Published online Mar 26, 2019. doi: 10.4330/wjc.v11.i3.120
Peer-review started: January 11, 2019
First decision: January 26, 2019
Revised: March 1, 2019
Accepted: March 16, 2019
Article in press: March 16, 2019
Published online: March 26, 2019
Processing time: 88 Days and 4 Hours
Takotsubo cardiomyopathy (TCM) is a transient reversible systolic dysfunction, estimated to be the culprit in 1%-2% of patients presenting with clinical symptoms of acute coronary syndrome (ACS). TCM was previously thought to be indistinguishable from ACS on the basis of electrocardiogram (EKG) findings; many authors now describe specific EKG changes that distinguish TCM from ACS as well as aid in early recognition of TCM.
This unique case presentation illustrates an uncommon subtype of TCM, and very clearly exemplifies the specific EKG changes meant to aid in distinguishing TCM from ACS. A bronchogenic subtype of TCM has been proposed, given its prevalence and distinguishing features from TCM without pulmonary pathology; this case exemplifies that notion. The specific EKG changes of low QRS voltage and attenuation of the amplitude of the QRS complex are now being noted in the EKGs of TCM patients. This patient presented for worsening shortness of breath and increased productive cough; her EKG revealed ST elevations in leads V3-V6, and low voltage QRS complexes when compared to previous EKG from 12 wk ago; troponin peaked at 5.16 ng/mL. Left heart catheterization did not reveal significant lesions and left ventriculogram findings were consistent with TCM. Patient was treated for COPD exacerbation, her symptoms improved significantly; she was sent home on the appropriate medications.
This case exemplifies EKG changes noted in TCM patients who may aid in early detection and appropriate treatment of TCM.
Core tip: This case report presents a unique opportunity to exemplify specific electrocardiogram (EKG) changes noted in patients with Takotsubo cardiomyopathy (TCM). Low QRS voltage and attenuation of the amplitude of the QRS complex have been noted in the EKGs of TCM patients. This case report presents a patient who had an EKG performed 12 wk prior to developing TCM and thus provides a recent EKG to compare the EKG changes noted during TCM.
- Citation: Khan M, Watti H, Dahal K, Dominic P. Utility of recognizing early electrocardiogram changes in bronchogenic Takotsubo cardiomyopathy: A case report. World J Cardiol 2019; 11(3): 120-125
- URL: https://www.wjgnet.com/1949-8462/full/v11/i3/120.htm
- DOI: https://dx.doi.org/10.4330/wjc.v11.i3.120
Takotsubo cardiomyopathy (TCM) is characterized by reversible systolic dysfunction of the left ventricle in the absence of any significant obstructive coronary artery disease[1]. Most commonly, the apical and the middle segments of the left ventricle are seen to be akinetic[1]. Its clinical presentation is said to be indistinguishable from myocardial infarct[2]. The gold standard used to differentiate acute coronary syndrome (ACS) from TCM is coronary angiography as it clearly shows if a significant obstructive lesion is present[1]. Although some authors believe that it is not possible to differentiate ACS form TCM based of electrocardiogram (EKG)alone, may new case reports have been published that support the existence of unique EKG changes present only in TCM. This is a unique case presentation as it not only illustrates an uncommon subtype of TCM, but also very clearly exemplifies specific EKG changes meant to aid in distinguishing TCM from ACS. This was previously thought to be indistinguishable on the basis of electrocardiogram (EKG).
A 63 year-old Caucasian female presented to the emergency department for acute exacerbation of her chronic obstructive pulmonary disease (COPD). The patient had been experiencing 2 wk of worsening shortness of breath, productive cough and increased sputum production.
She had been using her inhalers more frequently at home and had increased her home oxygen to 3 liters, still with only minimal relief. On the day of presentation to the emergency department, the patient called an ambulance as she was concerned about her breathing.
She was noted to have a past medical history of COPD (on 2 liters home oxygen), coronary artery disease [status post right coronary artery (RCA) stent in 2000’s], subarachnoid hemorrhage and tobacco abuse.
No other family history or personal history was reported.
When the patient arrived in the emergency department, her physical exam revealed a blood pressure of 98/74 mmHg, pulse 101, temperature 97.5 °F (36.4 °C), temperature source Oral, respiratory rate of 27, and oxygen saturation of 95% on 3-4 liters of oxygen. Scoliosis of spine was also noted. Patient was noted to be in respiratory distress.
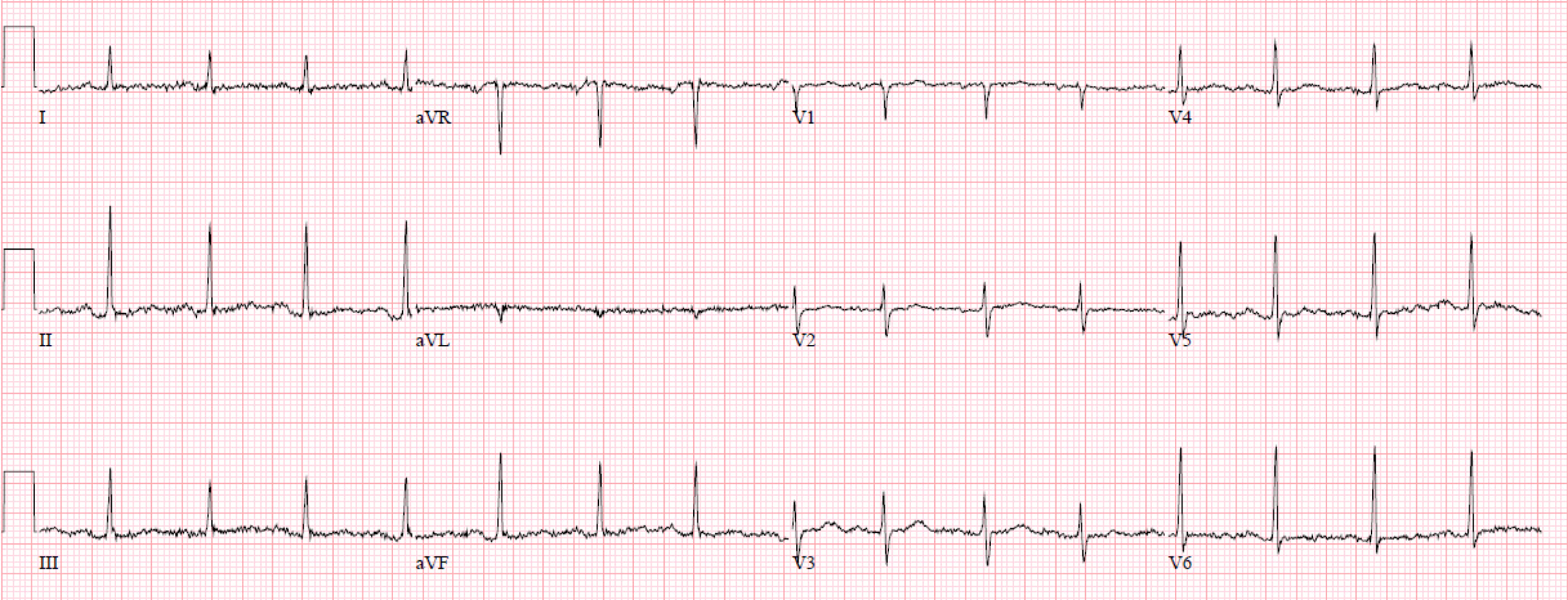
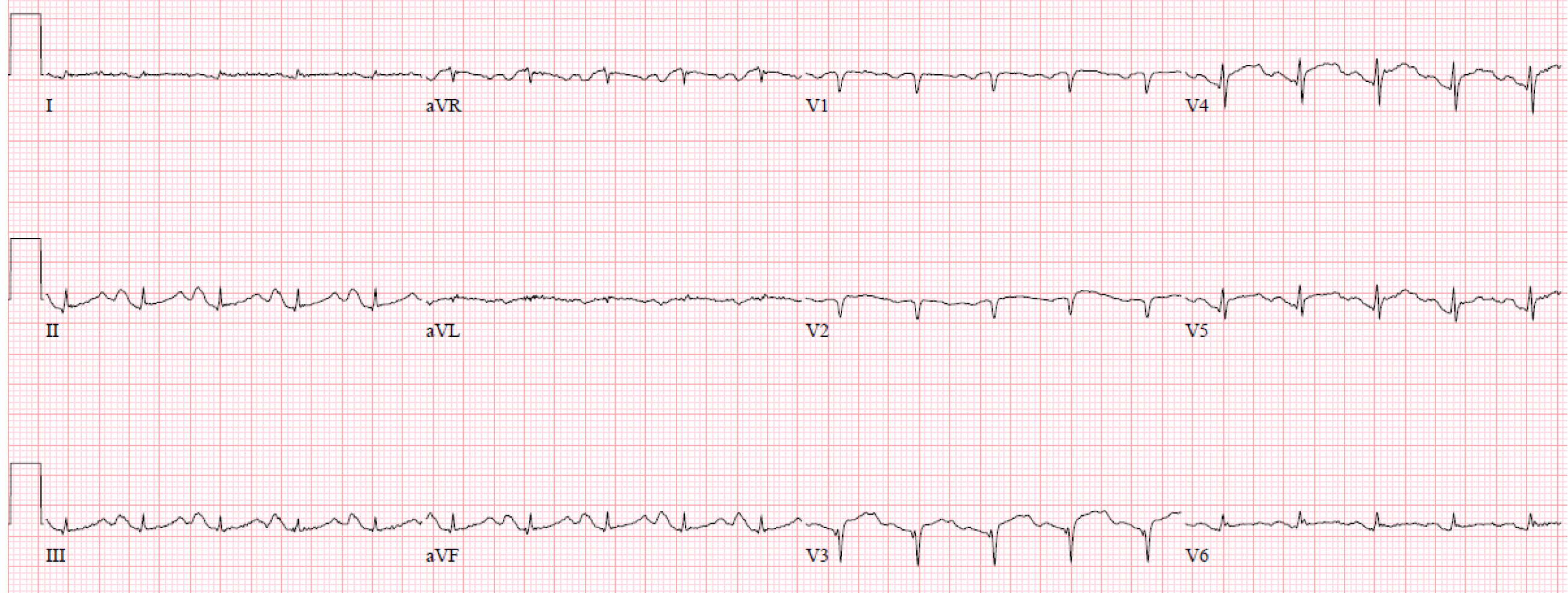
Initial troponin on presentation was 2.74 ng/mL and peaked at 5.16 ng/mL. Her renal function and hemoglobin were within normal limits. Her EKG showed sinus tachycardia with ST elevations in leads V3-V6 as well as low voltage QRS complexes when compared to previous EKG from 12 wk prior (Figures 1 and 2).
Cardiology was consulted for evaluation. The patient was advised to have an emergent left heart catheterization (LHC). However, the patient refused initially and wanted only medical management. She was not a candidate for thrombolysis due to history of subarachnoid hemorrhage.
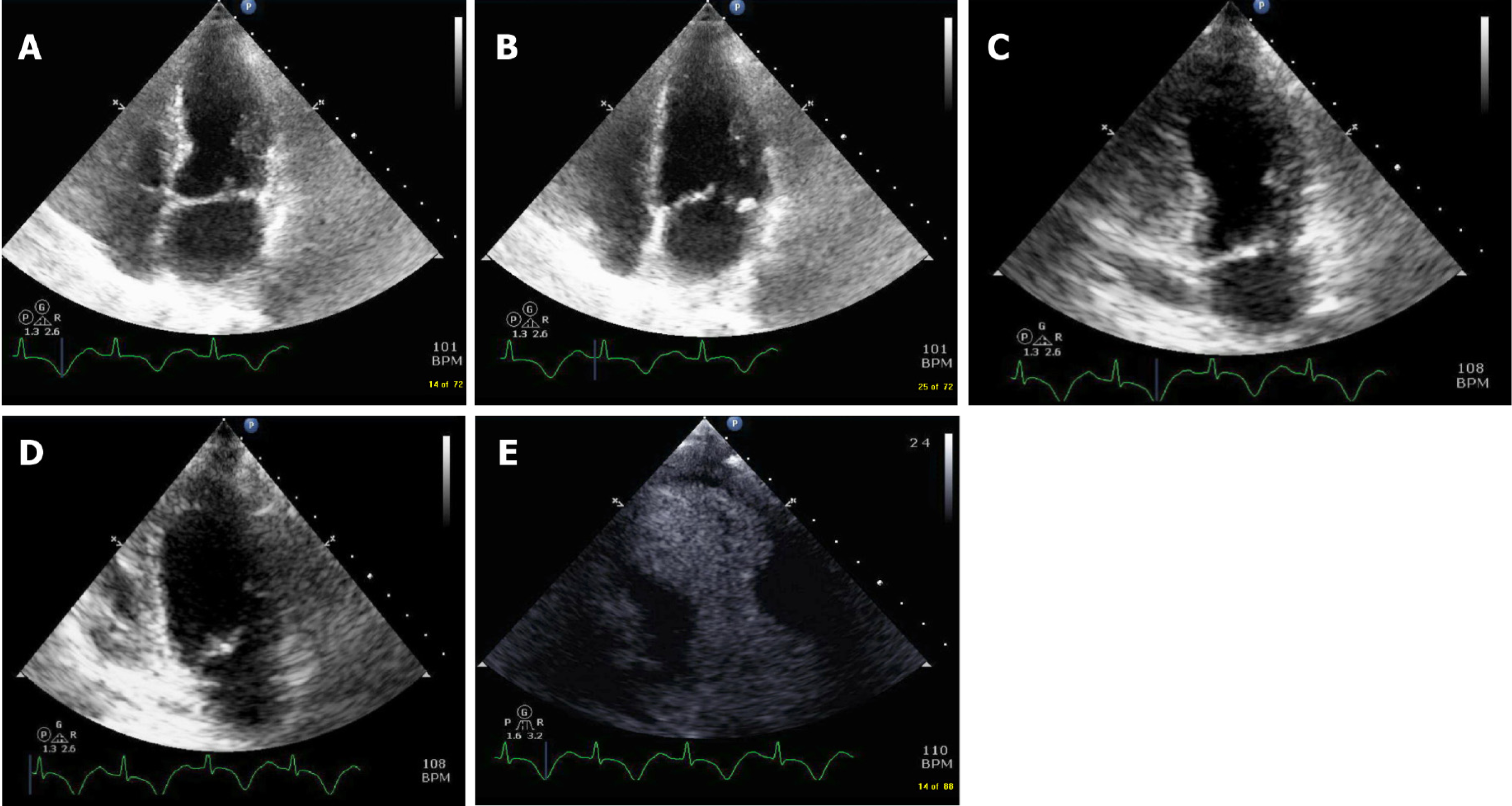
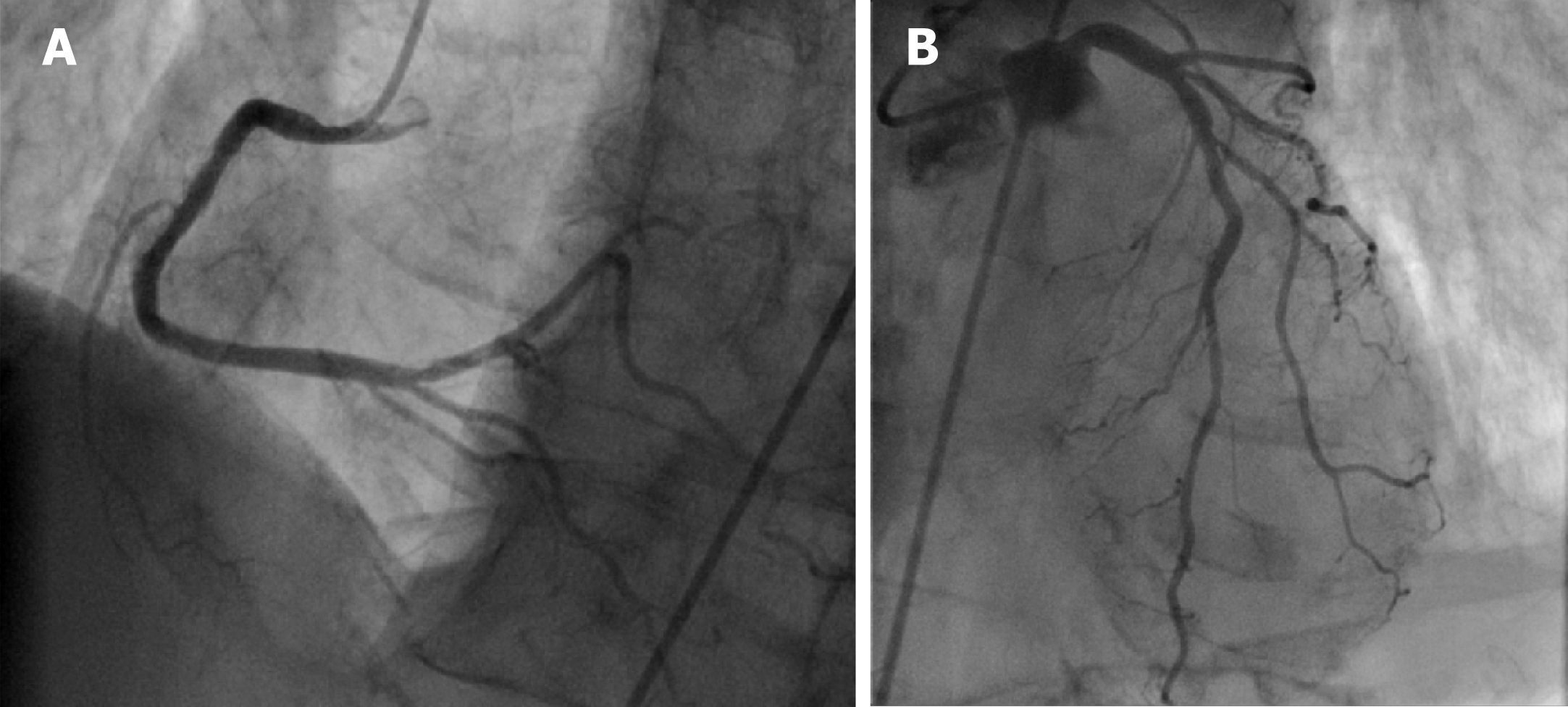
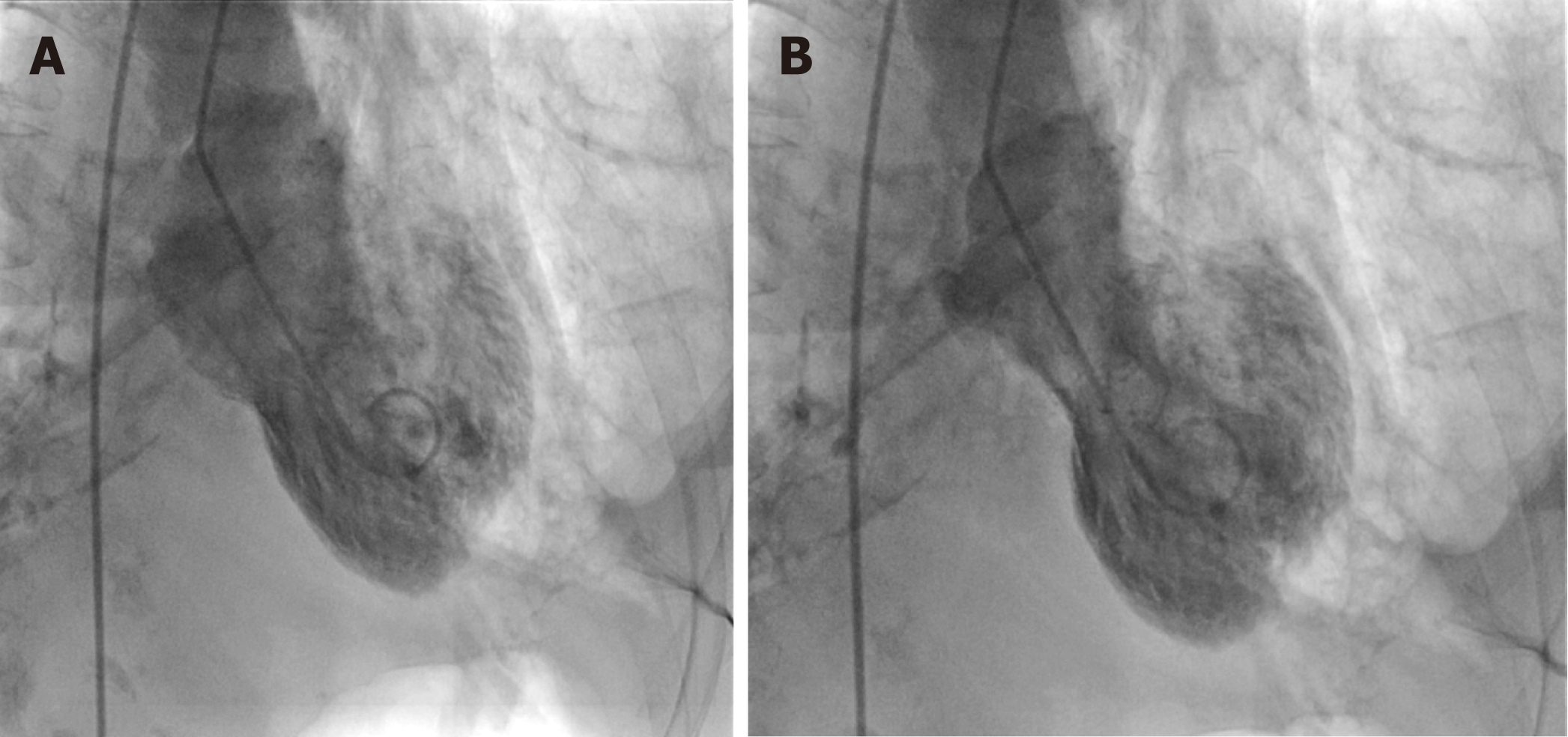
A 2-D echocardiogram was done which showed mid and distal septal, anterior, lateral and apical wall akinesis concerning for ischemia in the left anterior descending (LAD) territory (Figure 3). The patient was then agreeable to have the cardiac angiogram 3 days after the initial presentation. Cardiac angiogram showed patent RCA stent with only mild luminal irregularities noted in the RCA. Left main was angiographically normal, as was the left circumflex. Mild to moderate stenotic lesions were noted in LAD, Diagonal 1 and Ramus Intermedius (Figure 4). A Left ventriculogram revealed hyperkinetic basal segments and akinesis of the apex and periapical segments consistent with TCM (Figure 5).
Based on the findings of the left ventriculogram, the LHC, and the EKG findings the patient was diagnosed with TCM.
The patient was treated for COPD exacerbation. Her breathing improved, and she was back to her baseline 2 liters oxygen use. She was discharged to a long term acute care facility with medications ASA 81mg, Atorvastatin 80 mg, carvedilol 12.5 mg BID and losartan 25 mg. Her inhalers included tiotropium, fluticasone-salmeterol and ipratropium-albuterol. The patient was also started on sertraline 50 mg and instructed to continue her home medication of lorazepam 0.5 mg every 6 h as needed for anxiety.
Follow up Echo and EKG were planned; however, patient had passed away due to worsening of the pulmonary disease.
The Mayo Clinic diagnostic criteria, proposes that 4 criteria must be met in order to diagnose TCM: These criteria are, transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments, new ECG changes mimicking acute MI, absence of angiographic evidence of obstructive coronary disease, and absence of pheochromocytoma and myocarditis[2].
It has been widely suggested that a bronchogenic sub type of TCM exists[3]. Although not as common, there have been some reported cases of TCM in the setting of COPD or asthma[4,5]. Some authors even estimate that pulmonary pathologies are suspected to be found in as high as 44% of TCM cases[6], thus justifying the creation of a separate classification as a bronchogenic subtype. The disproportionate predominance of sympathetic activity during a COPD exacerbation has been noted as a possible trigger for TCM[4]. Rajwani et al[3] described 5 specific cases of bronchogenic TCM and noted some distinguishing features. The absence of chest pain, as with our patient, is noted as a main distinguishing feature of the bronchogenic subgroup of TCM. Progressive dyspnea was also a commonality noted in all 5 cases; this was also present in our patient.
TCM is commonly seen in postmenopausal women, as with our patient[2]. Also in the setting of TCM, wall motion abnormalities are seen to extend beyond the distribution pattern of any single epicardial coronary artery, as seen in our case report[2]. Though TCM is thought to be indistinguishable from ACS on the basis of EKG findings, Madias et al[7] described a noticeably low voltage and attenuated QRS complexes in association with TCM seen in over 90% of the EKGs reviewed for published literature of TCM cases. Since then, many other cases have been reported showing marked QRS complex attenuation in the setting of TCM. In our case, a previous EKG from 12 wk before the patient presentation was available for comparison (Figures 1 and 2). Low QRS voltage (LQRSV), which is defined as ≤ 5 mm in limb leads and/or ≤ 10 mm in precordial leads, and significant attenuation of QRS complexes was appreciated. The likely mechanisms of this phenomenon was explained by author Madias who explored myocardial edema versus counterbalancing of depolarization vectors as the likely mechanisms and concluded that myocardial edema is the most likely cause of the LQRSV appreciated in EKGs of TCM patients[7]. This was supported by review of multiple TCM cases where patients had cardiac MRI performed that revealed myocardial edema[7]. Madias used Ohm’s law (Voltage = Current x Resistance) to explain how changes in the resistance of the electric conductor caused by myocardial edema can account for this phenomenon of LQRSV and attenuation of the amplitude of the QRS complex (AAQRS) since anything that alters resistance or current will result in changes in voltage[7]. Extracardiac pathologies such as pulmonary congestion and pleural effusion, would also influence these changes[7].
TCM is a transient reversible systolic dysfunction and is estimated to be the culprit in 1%-2% of patient presenting with clinical symptoms of a ACS[2]. These patients do not require treatment with heparin drip and antiplatelet therapy thus it is important for clinicians to have a high level of suspicion to identify the correct etiology. As suggested by author Madias, utilizing EKG changes can aid in early identification of TCM and differentiation of TCM from ACS.
Though traditionally TCM was thought to be indistinguishable from ACS, many new case reports and papers have discussed using novel EKG criteria to aid in early recognition of TCM; this case exemplifies the characteristic EKG changes seen in TCM.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fabbian F, Rostagno C S-Editor: Ji FF L-Editor: A E-Editor: Wu YXJ
| 1. | Demirelli S, Ermis E, Hatem E, Uslu A, Askin L. Focal mid-ventricular anterior ballooning: An unusual pattern of Takotsubo cardiomyopathy. Intractable Rare Dis Res. 2015;4:108-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Madhavan M, Prasad A. Proposed Mayo Clinic criteria for the diagnosis of Tako-Tsubo cardiomyopathy and long-term prognosis. Herz. 2010;35:240-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 206] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 3. | Rajwani A, Adam Z, Hall JA. Bronchogenic stress cardiomyopathy: a case series. Cardiology. 2015;130:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Katsa I, Christia P, Massera D, Faillace R. Recurrent Stress Cardiomyopathy During COPD Exacerbation: Are Beta-adrenergic Agonists Only to Blame? Cureus. 2017;9:e1166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Manfredini R, Fabbian F, Giorgi AD, Pala M, Menegatti AM, Parisi C, Misurati E, Tiseo R, Gallerani M, Salmi R, Bossone E. Heart and lung, a dangerous liaison-Tako-tsubo cardiomyopathy and respiratory diseases: A systematic review. World J Cardiol. 2014;6:338-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Hertting K, Krause K, Härle T, Boczor S, Reimers J, Kuck KH. Transient left ventricular apical ballooning in a community hospital in Germany. Int J Cardiol. 2006;112:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Madias JE. Transient attenuation of the amplitude of the QRS complexes in the diagnosis of Takotsubo syndrome. Eur Heart J Acute Cardiovasc Care. 2014;3:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 148] [Article Influence: 12.3] [Reference Citation Analysis (0)] |