Published online Jan 26, 2019. doi: 10.4330/wjc.v11.i1.38
Peer-review started: August 23, 2018
First decision: October 4, 2018
Revised: November 1, 2018
Accepted: January 3, 2019
Article in press: January 4, 2019
Published online: January 26, 2019
Processing time: 156 Days and 21.2 Hours
Familial dilated cardiomyopathy (FDCM) account for 20%-30% of non-ischemic cardiomyopathies (NICM). Previous published data showed that some patients with FDCM tend to have rapidly progressive disease; however, five-year mortality was not significantly different in the familial and non-familial forms of NICM with optimal medical therapy.
To better define the characteristics and clinical outcomes of FDCM patients listed for heart transplantation (HT).
We queried the United Network for Organ Sharing Registry to identify FDCM patients listed for HT between January 2008 and September 2015 and compared them to NICM and ischemic cardiomyopathy (ICM) patients. We included all patients ≥ 18 years old and we separated patients to three groups: FDCM, NICM and ICM. Chi-square test was used to compare between categorical variables, the t-test was used to compare between continues variables, and Cox-proportional hazards model was used to perform time-dependent survival analyses.
Of the 24809 adults listed for HT, we identified 677 patients (2.7%) with the diagnosis of FDCM. Compared to patients with NICM and ICM, FDCM patients were younger (FDCM 43.9 ± 13.5 vs NICM 50.9 ± 12.3, P < 0.001, vs ICM 58.5 ± 8.1, P < 0.001), more frequently listed as status 2 (FDCM 35.2% vs NICM 26.5%, P < 0.001), with significantly lower left ventricular assist device (LVAD) utilization (FDCM 18.4% vs NICM 25.1%, P < 0.001; vs ICM 25.6%, P < 0.001), but higher use of total artificial heart (FDCM 1.3% vs NICM 0.6%, P = 0.039; vs ICM 0.4%, P = 0.002). Additionally, patients with FDCM were less frequently delisted for clinical deterioration or death and more likely to be transplanted compared to those with NICM [hazard ratio (HR): 0.617, 95% confidence interval (CI): 0.47-0.81; HR: 1.25, 95%CI: 1.14-1.37, respectively], and ICM (HR: 0.5, 95%CI: 0.38-0.66; HR: 1.18, 95%CI: 1.08-1.3, respectively). There was more frequent rejection among patients with FDCM (FDCM 11.4% vs NICM 9.8%, P = 0.28; vs ICM 8.4%, P = 0.034). One, three, and five post-transplant survival of patients with FDCM (91%, 88% and 80%) was similar to those with NICM (91%, 84%, 79%, P = 0.225), but superior to those with ICM (89%, 82%, 75%, P = 0.008), respectively.
End-stage FDCM patients are more likely to be transplanted, more likely to have early rejection, and have similar or higher survival than patients with other cardiomyopathies.
Core tip: Familial dilated cardiomyopathy (FDCM) can lead to end-stage heart failure requiring heart transplantation (HT). There is little contemporary information on progression, circulatory mechanical support use, and HT outcomes of these patients. We aimed to define the characteristics and outcomes of FDCM patients and to compare FDCM to non-ischemic cardiomyopathy (NICM) and ischemic cardiomyopathy (ICM) patients listed for HT. FDCM patients were younger, more frequently listed as status 2, and more likely to be transplanted. There was more frequent rejection among patients with FDCM compared to ICM. Post-transplant survival of FDCM patients was similar to NICM, but superior to ICM patients.
- Citation: Khayata M, Al-Kindi SG, Oliveira GH. Contemporary characteristics and outcomes of adults with familial dilated cardiomyopathy listed for heart transplantation. World J Cardiol 2019; 11(1): 38-46
- URL: https://www.wjgnet.com/1949-8462/full/v11/i1/38.htm
- DOI: https://dx.doi.org/10.4330/wjc.v11.i1.38
Familial dilated cardiomyopathy (FDCM) account for 20%-30% of non-ischemic cardiomyopathies (NICM)[1-3]. They are most often inherited in a Mendelian autosomal dominant fashion, although autosomal recessive or X-linked transmission exists[4]. Therefore, first-degree relatives have a higher risk of developing the disease[5]. In the United States, around 26% of patients listed for heart transplantation (HT) in the United Network for Organ Sharing (UNOS) Registry are diagnosed with FDCM[6]. Most previous outcome studies of NICM have not studied FDCM as a separate entity[2,7], perhaps because of the challenge in identifying these patients[2]. To make the diagnosis of FDCM, patients should have two or more affected relatives with NICM or a relative of a NICM patient with unexplained sudden death before the age of 35 years[8,9]. Previous published data showed that some patients with FDCM tend to have rapidly progressive disease[1,2], however, five-year mortality was not significantly different in the familial and non-familial forms of NICM with optimal medical therapy[2,3]. Similarly, mechanical circulatory support (MCS) utilization and HT outcomes have not well studied in FDCM patients and most available data are derived from relatively small cohorts and case reports. In this study, we used a large, contemporary, nationwide database to investigate the clinical characteristics, natural history, MCS use, and HT outcomes of patients with end-stage heart failure due to FDCM.
We used the thoracic transplantation files from the UNOS Registry contracted with the Health Resources and Services Administration. UNOS includes transplantation information on listed patients in all centers across the United States. Data are collected at different time points: at listing, before transplantation, and continually after transplantation. The listing center is responsible for providing the data. Data is used to match patients with donors, for administrative purposes, and for research reporting. The UNOS registry includes data on patient demographics, cause of cardiomyopathy, implanted devices, causes of removal from wait list, hemodynamics, comorbid conditions, listing status, laboratory tests, donor demographics, laboratory and other testing, post-transplantation complications [rejection, infection, kidney failure, length of stay (LOS)], vital status, and cause of death. The registry is continuously audited with strict quality control[10]. Data included in the UNOS are extracted from the transplant candidate registration form, which is filled at time of transplantation; and transplant recipient follow-up form, which is filled at follow-up. At the time of analysis, the database included 99177 patients listed for HT (1985-2015).
We included adults (≥ 18 years old), listed for HT with a diagnosis of idiopathic dilated cardiomyopathy “Dilated myopathy: idiopathic”, FDCM “Dilated Myopathy: Familial” and ischemic cardiomyopathy (ICM) “Dilated Myopathy: Ischemic”, between January 1st, 2008 to September 30th, 2015. We separated patients to three groups: FDCM, NICM and ICM and compared them. Additional cases were identified in the diagnosis free text variable. We compared their baseline characteristics, MCS utilization, and post-transplant outcomes to patients with the diagnosis of ICM and NICM.
All analyses were performed using Statistical Package for Social Sciences (SPSS, version 19.0; SPSS Inc, Chicago, IL). The primary outcomes of this study were waitlist mortality/delisting for clinical deterioration, and post-transplantation mortality among patients who undergo transplantation. Secondary outcomes were as follows: delisting due to improvement, transplant, post-transplantation stroke, post-transplantation permanent pacemaker implantation, post-transplantation acute rejection, post-transplantation dialysis, and LOS for index transplant hospitalization.
Categorical variables were presented as numbers and percentages and were compared using Pearson χ2 test. Continuous variables were presented as means and standard deviations and were compared with Student t-test and. Survival analyses were done using Kaplan-Meier method with log-rank test and adjusted survival using Cox-proportional-hazard model. Variables that were significant in univariable models (P < 0.05) were included in the multivariable model. All tests were two sided. P < 0.05 was considered statistically significant. No assumptions were used for missing data. Institutional review board approval was not required because only deidentified data sets were used for this analysis. The statistical review of the study was performed by a biomedical statistician.
Of the 24809 adults listed for HT between January 2008 and September 2015, we identified 677 patients (2.7%) with the diagnosis of FDCM, and compared them with 8416 patients (33.9%) with NICM, and 8301 (33.5%) patients with ICM patients (Table 1).
| NICM (n = 8416) | FDCM (n = 677) | P value | ICM (n = 8301) | P value | |
| Age at listing | 50.9 ± 12.3 | 43.9 ± 13.5 | < 0.001 | 58.5 ± 8.1 | < 0.001 |
| Male gender | 6113 (72.6) | 444 (65.6) | < 0.001 | 7212 (86.9) | < 0.001 |
| Ethnicity | < 0.001 | < 0.001 | |||
| White | 4609 (54.8) | 444 (65.6) | 6411 (77.2) | ||
| Black | 2776 (33.0) | 159 (23.5) | 976 (11.8) | ||
| Hispanic | 705 (8.4) | 54 (8.0) | 575 (6.9) | ||
| Asian | 223 (2.6) | 14 (2.1) | 269 (3.2) | ||
| Other or unknown | 103 (1.2) | 6 (0.9) | 70 (0.8) | ||
| Initial status | < 0.001 | 0.956 | |||
| 1A | 1918 (22.8) | 147 (21.7) | 1823 (22.0) | ||
| 1B | 4023 (47.8) | 273 (40.3) | 3415 (41.1) | ||
| 2 | 2227 (26.5) | 238 (35.2) | 2831 (34.1) | ||
| 7 | 248 (2.9) | 19 (2.8) | 232 (2.8) | ||
| Therapies | |||||
| Inotropes | 2947 (35) | 233 (34.4) | 0.769 | 2386 (28.7) | 0.002 |
| ECMO | 52 (0.6) | 4 (0.6) | 1.0 | 87 (1.0) | 0.320 |
| IABP | 395 (4.7) | 21 (3.1) | 0.056 | 403 (4.9) | 0.038 |
| Mechanical ventilation | 141 (1.7) | 10 (1.5) | 0.875 | 209 (2.5) | 0.118 |
| LVAD | 2104 (25.1) | 124 (18.4) | < 0.001 | 2116 (25.6) | < 0.001 |
| BiVAD | 153 (1.8) | 8 (1.2) | 0.288 | 157 (1.9) | 0.233 |
| TAH | 50 (0.6) | 9 (1.3) | 0.039 | 31 (0.4) | 0.002 |
| ICD | 6985 (83.5) | 562 (83.8) | 0.914 | 6652 (80.9) | 0.073 |
| Laboratory values | |||||
| Creatinine | 1.4 ± 1.0 | 1.3 ± 0.7 | 0.008 | 1.4 ± 0.9 | < 0.001 |
| Albumin | 3.7 ± 0.7 | 3.8 ± 0.6 | 0.001 | 3.7 ± 0.7 | 0.001 |
| Bilirubin | 1.1 ± 1.8 | 1.1 ± 1.0 | 0.578 | 1.0 ± 2.0 | 0.540 |
| PRA class I | 7.1 ± 18.6 | 7.2 ± 18.5 | 0.892 | 5.7 ± 16.2 | 0.084 |
| PRA class II | 4.8 ± 15.7 | 5.2 ± 16.2 | 0.645 | 3.4 ± 12.6 | 0.012 |
| Hemodynamics | |||||
| PA systolic pressure (mmHg) | 44.3 ± 13.9 | 42.7 ± 13.2 | 0.004 | 44.8 ± 15.2 | 0.001 |
| PA diastolic pressure (mmHg) | 22.1 ± 8.9 | 21.7 ± 8.7 | 0.266 | 20.8 ± 8.6 | 0.013 |
| PA mean pressure (mmHg) | 30.5 ± 10.2 | 29.7 ± 9.8 | 0.052 | 29.8 ± 10.5 | 0.821 |
| PCWP (mmHg) | 20.5 ± 9.0 | 20.4 ± 8.5 | 0.735 | 19.7 ± 8.9 | 0.081 |
| CO (L/min) | 4.3 ± 1.4 | 4.1 ± 1.3 | 0.011 | 4.5 ± 1.3 | < 0.001 |
Patients with FDCM were younger (mean age: 43.9 ± 13.5 vs NICM 50.9 ± 12.3, P < 0.001; vs ICM 58.5 ± 8.1; P < 0.001) and less predominantly men (FDCM 65.6% vs NICM 72.6%, P < 0.001; vs ICM 86.9%, P < 0.001). FDCM patients were more often listed as a status 2 (FDCM 35.2% vs NICM 26.5%, P < 0.001 vs, ICM 34.1%, P = 0.956), had significantly less left ventricular assist device (LVAD) use (FDCM 18.4% vs NICM 25.1%, P < 0.001; vs ICM 25.6%, P < 0.001) but more use of total artificial heart (TAH) (FDCM 1.3% vs NICM 0.6%, P = 0.039; vs ICM 0.4%, P = 0.002), had lower creatinine (FDCM 1.3 ± 0.7 vs NICM 1.4 ± 1.0, P = 0.008; vs ICM 1.4 ± 0.9, P < 0.001), had higher albumin (FDCM 3.8 ± 0.6 vs NICM 3.7 ± 0.7, P = 0.001; vs ICM 3.7 ± 0.7, P = 0.001), had lower pulmonary artery systolic pressure (FDCM 42.7 ± 13.2 vs NICM 44.73 ± 13.9, P = 0.004; vs ICM 44.8 ± 15.2; P = 0.001) , and lower cardiac output (FDCM 4.1 ± 1.3 vs NICM 4.3 ± 1.4, P = 0.011; vs ICM 4.5 ± 1.3, P < 0.001) (Table 1).
Of 677 FDCM patients, 33 patients (4.8%) died while waiting HT, 7 patients (1%) were delisted for improvement, 20 patients (2.9%) were delisted for deterioration, 470 patients (69%) were transplanted, 3 patients (0.4%) refused transplantation, and 13 patients (1.9%) transferred to another center. Causes of Death in FDCM patients were: multiple organ failure [11 patients (2%)], cardiovascular [6 patients (1%)], cerebrovascular [6 patients (1%)], infections [3 patients (< 1%)], respiratory [2 patients (< 1%)], hemorrhage [1 patient (< 1%)], and other [4 patients (< 1%)].
Patients with FDCM were less likely to die compared to NICM [hazard ratio (HR): 0.720, 95% confidence interval (CI): 0.507-1.023] and ICM (HR: 0.61, 95%CI: 0.43-0.86), less likely to be delisted due to deterioration compared to NICM (HR: 0.49, 95%CI: 0.32-0.78) and ICM (HR: 0.39, 95%CI: 0.25-0.6), less likely to die or to be delisted due to deterioration compared to NICM (HR: 0.62, 95%CI: 0.47-0.81) and ICM (HR: 0.5, 95%CI: 0.38-0.66), less likely to be delisted due to improvement compared to NICM (HR: 0.28, 95%CI: 0.13-0.59) and ICM (HR: 0.35, 95%CI: 0.16-0.74), and more likely to be transplanted compared to NICM (HR: 1.25, 95%CI: 1.14-1.37) and ICM (HR: 1.83, 95%CI: 1.08-1.3) while waiting HT (Table 2).
| Outcome | FDCM vs NICM | FDCM vs ICM |
| HR (95%CI), P value | HR (95%CI), P value | |
| Waitlist mortality | 0.720 [0.507-1.023], P = 0.067 | 0.609 [0.429-0.864], P = 0.005 |
| Delisting due to deterioration | 0.499 [0.319-0.781], P = 0.002 | 0.387 [0.248-0.604], P < 0.001 |
| Waitlist mortality or delisting due to deterioration | 0.617 [0.468-0.813], P = 0.001 | 0.501 [0.381-0.659], P = 0.001 |
| Delisting due to improvement | 0.277 [0.131-0.588], P = 0.001 | 0.347 [0.163-0.735], P = 0.006 |
| Transplant | 1.248 [1.135-1.373], P < 0.001 | 1.183 [1.076-1.302], P = 0.001 |
Factors associated with waitlist mortality or delisting for FDCM on multivariate analysis patients were: mechanical ventilation (HR: 3.69, 95%CI: 1.02-13.36), creatinine (HR: 1.38, 95%CI: 1.21-1.57), and UNOS status 1A (Table 3).
| Univariable HR (95%CI) | P value | Multivariable HR (95%CI) | P value | |
| Age at listing | 0.082 | |||
| Gender | 0.413 | |||
| Ethnicity | 0.712 | |||
| UNOS listing status | < 0.001 | 0.001 | ||
| 1b vs 1a | 0.431 [0.231-0.805] | 0.606 [0.305-1.204] | ||
| 2 vs 1a | 0.160 [0.073-0.350] | 0.176 [0.073-0.424] | ||
| 7 vs 1a | 0.852 [0.252-2.886] | 1.326 [0.373-4.707] | ||
| Inotropes | 0.110 | |||
| ECMO | 0.229 | |||
| IABP | 3.987 [1.575-10.090] | 0.004 | 0.124 | |
| Mechanical Ventilation | 4.294 [1.333-13.831] | 0.015 | 3.694 [1.022-13.360] | 0.046 |
| VAD | 0.009 | 0.519 | ||
| LVAD vs no VAD | 1.084 [0.540-2.179] | |||
| BiVAD vs no VAD | 7.636 [2.342-24.900] | |||
| TAH vs no VAD | 1.724 [0.236-12.600] | |||
| ICD | 0.392 | |||
| Creatinine | 1.275 [1.142-1.422] | < 0.001 | 1.377 [1.211-1.566] | < 0.001 |
| PASP | 1.022 [1.002-1.043] | 0.033 | 0.169 | |
| PADP | 0.067 | |||
| PAMP | 0.097 | |||
| PCWP | 0.387 | |||
| CO | 0.093 | |||
| List year | 0.282 |
There was no significant difference between FDCM and other types of cardiomyopathies in stroke rates (FDCM 1.4% vs NICM 2.3%, P=0.239; vs ICM 3.0%; P = 0.051), permanent pacemaker placement (FDCM 3.6% vs NICM 3.4%, P = 0.785, vs ICM 3.3%, P = 0.681), rejection rates (FDCM 11.4% vs NICM 9.8%, P = 0.283), dialysis need (FDCM 9.7% vs NICM 9.5%, P = 0.866; vs ICM 10.2%, P = 0.806), and LOS (FDCM 17.3 ± 13.1 vs NICM 19 ± 22, P = 0.105) after HT. When compared to ICM, FDCM patients had significantly higher early rejection rates (FDCM 11.4% vs ICM 8.4%, P < 0.034), and lower LOS (FDCM 17.3 ± 13.1 vs ICM 20.7 ± 25.4, P < 0.006) (Table 4).
| NICM | FDCM | P-value | ICM | P value | |
| Stroke | 114 (2.3) | 6 (1.4) | 0.239 | 147 (3.0) | 0.051 |
| Permanent pacemaker | 171 (3.4) | 16 (3.6) | 0.785 | 164 (3.3) | 0.681 |
| Treated for rejection | 496 (9.8) | 51 (11.4) | 0.283 | 416 (8.4) | 0.034 |
| Dialysis | 476 (9.5) | 43 (9.7) | 0.866 | 507 (10.2) | 0.806 |
| LOS (d) | 19 ± 22 | 17.3 ± 13.1 | 0.105 | 20.7 ± 25.4 | 0.006 |
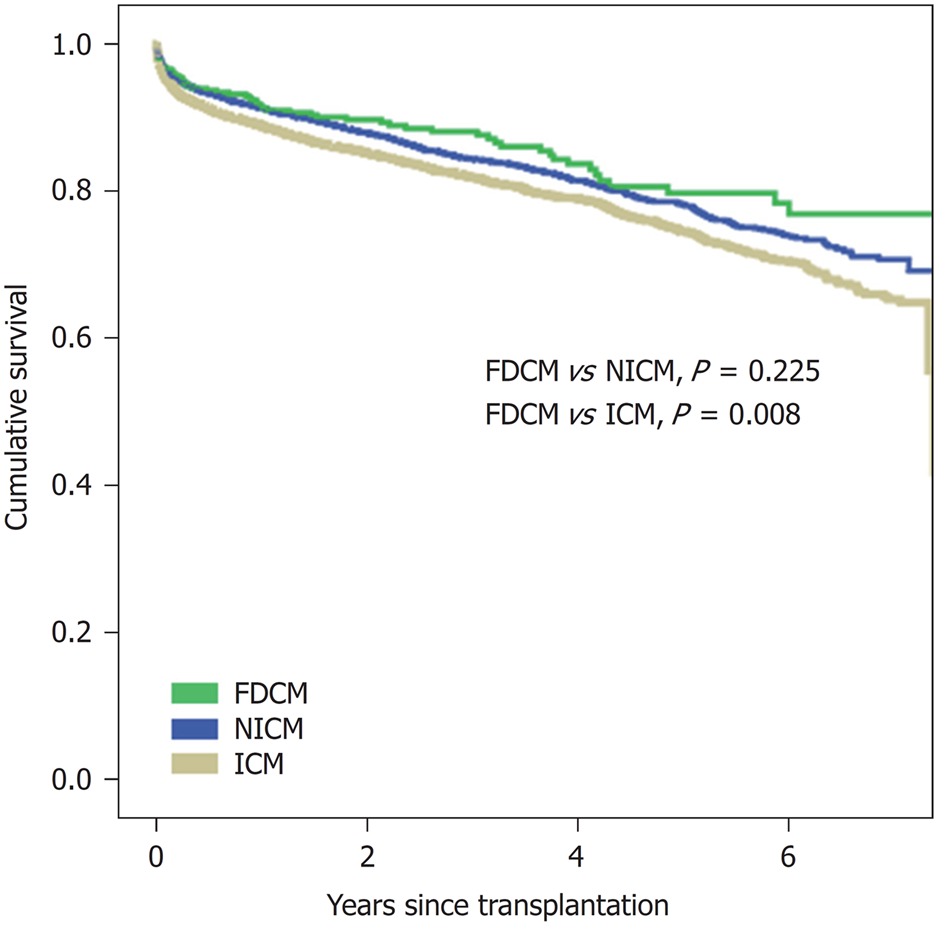
One, three, and five-year post-transplant survival were as follows: FDCM (91%, 88%, and 80%), NICM (91%, 84%, 79%), and ICM (89%, 82%, 75%), respectively, with no statistically significant differences between FDCM and NICM (P = 0.225) but higher survival compared to ICM (P = 0.008)(Figure 1).
Herein we describe the largest contemporary cohort of patients with end-stage heart failure from FDCM listed for HT and report on their clinical characteristics and outcomes.
Our data showed that around 2.7% of patients listed for HT have FDCM, considerably lower than the overall prevalence of FDCM. The low prevalence of the disease among patients listed for HT in our cohort might be explained by the fact that FDCM is often underdiagnosed[6].
We found that patients with FDCM who are listed for HT tended to be younger and less predominantly males compared to ICM and NICM patients, which is consistent with previous literature[7]. In addition, we found that the diagnosis of FDCM is associated with less acuity at listing, as FDCM patients were more likely to be listed as a status 2, less likely to need LVAD, and more likely to be transplanted. When FDCM patients do need MCS, they more often need biventricular support, as is illustrated by their higher usage of TAHs.
We also presented the clinical course of FDCM patients in the transplant waitlist and we showed that FDCM patients were less likely to deteriorate or die, but also less likely to improve compared to other heart failure patients. As a result, FDCM patients were more likely to be transplanted. This suggests that listed FDCM patients can be safely followed until a suitable donor is available, obviating the need for MCS as a bridge to transplant.
We also investigated transplantation outcomes in FDCM patients, which might be a concern on these patients given the fear of early rejection, as they tend to be younger with active immune system[11,12]. Previously published data compared between FDCM and non-FDCM patients who are listed for HT and showed that rejection incidence is similar in both groups[1], however, immunosuppression therapies have significantly changed since that study. We found that FDCM patients were more likely to be treated for post transplantation rejection (11.4%) compared to ICM (8.4%). That maybe explained, in part, by the fact that FDCM patients were younger and likely to have more active immune system compared to older patients[11-14].
To the best of our knowledge, our study is the largest contemporary study that compared FDCM to NICM and ICM, and followed patients after HT. We found that FDCM patients had higher survival at one, three, and five years after HT compared to ICM patients, with no significant difference compared to NICM patients. As FDCM patients were less likely to have hepatic or renal dysfunction, that may explain the higher rates of survival after HT in this group[15]. Besides that, ICM patients tend to have more comorbidities compared to patients with NICM, which may explain the higher mortality rate in ICM group[16]. Valentine et al. compared between FDCM and NICM and found that FDCM patients had higher survival compared to NICM patients 5 years after HT, however, the large discrepancy in sample size between the 2 groups in that study makes statistical comparison invalid[1].
Our study presents the clinical outcomes of patients with end-stage heart failure from FDCM listed for HT. The outcomes of our study may help providers in making clinical decisions while following these patients before and after HT.
Limitations of our study are mainly associated with registry-based analysis with a limited sample size of patients with FDCM, due to underestimation of the disease[6]. Therefore, our results should be interpreted in this context. Although regularly onsite audits are performed for the UNOS registry, the actual quality of the patient data has not been subject to a comprehensive audit[10]. Second, this database did not address how the diagnosis of FDCM was made and whether relatives of patients with FDCM had echocardiography to confirm the diagnosis of FDCM. Third, this registry did not mention the type of inotrope, doses, and other treatments such as: inhaled nitric oxide, or prostacyclins that were used while awaiting transplantation. Fourth, the database is missing the reason of mechanical ventilation. Although the difference of its incidence was not significant, we did not know if patients were intubated due to a cardiac etiology or any other reason. Fifth, graft failure rates might be underestimated across the groups, as its occurrence requires inotropes or mechanical ventilation support after transplantation, which is not captured by the UNOS database. Finally, as listing practices and peri-transplant care may be different in different countries, our results may not be applicable to transplant centers in other countries because UNOS is a US-based registry.
In conclusion, patients with end-stage FDCM are listed at a younger age, most often as status 2, and more frequently transplanted than patients with other cardiomyopathies. Although FDCM is associated with more frequent early rejection, survival of these patients is similar or better than other heart transplant recipients.
Familial dilated cardiomyopathy (FDCM) is a sub-type of non-ischemic cardiomyopathy (NICM) that may lead to end-stage heart failure requiring heart transplantation (HT). This group of patients tends to develop heart failure at earlier age and they are more likely to have less comorbidity, which suggest they may have better outcomes after HT. Although characteristics of FDCM patients with end-stage heart failure have been reported, the outcomes of FDCM patients listed for HT were not described.
As the outcomes of FDCM listed for HT patients were not studied, we used a large database to compare FDCM to ischemic cardiomyopathy (ICM) and NICM patients who are listed for HT. Our results may help to better understand the clinical course of FDCM patients while they are awaiting HT and their outcomes after being transplanted.
The objective of this study was to compare FDCM to ICM and NICM patients who are listed for HT and describe their clinical course while awaiting HT and their post-HT outcomes.
We identified patients who are listed for HT using the United Network for Organ Sharing Registry. We divided patients to three groups: ICM, NICM, and FDCM, and compared clinical outcomes of FDCM to ICM and NICM patients who are listed for HT.
FDCM patients were younger, less likely to be males, more likely to be listed as status 2, less likely to require mechanical support, but more likely to need total artificial heart. While awaiting HT, FDCM patients were less likely to die compared to ICM [HR 0.609 (0.429-0.864)], less likely to be delisted due to deterioration compared to ICM [0.387 (0.248-0.604)] and NICM [0.499 (0.319-0.781)], less likely to die or to be delisted due to deterioration compared ICM [0.501 (0.381-0.659)] and NICM [0.617 (0.468-0.813)], less likely to be delisted due to improvement compared to ICM [0.347 (0.163-0.735)] and NICM [0.277 (0.131-0.588)], and more likely to be transplanted compared to ICM [1.183 (1.076-1.302)] and NICM [1.248 (1.135-1.373)]. After HT, FDCM patients were more likely to have early rejection compared to ICM (FDCM 11.4% vs ICM 8.4%; P < 0.034), but more likely to survive (91%, 88%, and 80%) compared to ICM (89%, 82%, and 75%) at 1, 3, and 5 years, respectively.
Patients with end-stage heart failure due to FDCM are more likely to be transplanted compared to NICM and ICM. After HT, they are more likely to develop early rejection, but more likely to survive compared to ICM patients.
This study may help providers in making clinical decisions for patients with end-stage heart failure due to FDCM while waiting and after HT.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Kharlamov AN, Vermeersch P, Traykov V, Amrousy DE S- Editor: Dou Y L- Editor: A E- Editor: Song H
| 1. | Valantine HA, Hunt SA, Fowler MB, Billingham ME, Schroeder JS. Frequency of familial nature of dilated cardiomyopathy and usefulness of cardiac transplantation in this subset. Am J Cardiol. 1989;63:959-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Michels VV, Driscoll DJ, Miller FA, Olson TM, Atkinson EJ, Olswold CL, Schaid DJ. Progression of familial and non-familial dilated cardiomyopathy: long term follow up. Heart. 2003;89:757-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Martins E, Cardoso JS, Campelo M, Amorim S, Moura B, Maciel MJ, Gonçalves FR. Survival of patients with familial dilated cardiomyopathy on optimal heart failure therapy. Rev Port Cardiol. 2009;28:263-268. [PubMed] |
| 4. | Monserrat L, Hermida M, Bouzas B, Mosquera I, Mahon N, Peteiro J, Alvarez N, Penas-Lado M, Crespo M, Castro-Beiras A. Familial dilated cardiomyopathy in patients transplanted for idiopathic dilated cardiomyopathy. Rev Esp Cardiol. 2002;55:725-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Baig MK, Goldman JH, Caforio AL, Coonar AS, Keeling PJ, McKenna WJ. Familial dilated cardiomyopathy: cardiac abnormalities are common in asymptomatic relatives and may represent early disease. J Am Coll Cardiol. 1998;31:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 191] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Seidelmann SB, Laur O, Hwa J, Depasquale E, Bellumkonda L, Sugeng L, Pomianowski P, Testani J, Chen M, McKenna W, Jacoby D. Familial dilated cardiomyopathy diagnosis is commonly overlooked at the time of transplant listing. J Heart Lung Transplant. 2016;35:474-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Bahler RC. Assessment of prognosis in idiopathic dilated cardiomyopathy. Chest. 2002;121:1016-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Taylor MR, Carniel E, Mestroni L. Cardiomyopathy, familial dilated. Orphanet J Rare Dis. 2006;1:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 103] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Mestroni L, Maisch B, McKenna WJ, Schwartz K, Charron P, Rocco C, Tesson F, Richter A, Wilke A, Komajda M. Guidelines for the study of familial dilated cardiomyopathies. Collaborative Research Group of the European Human and Capital Mobility Project on Familial Dilated Cardiomyopathy. Eur Heart J. 1999;20:93-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 311] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 10. | Daily OP, Kauffman HM. Quality control of the OPTN/UNOS Transplant Registry. Transplantation. 2004;77:1309; author reply 1309-1309; author reply 1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Tjang YS, van der Heijden GJ, Tenderich G, Körfer R, Grobbee DE. Impact of recipient's age on heart transplantation outcome. Ann Thorac Surg. 2008;85:2051-2055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Sharma G, Hanania NA, Shim YM. The aging immune system and its relationship to the development of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2009;6:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Kilic A, Weiss ES, Allen JG, Conte JV, Shah AS, Baumgartner WA, Yuh DD. Simple score to assess the risk of rejection after orthotopic heart transplantation. Circulation. 2012;125:3013-3021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Marelli D, Laks H, Kobashigawa JA, Bresson J, Ardehali A, Esmailian F, Plunkett MD, Kubak B. Seventeen-year experience with 1,083 heart transplants at a single institution. Ann Thorac Surg. 2002;74:1558-1566; discussion 1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Grimm JC, Shah AS, Magruder JT, Kilic A, Valero V, Dungan SP, Tedford RJ, Russell SD, Whitman GJ, Sciortino CM. MELD-XI Score Predicts Early Mortality in Patients After Heart Transplantation. Ann Thorac Surg. 2015;100:1737-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 16. | Shore S, Grau-Sepulveda MV, Bhatt DL, Heidenreich PA, Eapen ZJ, Hernandez AF, Yancy CW, Fonarow GC. Characteristics, Treatments, and Outcomes of Hospitalized Heart Failure Patients Stratified by Etiologies of Cardiomyopathy. JACC Heart Fail. 2015;3:906-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |