |
The data presented in Figure 1 indicates that the ROC-curve for the indicator “sum of scores” almost coincides with that for the predicted probability and has a good diagnostic value [area under the curve (referred to as the AUC) = 0.805 ± 0.033, P < 0.001].
After the ROC curve analysis, we found it reasonable to divide the curve into four segments that would reflect the low, moderate, high, and very high risk (Table 6).
| Risk group | Score | Risk of abdominal complications, % | n | The percentage of the risk group in the general population, % |
| Low risk of abdominal complications | 0 | 0.4 | 5072 | 77.0 |
| Moderate risk of abdominal complications | 1-6 | 1.2 | 1047 | 15.9 |
| High risk of abdominal complications | 7-12 | 9.4 | 421 | 6.4 |
| Very high risk of abdominal complications | ≥ 13 | 44 | 46 | 0.7 |
We also prospectively evaluated our scale in a group of patients who underwent CABG with CPB in 2018. The identification of a high and very high risk group for abdominal complications contributed to early diagnosis in 14 patients. The number of lethal cases was 20 (27.4%) for 2011-2017 and decreased to 2 (14.3%) cases in 2018 (P < 0.05). Hence, the hospital mortality decreased to 52.2% in the group of patients with early abdominal complications.
The division of patients into risk groups according to the development of abdominal complications after CABG with CPB suggests a differentiated approach to their management in the postoperative period. Patients with a score of more than 7 according to our score require particular attention.
Abdominal complications after CABG with CPB are found in 0.2%-5.5% of operated patients[6] and are accompanied by a mortality rate from 11% to 74%[7]. Therefore, it is relevant to identify risk factors for predicting the development of abdominal complications.
Long-term CPB is accompanied by a wide range of pathophysiological disorders, which include non-pulsating blood flow, activation of hormonal immunity, anticoagulation, hypothermia, decreased organ perfusion, redistribution of blood flow, threat of embolism, and hyperkalemia[6]. It is known that subphysiological blood flow, the release of endogenous vasoconstrictors, including angiotensin II, and the subsequent increase in systemic vascular resistance during CPB may lead to abdominal ischemia, especially if atherosclerotic lesions are present[8,9].
An increase in aortic clamping time may lead to low cardiac output and/or release of inflammatory mediators[10]. In addition, if CABG is combined with valve surgery, the risk of mesenteric embolism increases[11].
In patients with postoperative bleeding that requires a resternotomy and in the case when a ventilation time is more than 24 h, there is a decrease in cardiac output and in mean arterial pressure and an increase in vascular resistance of internal organs, which induce temporary hypoperfusion[12]. These disorders of splanchnic hemodynamics are exacerbated by the activation of the renin-angiotensin-aldosterone system and increased levels of catecholamines.
Severe acute perioperative myocardial infarction is accompanied by a decrease in cardiac output, systemic hypotension with the centralization of blood circulation, and a decrease in mesenteric perfusion[13,14]. They are also facilitated by the following factors: (1) Vasopressors that are used to treat myocardial infarction[15]; (2) Prolongation of CPB and mechanical ventilation[16]; (3) Resternotomy for reshunting[6,8,17]; (4) Extracorporeal membrane oxygenation[16,18]; and (5) Intra-aortic balloon counterpulsation, when there is thromboembolism of visceral arteries or their obstruction due to incorrect positioning[17,19].
Atrial fibrillation in the postoperative period contributes to the embolism of the mesenteric vasculature[12], which is also possible during manipulations on the aorta in multifocal atherosclerosis[10]. In the latter, hemodynamically insignificant stenoses in the superior mesenteric artery exacerbate the impairment of mesenteric perfusion caused by hypovolemia and hypotension. In addition, multifocal atherosclerosis may act as an independent risk factor of early abdominal complications in patients older than 70 years[18].
Comparing the literature data with the results of our own research, we identified the most significant risk factors and used them to develop a prognostic score, which had a good diagnostic value (AUC = 0.805 ± 0.033, P < 0.001). This score allows us to stratify patients with the risk for early abdominal complications after CABG with CPB, which is important for timely treatment and diagnosis and, ultimately, will help to reduce postoperative mortality[20].
In conclusion, the leading risk factors for early abdominal complications after CABG with CPB in our study were multifocal atherosclerosis, extracorporeal membrane oxygenation, intra-aortic balloon pump, atrial fibrillation, acute perioperative myocardial infarction, and the need for performing postoperative resternotomy. According to the developed score, patients with a score of 7 or more had the highest risk of abdominal complications. The score makes it possible to predict the risk of early abdominal complications after CABG with CPB and to stratify patients with the risk for their development, which is important for timely treatment and diagnosis and, ultimately, will help to reduce postoperative mortality.
Abdominal complications in patients who underwent cardiac surgery are rare but the associated mortality varies from 11.0% to 74.0%, which makes the problem relevant. One reason for high mortality rates is late diagnosis. Certain difficulties in diagnosing these complications are associated with the peculiarities of postoperative management and unclear clinical picture due to sedation, analgesia, prolonged mechanical ventilation, and the use of extracorporeal membrane oxygenation. Determining the risk factors for abdominal complications and identifying high-risk groups is an urgent task that may help diagnose abdominal complications and reduce related mortality.
The topic of this study is the identification of leading risk factors for abdominal complications in patients after coronary artery bypass grafting (CABG) with cardiopulmonary bypass (CPB) and the development of a prediction score based on perioperative predictors to reveal patients at a high risk of abdominal complications.
The objectives of this study were to identify risk factors for abdominal complications according to clinical, laboratory, and imaging findings, to determine their rank influence on the development of early abdominal complications after CABG with CPB, and to develop a risk prediction score. The risk score makes it possible to perform early screening and to develop an algorithm of therapeutic and diagnostic measures for the prevention, early diagnosis, and treatment of this pathology.
The factors taken for evaluation were compared between patients with early abdominal complications (n = 73) and without them (n = 6513), and the relative risks were calculated. Statistical data processing was performed using Statistica 10.0 (Statsoft, Tulsa, OK, United States) and SPSS 23.0 (IBM Corp., Armonk, NY, United States). In order to describe the risks, contingency tables were used to calculate the relative risk and the odds ratio. An integrated score for assessing the risk of early abdominal complications was created on the basis of the above-mentioned factors by using multivariate logistic regression analysis. The presence or absence of complications was a dependent variable, while the above-mentioned factors were independent variables. Then, the obtained risk score was evaluated by using a receiver operating characteristic curve analysis. The presence or absence of early abdominal complications was an outcome variable. The ordinate axis (sensitivity) corresponded to the true positive rate; the abscissa axis (1-specificity) corresponded to the false positive rate. It is generally supposed that the area under the receiver operating characteristic curve that is in the range of 0.9-1.0 should be considered as an indicator of the highest informativeness of the diagnostic method. The range of 0.8-0.9 is good, 0.7-0.8 is acceptable, 0.6-0.7 is weak, and 0.5-0.6 is extremely weak.
The leading risk factors of the early abdominal complications after CABG with CPB were multifocal atherosclerosis, extracorporeal membrane oxygenation, intra-aortic balloon pump, atrial fibrillation, perioperative myocardial infarction, and need for resternotomy in the postoperative period. After calculating a score for each of the leading risk factors, we counted a total score for each particular patient. The highest risk was noted in patients with a total score of 7 or more. Further research may be devoted to a prospective assessment of the proposed scale for the prediction of the risk of abdominal complications and the development of an algorithm for the management of high-risk patients.
The developed score predicts the risk of early abdominal complications after CABG with CPB and makes it possible to stratify patients by risk groups. It is important for timely treatment and diagnosis and, ultimately, will help to reduce postoperative mortality in this group of patients.
Future studies should prospectively assess the effectiveness of the proposed method, as well as to create a protocol for the prevention, early diagnosis, and treatment of abdominal complications in high-risk patients.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D, D, D
Grade E (Poor): 0
P-Reviewer: Ciccone MM, Cirillo P, Ito S, Iyngkaran P S-Editor: Zhang H L-Editor: Filipodia P-Editor: Li JH
| 1. | Garbuzenko DV, Belov DV, Arefyev NO. A rare complication of cardiac surgery: Ogilvie syndrome. J Postgrad Med. 2019;65:56-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Yarustovskij MB, Abramyan MV, Nazarov NS, Komardina EV, Volkova SS. Abdominal complications after heart surgery in a cardiopulmonary bypass. Bull Bakoulev Center Cardiovasc Surg. 2018;3:318-326. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2722] [Cited by in RCA: 4478] [Article Influence: 895.6] [Reference Citation Analysis (0)] |
| 4. | American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care. 2011;34 Suppl 1:S11-S61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1908] [Cited by in RCA: 1917] [Article Influence: 136.9] [Reference Citation Analysis (1)] |
| 5. | Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1707] [Cited by in RCA: 2469] [Article Influence: 205.8] [Reference Citation Analysis (0)] |
| 6. | Viana FF, Chen Y, Almeida AA, Baxter HD, Cochrane AD, Smith JA. Gastrointestinal complications after cardiac surgery: 10-year experience of a single Australian centre. ANZ J Surg. 2013;83:651-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Guler A, Sahin MA, Atilgan K, Kurkluoglu M, Demirkilic U. A rare complication after coronary artery bypass graft surgery: Ogilvie's syndrome. Cardiovasc J Afr. 2011;22:335-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Allen SJ. Gastrointestinal complications and cardiac surgery. J Extra Corpor Technol. 2014;46:142-149. [PubMed] |
| 9. | Belov DV, Garbuzenko DV, Fokin AA, Milievskaya EB. Risk factors for developing abdominal complications after coronary artery bypass grafting. Bull Bakoulev Center Cardiovasc Surg. 2018;6:794-799. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Hessel EA 2nd. Abdominal organ injury after cardiac surgery. Semin Cardiothorac Vasc Anesth. 2004;8:243-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Chung JW, Ryu SH, Jo JH, Park JY, Lee S, Park SW, Song SY, Chung JB. Clinical implications and risk factors of acute pancreatitis after cardiac valve surgery. Yonsei Med J. 2013;54:154-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Chaudhry R, Zaki J, Wegner R, Pednekar G, Tse A, Sheinbaum R, Williams GW. Gastrointestinal Complications After Cardiac Surgery: A Nationwide Population-Based Analysis of Morbidity and Mortality Predictors. J Cardiothorac Vasc Anesth. 2017;31:1268-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Lin TW, Tsai MT, Roan JN, Liu YS, Tsai HM, Luo CY. Obscured hemorrhagic pancreatitis after orthotopic heart transplantation complicated with acute right heart failure and hepatic dysfunction: a case report. J Cardiothorac Surg. 2016;11:166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Rybka MM. Acute ischemic injury of the intestinal wall. Bull Bakoulev Center Cardiovasc Surg. 2016;5:11-18. |
| 15. | Sever K, Ozbek C, Goktas B, Bas S, Ugurlucan M, Mansuroglu D. Gastrointestinal complications after open heart surgery: incidence and determinants of risk factors. Angiology. 2014;65:425-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Karangelis D, Oikonomou K, Koufakis T. Gastrointestinal Complications Following Heart Surgery: An Updated Review. Eur J Cardiovasc Med. 2011;1:23-28. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Groesdonk HV, Klingele M, Schlempp S, Bomberg H, Schmied W, Minko P, Schäfers HJ. Risk factors for nonocclusive mesenteric ischemia after elective cardiac surgery. J Thorac Cardiovasc Surg. 2013;145:1603-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Plotnikov GP, SHukevich DL, Grigor'ev EV. Abdominal Complication After Cardiac Surgical Procedures With Extracorporeal Circulation. Complex Probl Cardiovasc Dis. 2014;1:75-86. |
| 19. | Karhausen J, Stafford-Smith M. The role of nonocclusive sources of acute gut injury in cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28:379-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Lukin OP, Belov DV, Milievskaya EB. Organization of high-tech cardiac surgical medical care in the Ural Federal District. Russ J Thorac Cardiovasc Surg. 2018;60:281-286. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |