Published online Jul 26, 2019. doi: 10.4330/wjc.v11.i7.189
Peer-review started: January 31, 2019
First decision: April 15, 2019
Revised: April 22, 2019
Accepted: June 20, 2019
Article in press: June 21, 2019
Published online: July 26, 2019
Processing time: 178 Days and 0.4 Hours
High-speed rotational atherectomy (HSRA) is most commonly used to modify calcified coronary artery lesions to facilitate stent deployment and expansion. The use of HSRA as an emergency rescue technique to release a fractured micro-catheter has not been described. We report the use of HSRA in a case of a fracture trapped corsair tip that was impeding coronary flow causing a ST elevation myocardial infarct.
A 79 years old male was scheduled for elective percutaneous coronary intervention (PCI) to his left anterior descending artery (LAD). Given its calcific nature, a decision was made for upfront rotablation. During procedural preparations, the tip of an employed micro-catheter was separated from the shaft resulting in obstructing coronary flow and ST-segment elevation. The consensus was for an attempt bail out PCI strategy. A rotafloppy wire was advanced to the distal LAD using a corsair micro-catheter which was placed proximal to the occlusion site. Modification of the mid LAD segment was performed, resulting in mobilising the corsair tip, and deflecting it to a small diagonal branch. Following serial predilation, the procedure was completed using two overlapping drug eluting stents, jailing the corsair tip in the diagonal branch. The patient made uneventful recovery and was clinically stable at one year follow up.
HSRA may be offered as a bailed-out strategy to rescue fractured and jailed micro-catheter tip in high risk surgical cases.
Core tip: Fractured micro-catheter tip impeding flow has not been previously described. With aging population and increasing calcification, this phenomenon is likely to face interventional cardiologists in the future. Non-surgical bailed-out strategy to rescue the trapped tip is described in the current case.
- Citation: Alkhalil M, McQuillan C, Moore M, Spence MS, Owens C. Use of rotablation to rescue a “fractured” micro catheter tip: A case report. World J Cardiol 2019; 11(7): 189-194
- URL: https://www.wjgnet.com/1949-8462/full/v11/i7/189.htm
- DOI: https://dx.doi.org/10.4330/wjc.v11.i7.189
Calcification remains a challenging feature of coronary atherosclerosis. The ageing population coupled with increased co-morbidities, such as renal failure and diabetes, make coronary calcification more commonly seen in daily practice[1]. In calcific lesions, high-speed rotational atherectomy (HSRA) is often necessary for lesion modification to permit optimal stent deployment and expansion[1]. HSRA has been demonstrated to be more successful than modified balloon (scoring or cutting balloon) prior to drug eluting stent implantation in severely calcified lesions[2]. The use of micro-catheter exchange to allow distal passage of the rota wire to facilitate HSRA is well described and is a useful technique in complex anatomy[1].
Here we report a complication of rotablation where the micro-catheter tip (Corasir, Asahi) was fractured and jailed in complex anatomy resulting in ST elevation myocardial infarction (STEMI) and the use of rescue HSRA to address this unique problem.
A 79 years old male was electively admitted for complex percutaneous coronary intervention (PCI) to left anterior descending artery (LAD) in a district general hospital without cardiac surgical support.
He initially presented with a lateral STEMI whereby successful primary PCI was performed to his left circumflex artery.
His medical history was significant for chronic obstructive pulmonary disease, hypertension and chronic kidney disease (stage III).
Cardiovascular examination was unremarkable.
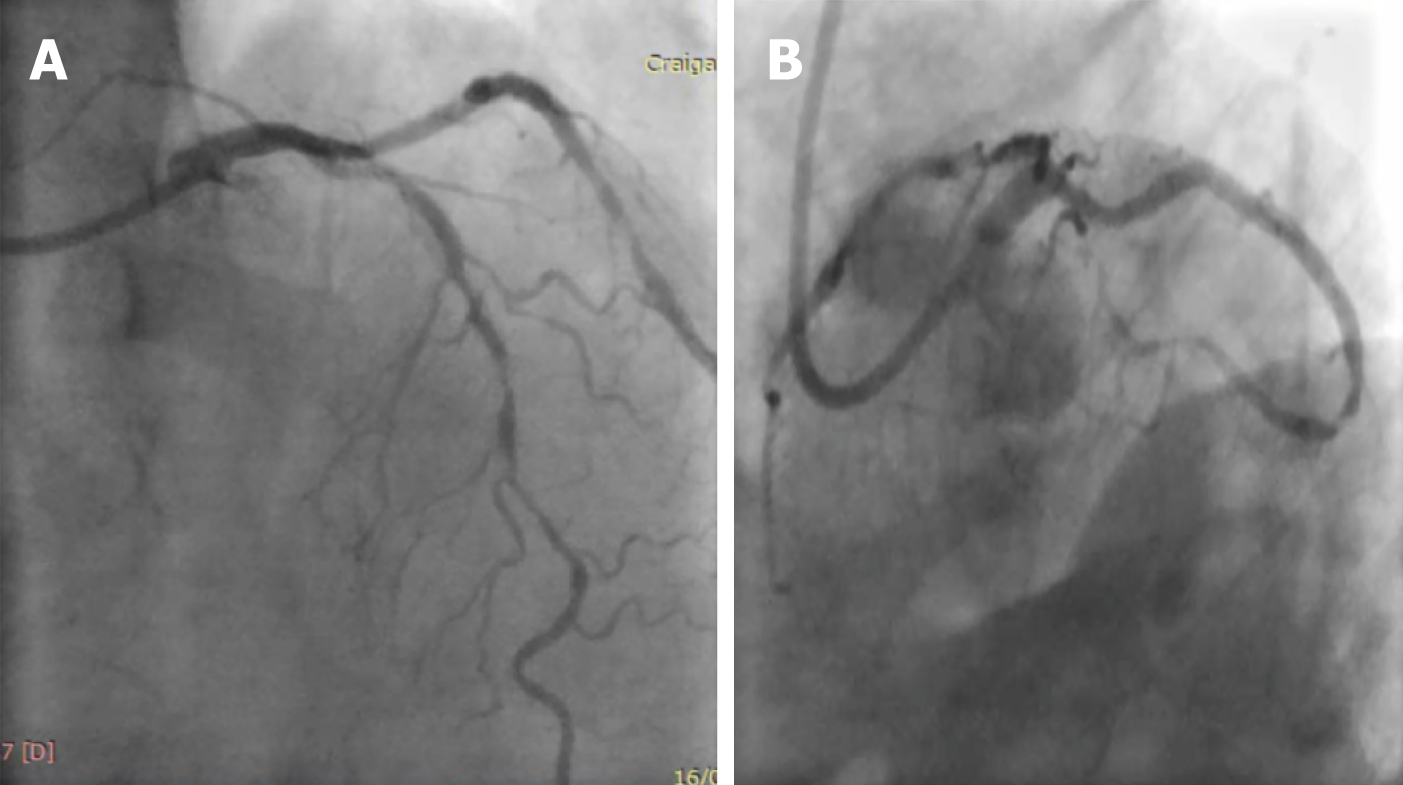
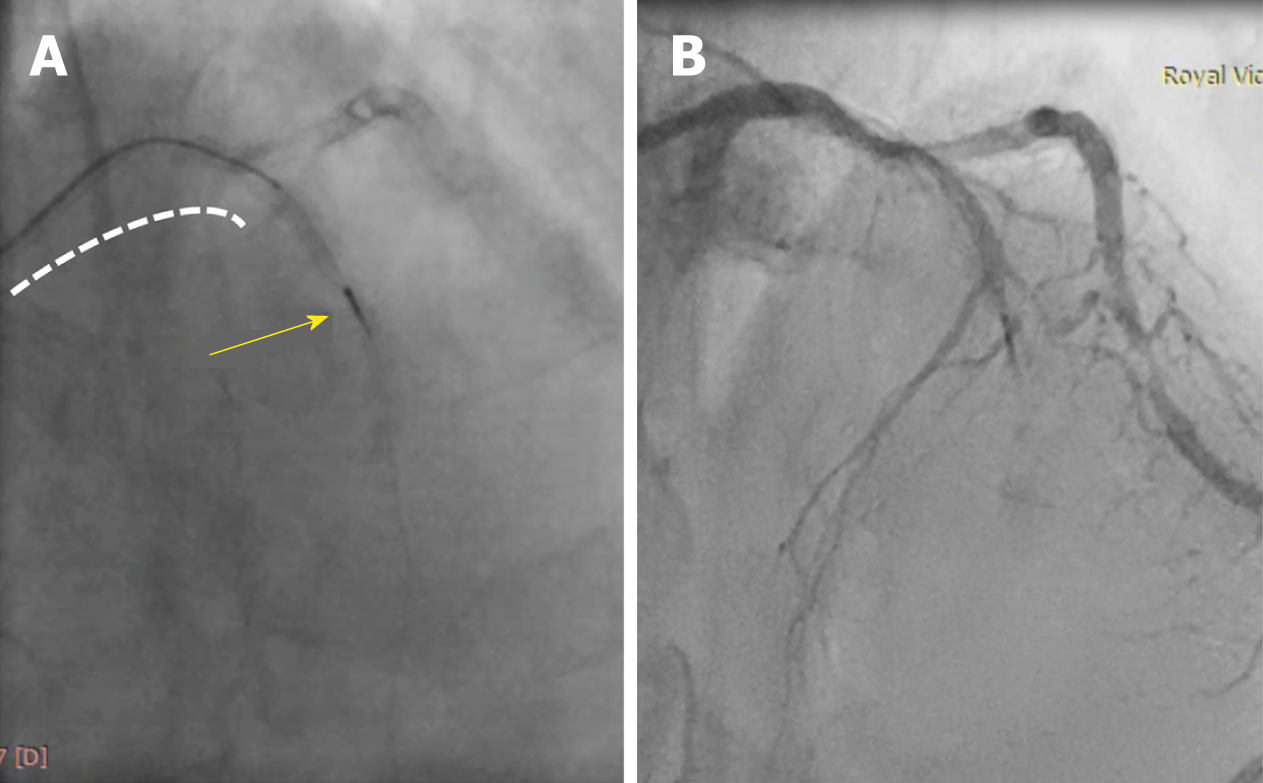
The LAD had calcific diffuse disease extending beyond the mid segment of the LAD with severe ostial disease in a diseased small calibre diagonal branch (Figure 1). Given the calcific nature of the LAD, a decision was made for upfront rotablation. A Sion blue wire (Asahi) was placed in the distal LAD to facilitate micro-catheter exchange for a rotafloppy wire (RotaLink, Boston Scientific). Despite combination of rotation and forward tension, the corsair was unsuccessful in traversing the mid LAD. Upon attempted retraction of the Corsair (Asahi) micro-catheter, it was evident that the tip of the Corsair was separated from the shaft and was trapped in the LAD (Figure 2A) resulting in obstruction of coronary flow and ST-segment elevation (Figure 2B). In an attempt to establish flow, a 1.5 mm MINI TREK (Abbott Vascular) was advanced over a second angioplasty wire beside the trapped corsair tip but would not advance past the fractured corsair tip despite Guidezilla (Boston Scientific) support. A wire-wrap technique was unsuccessfully used to try and retrieve the fractured tip but this resulted in loss of wire position. An intra-aortic balloon pump was inserted via the right femoral artery to stabilise the patient for transfer to our tertiary centre for rescue coronary artery bypass graft (CABG).
STEMI secondary to fractured and trapped micro-catheter tip.
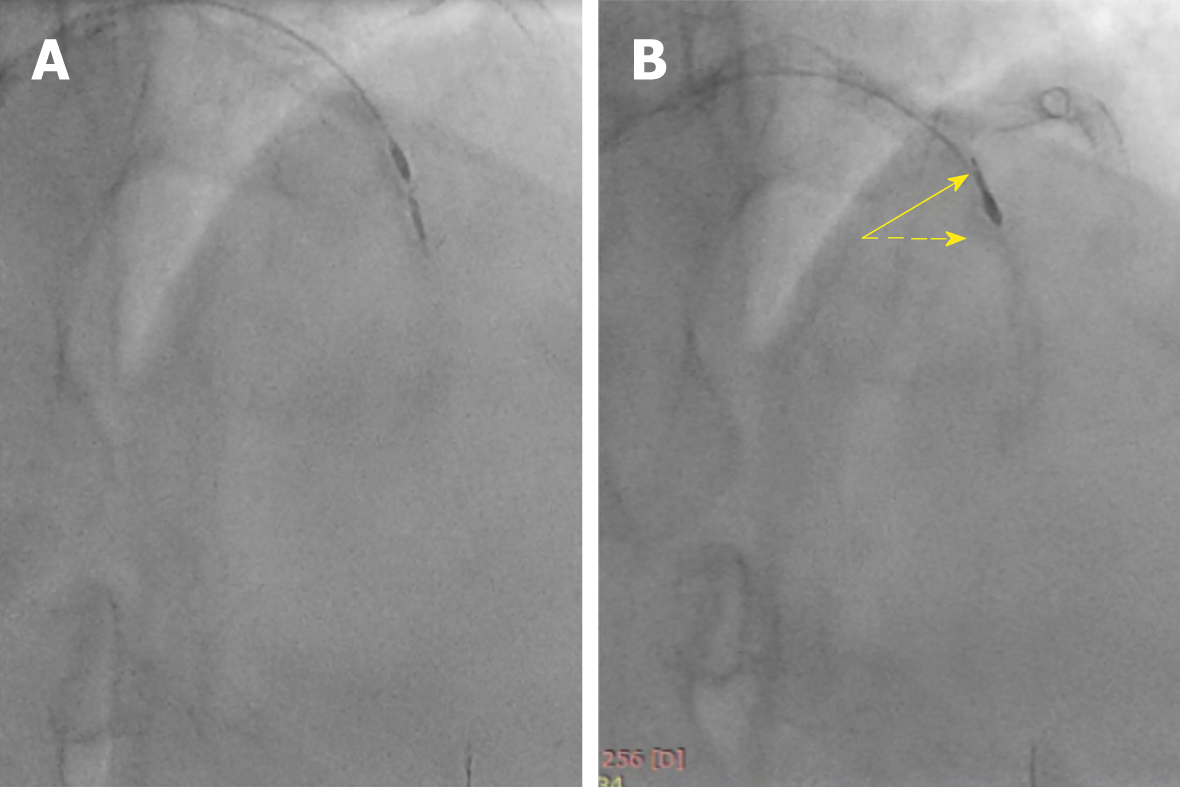
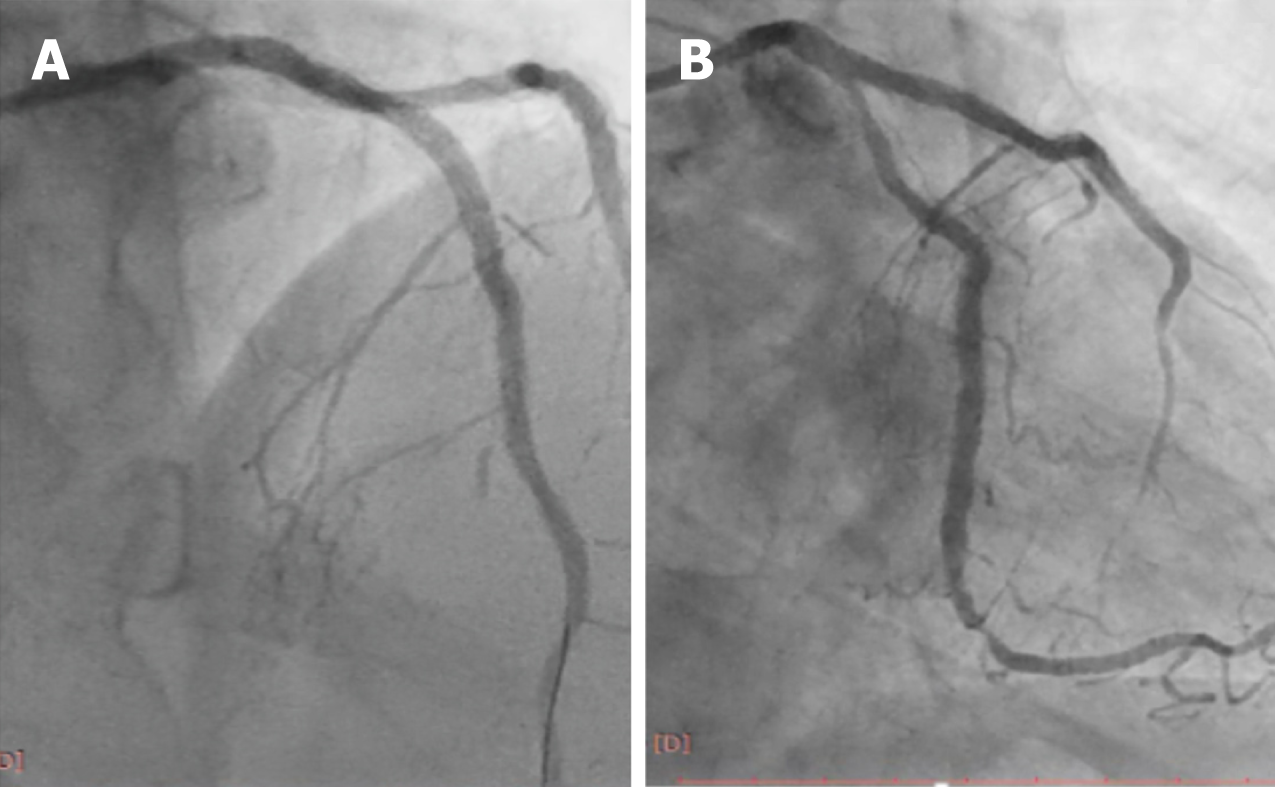
On arrival, CABG was deemed high risk due his STEMI presentation and comor-bidities. The consensus from the heart team was made for bail out PCI. Right radial access was used and a 7 French VL 3.5 guide catheter was chosen for support. Repeat imaging confirmed a heavily calcified LAD with a fractured corsair tip impeding coronary flow. A Sion blue wire was advanced beyond the occlusion site and a Corsair micro-catheter was advanced proximal to the occlusion site. A rotafloppy wire was exchanged and advanced to the distal LAD (Supplementary video 1). A 1.25 mm then 1.5 mm rota burr were used to modify the LAD past the corsair tip to free the trapped segment (Figure 3A) (Supplementary video 2). This has resulted in mobilising the corsair tip, deflecting to the small diagonal branch during the forward movement of the rota burr and restoration of flow in the LAD (Figure 3B) (Supplementary video 3). The LAD was pre-dilated with a 2.5 mm × 30 mm non-compliant balloon and stented distally to proximally with two overlapping Synergy drug eluting stents (3.0 mm × 38 mm and 3.5 mm × 38 mm) (Boston Scientific) back to the ostium of the LAD thus jailing the corsair tip in the diagonal branch (Figure 4). This did not result in any significant hemodynamic or ECG compromise with resolution of ST elevation.
The patient made uneventful recovery without need for rescue CABG and was clinically stable at one year follow up.
The presence of severe coronary calcification is a well-established predictor of procedural success and worse clinical outcomes[3]. This remained unchanged despite improvements in contemporary PCI, including the advent of drug eluting stents[4]. In patient-level pooled analysis from seven contemporary trials, coronary calcification was associated with 33% increase in mortality rate irrespective of the Syntax score[4]. While this could be attributed to the residual and untreated coronary artery disease, coronary calcification is also considered as marker of more advanced and atherosclerotic disease making those patients at higher risk prior to any coronary intervention[5,6]. Regardless of the mechanism, heavily calcified segments may render coronary stenoses undilatable with conventional balloon angioplasty thus compromising optimal stent deployment. Optimal lesion preparation by differential cutting using HSRA has been reported more than 3 decades ago and debulking coronary atheroma with HSRA ensures less resistant plaque surface allowing balloon and subsequently stent crossing[2,6]. The use of HSRA is not without complications and includes slow flow, coronary dissection or perforation, burr lodging within the stenotic segment and thermal injury from heating to the adjacent tissue[1,7]. Here we describe, an unreported complication associated with wire exchange to facilitate HSRA. The micro-catheter was used in this case to facilitate rotafloppy wire exchange and although a useful and often necessary technique, over torqueing the micro-catheter coupled with heavy coronary calcification can result in micro-catheter tip “fracture” as in this case.
Broken and retained interventional instruments continue to be reported and may be attributed to the increasing complexity of percutaneous interventional procedures[8]. The combination of tortuosity and calcification of coronary arteries pose difficulties in navigating and delivering devices across lesions. In our case, the coronary anatomy, in addition to micro-catheter over torqueing have led the tip to “snap” and to separate from the main shaft obstructing flow. Extensive literature exist reporting fractured and retained wires that go back to the early days of coronary angioplasty[9,10]. Similarly stent loss has also been reported in a large scale study of more than 11000 PCI procedures with an incidence of < 0.5%[11]. Overall, the incidence of retained angioplasty tools did not change over time despite undergoing extensive refinements and this could be attributed to the increased complexity of PCI procedures in current daily practices. More recently, other angioplasty devices such as fragments of balloons or thrombectomy catheter have been reported to be trapped within the coronary artery[8,12]. To the best of our knowledge, this is the first report of fractured corsair catheter impeding flow and leading to STEMI. While any broken fragment could serve as a nidus for thrombus formation, vessel occlusion in our case was more related to the actual presence of the micro-catheter tip blocking the flow in a heavily calcified artery. In order to establish flow, an attempt to deliver a small balloon beyond the occlusion site was made. However, the balloon was deemed impassable and, therefore, precluded any attempt to use balloon-assisted retrieval technique to recover the retained corsair tip.
Numerous techniques have been previously reported to facilitate retrieval of entrapped coronary equipment and interventional cardiologists should familiarise themselves with different retrieval techniques[13]. In this case, use of HSRA permitted lesion modification and mobilisation of the fractured trapped corsair tip to the diagonal side branch were it was subsequently jailed by LAD stenting. Importantly, there was a risk of thermal injury to the hydrophilic tip while using HSRA. In order to prevent any excessive rise in temperature, the speed of the rotablator was set up at 180000 rpm with focus attention not to drop more than 5000-7000 rpm and a total duration of less than 20 s for each rotablation run[1,7].
We elected not to retrieve the deflected corsair tip in the diagonal branch given its relative small size with a potential risk of jeopardising the LAD. While this could be considered as a limitation, losing a side branch is not infrequent during coronary bifurcation stenting. Decision to rescue the side branch depends on numerous factors, including the size of myocardium at jeopardy[14]. The benign long term outcome of the patient supports our pragmatic decision in approaching this case.
Use of HSRA in an emergency bail out setting for a fractured and jailed corsair tip re-established coronary flow and permitted rescue of an otherwise high risk surgical bail out.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Altarabsheh SE, Kharlamov AN, Pastromas S, Ueda H S-Editor: Ji FF L-Editor: A E-Editor: Xing YX
| 1. | Barbato E, Carrié D, Dardas P, Fajadet J, Gaul G, Haude M, Khashaba A, Koch K, Meyer-Gessner M, Palazuelos J, Reczuch K, Ribichini FL, Sharma S, Sipötz J, Sjögren I, Suetsch G, Szabó G, Valdés-Chávarri M, Vaquerizo B, Wijns W, Windecker S, de Belder A, Valgimigli M, Byrne RA, Colombo A, Di Mario C, Latib A, Hamm C; European Association of Percutaneous Cardiovascular Interventions. European expert consensus on rotational atherectomy. EuroIntervention. 2015;11:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 191] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 2. | Abdel-Wahab M, Toelg R, Byrne RA, Geist V, El-Mawardy M, Allali A, Rheude T, Robinson DR, Abdelghani M, Sulimov DS, Kastrati A, Richardt G. High-Speed Rotational Atherectomy Versus Modified Balloons Prior to Drug-Eluting Stent Implantation in Severely Calcified Coronary Lesions. Circ Cardiovasc Interv. 2018;11:e007415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 188] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 3. | Savage MP, Goldberg S, Hirshfeld JW, Bass TA, MacDonald RG, Margolis JR, Taussig AS, Vetrovec G, Whitworth HB, Zalewski A. Clinical and angiographic determinants of primary coronary angioplasty success. M-HEART Investigators. J Am Coll Cardiol. 1991;17:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 108] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Bourantas CV, Zhang YJ, Garg S, Iqbal J, Valgimigli M, Windecker S, Mohr FW, Silber S, Vries Td, Onuma Y, Garcia-Garcia HM, Morel MA, Serruys PW. Prognostic implications of coronary calcification in patients with obstructive coronary artery disease treated by percutaneous coronary intervention: a patient-level pooled analysis of 7 contemporary stent trials. Heart. 2014;100:1158-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 227] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 5. | Sotomi Y, Shlofmitz RA, Colombo A, Serruys PW, Onuma Y. Patient Selection and Procedural Considerations for Coronary Orbital Atherectomy System. Interv Cardiol. 2016;11:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Valdes PJ, Diaz MA. Rotational Atherectomy. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019; . [PubMed] |
| 7. | Reisman M, Shuman BJ, Harms V. Analysis of heat generation during rotational atherectomy using different operational techniques. Cathet Cardiovasc Diagn. 1998;44:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Mehta V, Pandit BN, Trehan V. Retrieval of Broken Export Catheter during Primary Angioplasty. Int J Angiol. 2013;22:185-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Iturbe JM, Abdel-Karim AR, Papayannis A, Mahmood A, Rangan BV, Banerjee S, Brilakis ES. Frequency, treatment, and consequences of device loss and entrapment in contemporary percutaneous coronary interventions. J Invasive Cardiol. 2012;24:215-221. [PubMed] |
| 10. | Hartzler GO, Rutherford BD, McConahay DR. Retained percutaneous transluminal coronary angioplasty equipment components and their management. Am J Cardiol. 1987;60:1260-1264. [PubMed] |
| 11. | Brilakis ES, Best PJ, Elesber AA, Barsness GW, Lennon RJ, Holmes DR, Rihal CS, Garratt KN. Incidence, retrieval methods, and outcomes of stent loss during percutaneous coronary intervention: a large single-center experience. Catheter Cardiovasc Interv. 2005;66:333-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 130] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Kunwar BK, Jain P, Ghogare M. Catheter-Assisted Balloon-Supported Retrieval of a Broken Semi-Compliant Balloon from a Coronary Artery. J Clin Diagn Res. 2017;11:OD06-OD07. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Paulus BM, Fischell TA. Retrieval devices and techniques for the extraction of intravascular foreign bodies in the coronary arteries. J Interv Cardiol. 2010;23:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Lassen JF, Burzotta F, Banning AP, Lefèvre T, Darremont O, Hildick-Smith D, Chieffo A, Pan M, Holm NR, Louvard Y, Stankovic G. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:1540-1553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 152] [Article Influence: 21.7] [Reference Citation Analysis (0)] |