Published online Sep 26, 2018. doi: 10.4330/wjc.v10.i9.119
Peer-review started: April 16, 2018
First decision: June 6, 2018
Revised: July 9, 2018
Accepted: August 26, 2018
Article in press: August 26, 2018
Published online: September 26, 2018
Processing time: 168 Days and 9.9 Hours
We present a modified implantation technique of the Perceval® sutureless aortic valve (LivaNova, London, United Kingdom) that involves the usage of snuggers for the guiding sutures during valve deployment. Both limbs of each guiding suture are pulled through an elastic tube, which is fixed with a Pean clamp, which tightens the sutures and fixes the prosthesis to the aortic annulus during valve deployment. This method proved safe and useful in over 120 cases. Valve implantation was facilitated and the need for manipulation by the assistant or the nurse was eliminated.
Core tip: In this article, we are presenting a modified implantation technique of the Perceval sutureless aortic valve prosthesis to enhance proper positioning of the prosthesis and aid the reproducibility of the implantation procedure. The modification involves using snuggers to fix the valve prosthesis to the aortic annulus during deployment.
- Citation: Mashhour A, Zhigalov K, Szczechowicz M, Mkalaluh S, Easo J, Eichstaedt H, Borodin D, Ennker J, Weymann A. Snugger method - The Oldenburg modification of perceval implantation technique. World J Cardiol 2018; 10(9): 119-122
- URL: https://www.wjgnet.com/1949-8462/full/v10/i9/119.htm
- DOI: https://dx.doi.org/10.4330/wjc.v10.i9.119
Surgery of the aortic valve replacement (AVR) is still recommended in certain patients with aortic valve disease. Two approaches have become quite popular; surgical and trans-catheter aortic valve replacement (SAVR and TAVR, respectively), whereby TAVR is mostly reserved for elderly patients with higher surgical risk[1,2]. Although not considered in the current guidelines, the sutureless variety of SAVR has been proven to reduce the overall surgical risk by significantly reducing operative and cross-clamp times, while demonstrating lower incidence of known complications of TAVR with comparable or even better results, especially in intermediate-risk patients[3-5].
The Perceval valve (Sorin Group Italia Srl, Saluggia, Italy) is a self-anchoring, self-expanding, sutureless, surgical aortic bioprosthesis. The valve leaflets are mounted to an elastic nickel-titanium alloy stent[3]. The stent anchors the valve via six sinusoidal posts to the aortic root at the sinuses of Valsalva, while the valve prosthesis seals the left ventricular outflow tract (LVOT) through an intra-annular and a supra-annular sealing ring. Correctly positioned, the leaflets of the valve prosthesis are aligned with those of the native aortic valve and the inflow ring of the prosthesis lies at the level of the insertion plane of the native leaflets[6]. The intra-annular ring of the Perceval valve prosthesis is supplied with three eyelets to pass guiding sutures which are previously made at the hinge points of the native aortic valve leaflets.
The valve prosthesis is then inserted into the aortic root over these guiding sutures and deployed “hand-held” in position. We describe a modification of this technique, where the prosthesis is virtually “fixed” onto the aortic annulus during deployment, which guarantees correct positioning of the prosthesis and aid the reproducibility of the implantation procedure.
The aortotomy should be in a transverse manner at least 3.5 cm above the aortic annulus to facilitate aortic closures. The native aortic valve is excised as with other SAVR prostheses. Although a complete decalcification of the aortic annulus is not necessary, a regular annular profile is essential for proper sealing. Sizing of the aortic annulus should be performed using the dedicated sizers.
Now, the prepared prosthesis can be put in place. To ensure correct placement and alignment, a suture is made at hinge point of each leaflet perpendicular to the annulus, so that the three sutures are approximately 120° equidistant. The suture points should be 2-3 mm afar from each side of the insertion plane of the leaflets. After each suture is taken, the needle should be cut off and both ends of the thread secured with a clamp.
Each of the guiding sutures is then passed through one of the eyelets of the prosthesis. After that, the valve prosthesis is parachuted into the aorta sliding on the guiding threads which are kept straight with a gentle pull maintaining alignment with the aorta. Correct position of the prosthesis is reached when it is descended until it is stopped at the insertion points of the threads and the commissural struts of the prosthesis are aligned with the native commissures.
The valve is then released in two steps. First, the inflow section is released by rotating the control button on the delivery device until a click is heard and felt. At this stage, it is important to ensure that the sinusoidal struts correspond to the sinuses of Valsalva and that the stent of the prosthesis does not obstruct the coronary ostia. Second, the outflow section is released by withdrawing the sliding sheath off the holder avoiding rotational movement. It is important to keep the holder in an axial position to aorta all the time.
After visual assessment of the correct position and alignment of the prosthesis, patency of the coronary ostia and that no annulus is visible below and above the valve inflow ring, the inflow ring should be postdilated (4 atmospheric pressure for 30 s) using a dedicated catheter. While the postdilation balloon is inflated, warm sterile saline is poured within the aortic root to ensure optimal valve sealing and optimized anchoring. The guiding sutures are removed and the aortotomy is closed as usual taking care not to capture the stent of the prosthesis within the closure suture.
Preparations of the prosthesis and the aortic root as well as the sizing procedure and prosthesis selection are similar to the method described above. The guiding sutures are also placed as described. We use 3/0 double-armed poly-propylene sutures. The suture is made with one needle from the LVOT side to the aorta side of the hinge point of each leaflet leaving 2-3 mm on each side as recommended above. The other needle is passed through the eyelet of the Perceval prosthesis before both needles are cut off.
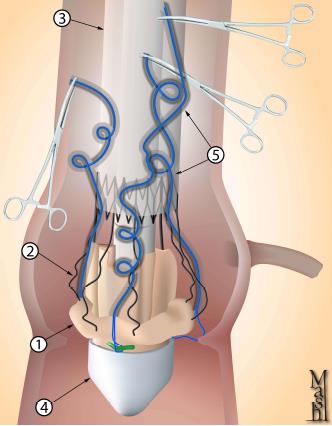
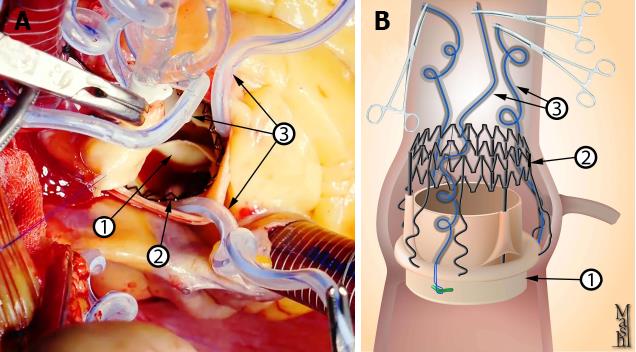
Now, instead of directly securing the thread with a clamp, both ends are passed through an elastic tube making a snugger. While holding the prosthesis holder in place and axial to the aortic root, the snuggers are tightened. While tightening each snugger, both ends of the thread are pulled upwards. This “pull” is partially opposed by a light downward pressure on the prosthesis in the direction of the insertion of the guiding suture. The snugger is then pulled tight and secured with a Pean clamp (Figure 1).
This is repeated with the other two guiding sutures. The assistant should retract the aortic wall slightly open, so that the descent of the elastic tube into the tightened position is done under direct vision. It is important that the snuggers are tight enough; however, care should be taken that the elastic tube ends above the sealing ring of the inflow stent of the prosthesis and not trapped between the ring and the aortic annulus (Figure 2), as this could lead to incomplete deployment of the prosthesis, difficult withdrawal of the elastic tube and, potentially, dislodgement of the prosthesis during withdrawal of the elastic tube.
Next, the prosthesis is deployed in the same fashion described above. In this step, the assistant can help stabilize the prosthesis and hold the aorta open to aid visualization. Checking for correct positioning etc. as well as postdilation and irrigation with warm saline are also performed as described above.
Now, the snuggers a loosened and the elastic tubes are withdrawn. This should be done slowly and under direct vision taking care not to dislodge the prosthesis. The threads are then pulled out carefully. The prosthesis is checked again for proper anchoring and correct seat, and the aortotomy is closed.
As rapid-deployment prosthesis, one of the main benefits of the Perceval prosthesis is reducing operative and cross-clamp times through simplifying the surgical implantation technique. However, absolute stability is required during valve deployment to ensure proper seating of the prosthesis within the aortic root. Otherwise, valve malposition could occur[7].
On the contrary, in the technique described in this work, after tightening the snuggers, the prosthesis and the aortic annulus are fixed together eliminating the need for extra manipulations by the assistant or the nurse, so that the surgeon can self-sufficiently deploy the valve with one hand holding the delivery device and the other hand rotating the control button to release the valve.
Moreover, while tightening each snugger, the surgeon should pay attention to this one guiding suture; a step which is repeated with each suture at a time. On the contrary, the standard technique recommended by the manufacturer requires ensuring that the prosthesis is seated in the right position in respect to the three guiding sutures simultaneously.
According to the manufacturer’s recommendations, traction sutures should be released prior to the deployment of the valve. We did not consider this step necessary as the snuggers would literally fix the valve prosthesis to the aortic annulus at three points forcing it into planarity and thus eliminating any distorting leverage exerted by the traction sutures. The continued presence of the traction sutures allows better visualization of the aortic annulus during prosthesis deployment.
In the manufacturer’s recommendations, in case of a hypoplastic coronary ostium, the first guiding suture should be in the corresponding sinus. We did not encounter this in our case series. We also did not find any reports on the use of Perceval prosthesis in cases with a hypoplastic coronary ostium. Indeed, this should not be problematic. Nevertheless, the modification proposed in this work would add more security to the implantation, as the snuggers push the prosthesis down as far as possible, guaranteeing freedom of the hypoplastic ostium.
The use of snuggers, was reported once to facilitate a total endoscopic AVR[8]. However, to our knowledge, the use of snuggers to fixate the Perceval prosthesis during deployment in the way described in this work has not been described before. Until now, we have used this modification in over 120 patients with 100% primary success and excellent postoperative results.
Manuscript source: Unsolicited Manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Iacoviello M, Dai X, Falconi M S- Editor: Dou Y L- Editor: A E- Editor: Wu YXJ
| 1. | Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e1159-e1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1308] [Cited by in RCA: 1473] [Article Influence: 184.1] [Reference Citation Analysis (0)] |
| 2. | Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739-2791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4598] [Cited by in RCA: 4391] [Article Influence: 548.9] [Reference Citation Analysis (0)] |
| 3. | Fischlein T, Meuris B, Hakim-Meibodi K, Misfeld M, Carrel T, Zembala M, Gaggianesi S, Madonna F, Laborde F, Asch F. The sutureless aortic valve at 1 year: A large multicenter cohort study. J Thorac Cardiovasc Surg. 2016;151:1617-1626.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | Laborde F, Fischlein T, Hakim-Meibodi K, Misfeld M, Carrel T, Zembala M, Madonna F, Meuris B, Haverich A, Shrestha M; Cavalier Trial Investigators. Clinical and haemodynamic outcomes in 658 patients receiving the Perceval sutureless aortic valve: early results from a prospective European multicentre study (the Cavalier Trial)†. Eur J Cardiothorac Surg. 2016;49:978-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 101] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 5. | Kadam PD, Chuan HH. Erratum to: Rectocutaneous fistula with transmigration of the suture: a rare delayed complication of vault fixation with the sacrospinous ligament. Int Urogynecol J. 2016;27:505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Folliguet TA, Laborde F, Zannis K, Ghorayeb G, Haverich A, Shrestha M. Sutureless perceval aortic valve replacement: results of two European centers. Ann Thorac Surg. 2012;93:1483-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 173] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 7. | Santarpino G, Pfeiffer S, Concistrè G, Fischlein T. A supra-annular malposition of the Perceval S sutureless aortic valve: the ‘χ-movement’ removal technique and subsequent reimplantation. Interact Cardiovasc Thorac Surg. 2012;15:280-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Vola M, Fuzellier JF, Gerbay A, Campisi S. First in Human Totally Endoscopic Perceval Valve Implantation. Ann Thorac Surg. 2016;102:e299-e301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |