Published online Nov 26, 2018. doi: 10.4330/wjc.v10.i11.201
Peer-review started: July 30, 2018
First decision: August 20, 2018
Revised: September 21, 2018
Accepted: October 7, 2018
Article in press: October 7, 2018
Published online: November 26, 2018
Processing time: 119 Days and 12.2 Hours
Coronary spasm is caused by a transient coronary narrowing due to the constriction of epicardial coronary artery, which leads to myocardial ischemia. More than 50 years have passed since the first recognition of coronary spasm, and many findings on coronary spasm have been reported. Coronary spasm has been considered as having pivotal roles in the cause of not only rest angina but also exertional angina, acute coronary syndrome, and heart failure. In addition, several new findings of the mechanism of coronary spasm have emerged recently. The diagnosis based mainly on coronary angiography and spasm provocation test and the mainstream treatment with a focus on a calcium-channel blocker have been established. At a glance, coronary spasm or vasospastic angina (VSA) has become a common disease. On the contrary, there are several uncertain or unsolved problems regarding coronary spasm, including the presence of medically refractory coronary spasm (intractable VSA), or an appropriate use of implantable cardioverter defibrillator in patients with cardiac arrest who have been confirmed as having coronary spasm. This editorial focused on coronary spasm, including recent topics and unsolved problems.
Core tip: Coronary spasm is the transient vasoconstriction of epicardial coronary artery, leading to myocardial ischemia. Recently, coronary spasm has become widely accepted as one of the important pathophysiologies of coronary artery disease. However, even at present, there are several unsolved problems regarding coronary spasm.
- Citation: Teragawa H, Oshita C, Ueda T. Coronary spasm: It’s common, but it’s still unsolved. World J Cardiol 2018; 10(11): 201-209
- URL: https://www.wjgnet.com/1949-8462/full/v10/i11/201.htm
- DOI: https://dx.doi.org/10.4330/wjc.v10.i11.201
More than several decades have passed since the first recognition of coronary spasm[1-3]. Since then, numerous studies have been conducted, and many findings regarding coronary spasm have been clarified. Coronary spasm is caused by transient narrowing due to the vasoconstriction of the epicardial coronary arteries, leading to myocardial ischemia, and it plays pivotal roles in the cause of not only rest angina but also exertional angina, acute coronary syndrome, including unstable angina, acute myocardial infarction, and ischemic sudden death[4-9]. Recently, coronary spasm has been considered one of the causes of heart failure with reduced ejection fraction[10-12]. Mechanisms responsible for coronary spasm were reported to be the abnormal response of the autonomic nervous system[13], endothelial dysfunction[14-17], abnormal or hyper-reaction of vascular smooth muscles[18-20], and other factors, such as magnesium deficiency[21,22], inheritance[23], or specific anatomy of the coronary artery[24-27]. In addition, the diagnosis and treatment of coronary spasm were based on the guidelines of coronary spasm[28,29]. Its diagnosis has been based on several examinations on the presence of coronary spasm; however, coronary angiography and spasm provocation test (SPT) have been recognized as the standard and final tests[28,30]. It is mainly treated with coronary vasodilators particularly with calcium-channel blocker (CCB)[28,31]. According to the accumulations of experiences, numerous studies, and recent guidelines[6,7,28,29], recently, many physicians roughly know “coronary spasm” or “vasospastic angina” (VSA). However, even at present, there have been undoubtedly several uncertain or unsolved problems on coronary spasm, such as management of medically refractory coronary spasm (intractable VSA) and coronary microvascular angina or appropriate use of implantable cardioverter defibrillator (ICD) for patients with cardiac arrest, who were confirmed as having coronary spasm[28,32,33]. Therefore, this paper focuses on the mechanisms, diagnosis, and treatment of coronary spasm, including recent topics and uncertain or unsolved problems.
Several mechanisms have reported the causes of coronary spasm, such as the abnormal response of the autonomic nervous system[13], endothelial dysfunction of the coronary artery or systemic peripheral vasculature[14-17], abnormal or hyper-reaction of vascular smooth muscles[18-20], and other factors such as a magnesium deficiency[21,22], inheritance[23], or specific anatomy of the coronary artery[24-27]. Naturally, the mechanism of coronary spasm may not be always simple, but may be also multi-factorial. We have come to strongly recognize the multi-factorial mechanisms responsible for coronary spasm when we consider sex differences in the clinical characteristics of VSA patients. Smoking, presence of atherosclerosis of the coronary artery, and morphology of coronary spasm during the SPT differ in male and female VSA patients[8,34,35], indicating the presence of multi-factorial mechanisms of coronary spasm. Findings that the presence of family history of coronary artery disease is higher in women than in men or that younger female VSA patients had higher incidence of smoking than older female VSA patients did, despite the lower incidence of smoking among the whole of female VSA patients[8], are of great interest, taking into consideration the mechanisms of coronary spasm in female patients (Table 1).
| Previously reported or established | Recent topics | Unsolved problems | |
| Mechanism | Abnormal autonomic nervous system Endothelial dysfunction Hyperreactivity of the coronary smooth muscle | Inflammation of perivascular components | |
| Others Inheritance Magnesium deficiency | Specific anatomy of the coronary artery (myocardial bridge) | Different mechanisms in men and women Is there a racial difference in coronary spasm? | |
| Diagnosis | Non-invasive: Holter ECG | Malondialdehyde-modified low-density lipoprotein Exercise ECG | Is a biochemical marker for coronary spasm present? |
| Invasive: SPT | Higher doses of ACh infusions Sequential SPT SPT using a pressure wire Second SPT despite of negative results of first SPT | Detailed SPT protocol using EM Are higher doses of ACh for SPT being used? Does SPT positivity continue for decades? | |
| Treatment | Life style Stop smoking Pharmacological Calcium-channel blockers Sublingual nitroglycerin during attacks Combination of coronary vasodilators | Cilostazol Statin Aspirin | Treatment of intractable VSA Which combinations of coronary vasodilator are the most effective? |
| Non-pharmacological | Use of ICD in VSA patients with cardiac arrest Cardiac rehabilitation | Which is effective in preventing adverse events in VSA patients with cardiac arrest: use of ICD or aggressive medical therapy? Treatment of accompanying microvascular angina |
Among the mechanisms of coronary spasm shown above, Ohyama et al[20,36] have recently reported the relationship between coronary spasm and perivascular components, such as perivascular adipose tissue and adventitial vasa vasorum (Table 1). They showed that such perivascular components play an important role as a source of various inflammatory mediators and showed that inflammatory changes of such perivascular components caused increased the formation of adventitial vasa vasorum and increased the activity of Rho-kinase, leading to the occurrence of coronary spasm[20,36]. These findings appeared to be novel and noteworthy. These findings may account for the presence of focal spasm, because it appears quite difficult to consider the presence of focal spasm based solely on endothelial dysfunction of the coronary artery. On the contrary, the studied VSA patients had coronary spasm of the left anterior descending coronary artery (LAD)[20,36]. Moreover, coronary spasm occurs more frequently in the LAD and right coronary artery (RCA) than in the left circumflex coronary artery (LCX)[37], and it remains unclear whether the findings reported by Ohyama et al[20,36] may also account for coronary spasm in the RCA or differences in the frequency of coronary spasm according to the territory of coronary arteries.
Recently, some interest has also focused on the specific coronary anatomy in VSA patients (Table 1): The presence of myocardial bridge (MB), which is characterized by the systolic narrowing of the epicardial coronary artery because of myocardial compression during systole[24-27]. Furthermore, coronary spasm occurs more frequently at the MB, which is in part mediated by coronary vascular dysfunction, including endothelium-dependent and endothelium-independent dysfunctions, at the MB segments. Further observation regarding the occurrence of coronary spasm at MB segments is needed in the international registry of VSA.
Previously, the prevalence of coronary spasm had been considered higher in Asians than in Caucasians[38,39], showing the presence of racial difference in the occurrence of VSA. However, recently, the presence of VSA is more frequent in Caucasians when SPT is aggressively performed[40,41]. In addition, coronary spasm is considered as playing some roles in the cause of acute coronary syndrome with plaque rupture[42] or myocardial infarction with non-obstructive coronary artery[43]. The aggressive effort of making a diagnosis of VSA may clarify the real presence of VSA worldwide (Table 1).
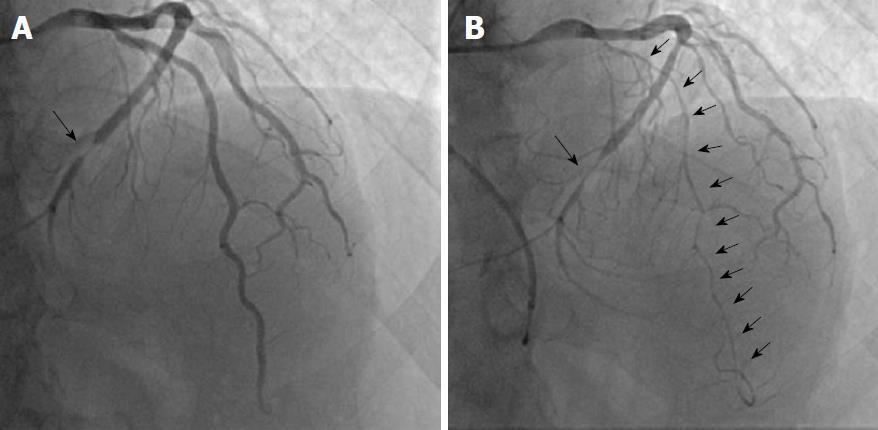
According to the guideline on coronary spasm[28,29], the recognition of transient changes in ST-T segments on electrocardiogram (ECG) during chest symptoms, as well as the presence of chest symptoms derived from coronary spasm, including the good responses to sublingual nitroglycerin and timing of occurrence of coronary spasm at rest, during sleep, or early in the morning, is very important in the diagnosis of VSA. Thus, needless to say, Holter ECG monitoring is important in the diagnosis of VSA[28]; however, Sueda et al[44] reported that approximately half of VSA patients had pathologic exercise tests, showing the importance of exercise ECG testing in the clinical setting. Exercise ECG testing may be also useful in patients suspected of coronary spasm (Table 1). As a biochemical index, which has been eagerly longed for but has not been detected until now (Table 1), the level of malondialdehyde-modified low-density lipoprotein (MDA-LDL) was increased in VSA patients[45]. However, this biochemical marker is reported elevated in patients with other unstable coronary diseases[46,47]. An elevated MDA-LDL level may be carefully interpreted in the diagnosis of VSA. In general, using coronary computed tomography (CT) angiography alone, the diagnosis of VSA itself cannot be obtained, and we doubt the presence of VSA when no significant coronary stenosis is detected on coronary CT angiography. We have sometimes experienced patients with coexistence of coronary spasm and organic coronary stenosis (Figure 1), and the assessment of or exclusion for organic coronary stenosis using a coronary CT angiography may be also needed even in patients, whose diagnosis of VSA was made based on the typical chest symptoms and transient ST-T changes in ECG. Furthermore, as shown above, coronary spasm sometimes occurs at the MB segments[24-27], and the presence of MB on a coronary CT angiography[48] may be a useful clue of the possibility of VSA in patients with chest pain when atherosclerosis was absent on a coronary CT angiography. According to Ohyama et al[20], positron-emission tomography, which has been adopted in the assessment of inflammatory perivascular components, cannot be performed widely in the clinical setting.
Thus, SPT is considered the gold standard examination and actually has been performed frequently because transient ST-T changes on ECG during chest symptoms cannot always be obtained in the clinical setting. Furthermore, SPT may be useful not only in the diagnosis of VSA but also in providing some information in the activity of coronary spasm and prognosis; presence of organic stenosis, multi-vessel spasm, focal spasm, coronary spasm induced by a low dose of acetylcholine (ACh), and total occlusion due to coronary spasm[49-51]. The provocative drugs in SPT are ACh and ergonovine maleate (EM). The methodology of SPT using ACh infusions has been almost established[28-30,52,53], except for the use of transient pacing catheter or the maximal doses of ACh. In general, during SPT using ACh infusions, an insertion of transient pacing catheter via an internal jugular vein or a medial cubital vein may be safer to avoid ACh-induced bradycardia despite the duration of ACh infusion into the coronary artery[54]. The recommended maximal doses of ACh is 100 μg for the left coronary artery (LCA) and 50 μg for the RCA[28]; however, such maximal doses of ACh were determined based on the doses of ACh adopted for the provocation of coronary spasm in patients with variant angina[55], which involved increased coronary spasm activity[49,56]. Thus, the higher maximal doses of ACh in patients with stable VSA are reasonable. Recently, some adopt the maximal doses of ACh as 200 μg for the LCA and 80 μg for the RCA, showing the higher induction of coronary spasm without a significant increase in complications[40,57]. However, it remains unclear whether the higher doses of ACh than the above-mentioned doses are useful or harmful in the SPT (Table 1). On the contrary, the methodology of SPT using EM infusion has not been established sufficiently, compared with that of using ACh (Table 1). The total doses of EM, which are described as the doses of EM with 20-60 μg for 2-5 min for each coronary artery in the guideline[28], vary. In addition, the method of EM infusion, which was infused continuously or with a stepwise incremental dose, has still not been determined. In general, the insertion of transient pacing catheter is unnecessary, and this appears to be advantageous.
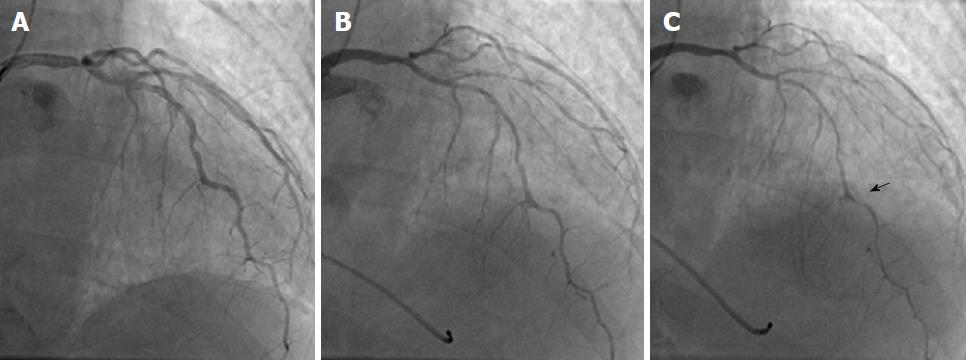
Moreover, the experienced method of SPT using ACh or EM at each institution may be performed safely; however, several tips regarding SPT using these provocative drugs have been known. Female VSA patients have more sensitivity to ACh provocation[8,34,35], and the SPT using ACh infusion may be recommended in female patients who undergo SPT. In addition, some patients have positive SPT using EM infusions despite the negative results in SPT using ACh infusions[30]. Furthermore, Sueda et al[58] have reported the sequential SPT, which was induced by infusions of first ACh, then EM, and finally ACh, showing the high provocative rate without a significant increase in complications[53]. Naturally, the ACh or EM working receptors are different[59], and the use of different provocative drugs for a short duration is reasonable. The sequential SPT may stimulate both receptors simultaneously, leading to a higher provocation of coronary spasm. To our knowledge, the sequential SPT may be the strongest until now. Sueda et al[53,58] showed no difference in complications including major ones or atrial fibrillation between the sequential and standard SPTs. On the contrary, further verification on the presence of false-positive cases will be needed using the sequential SPT. Furthermore, younger patients have a tendency of negative induction of coronary spasm in response to standard provocation[60] due to the not-severe coronary vascular dysfunction, and the sequential SPT may be useful in such patients. In addition, we have experienced some patients who showed no significant coronary stenosis on coronary angiography despite the fact that significant coronary stenosis was suspicious based on the results of examinations and patients’ symptoms. In such cases, the diagnosis of VSA was possible; however, performing an SPT was difficult because an intracoronary nitroglycerin infusion had been administered or taking vasodilators before coronary angiography were continued. Under such circumstances, the sequential SPT may also be useful (Figure 2).
According to the length of coronary spasm induced by the SPT, there have been a subclassification with “focal spasm”, which is defined as vasoconstriction within the confines of one isolated coronary segment, and “diffuse spasm”, which is defined as the vasoconstriction of ≥ 2 adjacent coronary segments[29,50]. Sato et al[50] have shown poorer prognosis in focal spasm than in diffuse spasm. On the contrary, Sueda et al[61] have shown the importance of diffuse spasm as one of causes of medically refractory VSA. Thus, it may be an unsolved problem which “focal spasm” or “diffuse spasm” is worse in the clinical setting[50,61] (Table 1).
The positive criteria of SPT is defined as “transient, total, or sub-total occlusion (> 90% stenosis) of a coronary artery with signs/symptoms of myocardial ischemia (anginal pain and ischemic ST changes)”[28]. However, some patients have significant narrowing induced by provocative drugs despite the chest symptoms and ST-T changes on ECG. Sueda et al[37] showed that such patients were detected in 6.8% of studied patients who underwent an SPT. In addition, we have also experienced some patients with moderate vasoconstriction diffused with chest symptoms and/or ECG changes. Under such circumstances, the diagnosis of VSA may be difficult. At that time, other supportive index for the diagnosis of VSA may be needed. We have shown that the use of pressure wire may help in the diagnosis of VSA[62-64], showing the sudden drop of intracoronary pressure in response to ACh infusions in SPT-positive vessels and less frequency of major complications related to SPT. The validity of SPT using a pressure wire should be verified (Table 1); however, this method may be useful in the following situations: (1) when hemodynamic instability may be precipitated by coronary spasm, such as when patients have hypertrophic cardiomyopathy or left ventricular dysfunction; (2) when patients have chronic kidney disease; and (3) when cardiologists seek to clarify the disease status through a second SPT. SPT has been considered the final examination; however, the results of SPT is not absolute, and we have to make a diagnosis of VSA comprehensively, taking other conditions as well as the results of SPT into consideration. The second session of SPT may be needed in patients who had repeated chest symptoms despite the negative results of the first SPT[64].
Needless to say, smoking cessation is an important treatment of VSA[28]. As a pharmacological treatment for VSA, CCB as prevention and sublingual nitroglycerin during anginal attacks are the first-line therapies for VSA[28,29,31,65]. The monotherapy of β-blockers is class III in VSA patients with organic stenosis[28]. However, VSA is accompanied with many cardiovascular diseases, in which β blockers are effective, such as left ventricular dysfunction[10-12], hypertrophic cardiomyopathy[66], and myocardial bridging[24,26,27,62,67]. Under such conditions, coronary vasodilators should be administered first, and then β blockers should be administered from small doses, observing carefully for the worsening of chest symptoms and hemodynamics.
In addition, the sudden cessation of coronary vasodilators while chest symptoms disappeared under long-term intake of coronary vasodilators may cause severe conditions due to coronary spasm[68]. Avoidance of sudden cessation of coronary vasodilators should be repeated to VSA patients, although the duration of continued coronary spasm activity has not been clarified (Table 1).
Some patients have angina attacks even while under CCB medications. In such conditions, several countermeasures should be followed. First, we must consider the type of CCB, because CCBs may differ in their ability to prevent angina attacks[31,65]. Second, the dosing regimen should be considered, such as whether a submaximal or maximal dose or medication once or twice a day would be appropriate. There are patients on a once-a-day CCB regimen who have had angina attacks just before the dosage time. Third, dosage-timing should be considered. In general, angina attacks often occur between midnight and early morning[5-7,28]. Thus, taking CCB at bedtime is usually recommended. However, for some VSA patients, taking CCB at the time of rising may be effective. Fourth, we must check whether the vasodilators prescribed are branded vasodilators. In VSA patients with high coronary spasm activities, switching from branded vasodilators to generic ones may worsen their chest symptoms[69]. Finally, another vasodilator must be added such as long-acting nitrates, nicorandil, and other type of CCBs (dihydropyridine CCB vs non-dihydropyridine CCB). The combination of more than one and two kinds of coronary vasodilators varies and dependent mainly on each primary doctors’ experience. However, which combination of coronary vasodilators was more useful in preventing coronary spasm is still unclear[70] (Table 1).
Recently, in a randomized, multicenter, double-blind, placebo-controlled study, Shin et al[71] have shown that an addition of cilostazol, which was a selective inhibitor of phosphodiesterase 3, to a CCB decreased the frequency and severity of chest symptoms in VSA patients. Moreover, they showed that an additional of cilostazol may be promising, although the finding that the CCB adopted in the present study was amlodipine, which was not the standard CCB for the prevention of coronary spasm in VSA patients, was a slightly controversial. The usefulness of other drugs such as statins[72,73] and a low-dose aspirin[74,75] on clinical outcomes has been accumulated, and these drugs may be considered to improve the clinical outcomes in VSA patients (Table 1).
First, one of the unsolved problems related to coronary spasm is the presence of intractable VSA, which was defined as angina that cannot be controlled even with the administration of two types of coronary vasodilators. A study revealed that 13.7% of VSA patients had intractable VSA with a younger age at the time of onset and included higher proportions of tobacco smokers and normotensive patients[28]. Our previous report has shown that the presence of SPT-related angiographic findings, such as provocation induced by a low-dose ACh, total occlusion due to coronary spasm, and multi-vessel coronary spasm, were predictors for the presence of intractable VSA[51], showing the importance of performing SPT. When we have controlled the condition of taking several kinds of coronary vasodilators, as shown above, there have been many patients who were refractory to the administrations of several kinds of coronary vasodilators. Among the VSA patients, there have been some VSA patients with microvascular dysfunction[76,77]. Standard coronary vasodilators are less effective in patients with microvascular dysfunction or microvascular angina[33]. Therefore, the comorbid of VSA and microvascular dysfunction may contribute to the presence of intractable VSA. Thus, additional novel drugs may be anticipated. Cardiac rehabilitation has been reportedly effective in preventing coronary spasm in VSA patients[78], and non-pharmacological treatment may be also anticipated.
Second, the need for ICD in VSA patients with cardiac arrest has been one of the unsolved problems of coronary spasm[28,32,56,79,80]. Recently, Sueda et al[32] have summarized the results that appropriate ICD shocks were observed in 24.1% of VSA patients with aborted ICD. Rodríguez-Mañero et al[80] have shown that ICD was effective when insufficient medications were administered in VSA patients. In the clinical setting, whether sufficient medications without ICD can prevent such malignant arrhythmia due to coronary spasm is still undetermined. The physicians-in-chief of the heart team should carefully determine the ICD by taking patient background such as taking coronary vasodilators sufficiently and the results of SPT under sufficient medications[81] into consideration (Table 1).
Given the accumulation of studies on coronary spasm for more than half a century, coronary spasm is the key player and main cause in the pathophysiology of heart diseases. At present, its mechanisms, diagnosis, and treatments have been understood. Nonetheless, some unsolved problems on coronary spasm are still present, and we have to make efforts in obtaining clues to these unsolved problems.
Manuscript source: Invited Manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anan R, De Rosa S, Liberale L, Rostagno C, Ueda H S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | Spritzler R, Corday E, Bergman HC, Prinzmetal M. Studies on the coronary circulation. VIII. Demonstration of spasm of the major coronary arteries. Cardiologia. 1952;21:255-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Prinzmetal M, Ekmekci A, Toyoshima H, Kwoczynski JK. Angina pectoris. III. Demonstration of a chemical origin of ST deviation in classic angina pectoris, its variant form, early myocardial infarction, and some noncardiac conditions. Am J Cardiol. 1959;3:276-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med. 1959;27:375-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1104] [Cited by in RCA: 1002] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 4. | Yasue H, Nagao M, Omote S, Takizawa A, Miwa K, Tanaka S. Coronary arterial spasm and Prinzmetal’s variant form of angina induced by hyperventilation and Tris-buffer infusion. Circulation. 1978;58:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 199] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Yasue H, Omote S, Takizawa A, Nagao M. Coronary arterial spasm in ischemic heart disease and its pathogenesis. A review. Circ Res. 1983;52:I147-I152. [PubMed] |
| 6. | Yasue H, Kugiyama K. Coronary spasm: clinical features and pathogenesis. Intern Med. 1997;36:760-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 165] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51:2-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 378] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 8. | Kawana A, Takahashi J, Takagi Y, Yasuda S, Sakata Y, Tsunoda R, Ogata Y, Seki A, Sumiyoshi T, Matsui M. Gender differences in the clinical characteristics and outcomes of patients with vasospastic angina--a report from the Japanese Coronary Spasm Association. Circ J. 2013;77:1267-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Shin ES, Ann SH, Singh GB, Lim KH, Yoon HJ, Hur SH, Her AY, Koo BK, Akasaka T. OCT-Defined morphological characteristics of coronary artery spasm sites in vasospastic angina. JACC Cardiovasc Imaging. 2015;8:1059-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 10. | Sueda S, Kohno H, Oshita A, Izoe Y, Nomoto T, Fukuda H. Vasospastic heart failure: multiple spasm may cause transient heart failure? J Cardiol. 2009;54:452-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Inami T, Kataoka M, Shimura N, Ishiguro H, Kohshoh H, Taguchi H, Yanagisawa R, Hara Y, Satoh T, Yoshino H. Left ventricular dysfunction due to diffuse multiple vessel coronary artery spasm can be concealed in dilated cardiomyopathy. Eur J Heart Fail. 2012;14:1130-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Oda S, Fujii Y, Takemoto H, Nomura S, Nakayama H, Toyota Y, Nakamura H, Teragawa H. Heart failure in which coronary spasms played an important role. Intern Med. 2014;53:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Yasue H, Touyama M, Shimamoto M, Kato H, Tanaka S. Role of autonomic nervous system in the pathogenesis of Prinzmetal’s variant form of angina. Circulation. 1974;50:534-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 316] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Okumura K, Yasue H, Ishizaka H, Ogawa H, Fujii H, Yoshimura M. Endothelium-dependent dilator response to substance P in patients with coronary spastic angina. J Am Coll Cardiol. 1992;20:838-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Kugiyama K, Ohgushi M, Motoyama T, Sugiyama S, Ogawa H, Yoshimura M, Inobe Y, Hirashima O, Kawano H, Soejima H. Nitric oxide-mediated flow-dependent dilation is impaired in coronary arteries in patients with coronary spastic angina. J Am Coll Cardiol. 1997;30:920-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Teragawa H, Kato M, Kurokawa J, Yamagata T, Matsuura H, Chayama K. Endothelial dysfunction is an independent factor responsible for vasospastic angina. Clin Sci (Lond). 2001;101:707-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Teragawa H, Mitsuba N, Ishibashi K, Nishioka K, Kurisu S, Kihara Y. Evaluation of coronary microvascular function in patients with vasospastic angina. World J Cardiol. 2013;5:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Shimokawa H. Cellular and molecular mechanisms of coronary artery spasm: lessons from animal models. Jpn Circ J. 2000;64:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 125] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Shimokawa H. 2014 Williams Harvey Lecture: importance of coronary vasomotion abnormalities-from bench to bedside. Eur Heart J. 2014;35:3180-3193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 172] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 20. | Ohyama K, Matsumoto Y, Takanami K, Ota H, Nishimiya K, Sugisawa J, Tsuchiya S, Amamizu H, Uzuka H, Suda A. Coronary adventitial and perivascular adipose tissue inflammation in patients with vasospastic angina. J Am Coll Cardiol. 2018;71:414-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 135] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 21. | Satake K, Lee JD, Shimizu H, Ueda T, Nakamura T. Relation between severity of magnesium deficiency and frequency of anginal attacks in men with variant angina. J Am Coll Cardiol. 1996;28:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Teragawa H, Kato M, Yamagata T, Matsuura H, Kajiyama G. The preventive effect of magnesium on coronary spasm in patients with vasospastic angina. Chest. 2000;118:1690-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Yoshimura M, Yasue H, Nakayama M, Shimasaki Y, Ogawa H, Kugiyama K, Saito Y, Miyamoto Y, Ogawa Y, Kaneshige T. Genetic risk factors for coronary artery spasm: significance of endothelial nitric oxide synthase gene T-786-->C and missense Glu298Asp variants. J Investig Med. 2000;48:367-374. [PubMed] |
| 24. | Teragawa H, Fukuda Y, Matsuda K, Hirao H, Higashi Y, Yamagata T, Oshima T, Matsuura H, Chayama K. Myocardial bridging increases the risk of coronary spasm. Clin Cardiol. 2003;26:377-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Kim JW, Seo HS, Na JO, Suh SY, Choi CU, Kim EJ, Rha SW, Park CG, Oh DJ. Myocardial bridging is related to endothelial dysfunction but not to plaque as assessed by intracoronary ultrasound. Heart. 2008;94:765-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Saito Y, Kitahara H, Shoji T, Tokimasa S, Nakayama T, Sugimoto K, Fujimoto Y, Kobayashi Y. Relation between severity of myocardial bridge and vasospasm. Int J Cardiol. 2017;248:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 27. | Nam P, Choi BG, Choi SY, Byun JK, Mashaly A, Park Y, Jang WY, Kim W, Choi JY, Park EJ. The impact of myocardial bridge on coronary artery spasm and long-term clinical outcomes in patients without significant atherosclerotic stenosis. Atherosclerosis. 2018;270:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 28. | JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circ J. 2014;78:2779-2801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 356] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 29. | Beltrame JF, Crea F, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Bairey Merz CN; Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017;38:2565-2568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 179] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 30. | Sueda S, Kohno H, Ochi T, Uraoka T, Tsunemitsu K. Overview of the pharmacological spasm provocation test: Comparisons between acetylcholine and ergonovine. J Cardiol. 2017;69:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Nishigaki K, Inoue Y, Yamanouchi Y, Fukumoto Y, Yasuda S, Sueda S, Urata H, Shimokawa H, Minatoguchi S. Prognostic effects of calcium channel blockers in patients with vasospastic angina--a meta-analysis. Circ J. 2010;74:1943-1950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | Sueda S, Kohno H. Optimal Medications and Appropriate Implantable Cardioverter-defibrillator Shocks in Aborted Sudden Cardiac Death Due to Coronary Spasm. Intern Med. 2018;57:1361-1369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Ong P, Camici PG, Beltrame JF, Crea F, Shimokawa H, Sechtem U, Kaski JC, Bairey Merz CN; Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. 2018;250:16-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 610] [Cited by in RCA: 539] [Article Influence: 77.0] [Reference Citation Analysis (0)] |
| 34. | Sueda S, Miyoshi T, Sasaki Y, Sakaue T, Habara H, Kohno H. Gender differences in sensitivity of acetylcholine and ergonovine to coronary spasm provocation test. Heart Vessels. 2016;31:322-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Aziz A, Hansen HS, Sechtem U, Prescott E, Ong P. Sex-related differences in vasomotor function in patients with angina and unobstructed coronary arteries. J Am Coll Cardiol. 2017;70:2349-2358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 148] [Article Influence: 18.5] [Reference Citation Analysis (1)] |
| 36. | Ohyama K, Matsumoto Y, Nishimiya K, Hao K, Tsuburaya R, Ota H, Amamizu H, Uzuka H, Takahashi J, Ito K. Increased coronary perivascular adipose tissue volume in patients with vasospastic angina. Circ J. 2016;80:1653-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Sueda S, Miyoshi T, Sasaki Y, Ohshima K, Sakaue T, Habara H, Kohno H. Complete definite positive spasm on acetylcholine spasm provocation tests: comparison of clinical positive spasm. Heart Vessels. 2016;31:143-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 38. | Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol. 1999;33:1442-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 266] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 39. | Pristipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, Mongiardo R, Cianflone D, Sanna T, Sasayama S, Maseri A. Major racial differences in coronary constrictor response between japanese and caucasians with recent myocardial infarction. Circulation. 2000;101:1102-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 264] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 40. | Ong P, Athanasiadis A, Hill S, Vogelsberg H, Voehringer M, Sechtem U. Coronary artery spasm as a frequent cause of acute coronary syndrome: The CASPAR (Coronary Artery Spasm in Patients With Acute Coronary Syndrome) Study. J Am Coll Cardiol. 2008;52:523-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 255] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 41. | Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol. 2012;59:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 288] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 42. | Kanwar SS, Stone GW, Singh M, Virmani R, Olin J, Akasaka T, Narula J. Acute coronary syndromes without coronary plaque rupture. Nat Rev Cardiol. 2016;13:257-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 43. | Scalone G, Niccoli G, Crea F. Pathophysiology, diagnosis and management of MINOCA: an update. Eur Heart J Acute Cardiovasc Care. 2018;2048872618782414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 122] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 44. | Sueda S, Miyoshi T, Sasaki Y, Sakaue T, Habara H, Kohno H. Approximately half of patients with coronary spastic angina had pathologic exercise tests. J Cardiol. 2016;68:13-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 45. | Ito T, Fujita H, Tani T, Sugiura T, Ohte N. Increased circulating malondialdehyde-modified low-density lipoprotein levels in patients with ergonovine-induced coronary artery spasm. Int J Cardiol. 2015;184:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 46. | Tajika K, Okamatsu K, Takano M, Inami S, Yamamoto M, Murakami D, Kobayashi N, Ohba T, Hata N, Seino Y. Malondialdehyde-modified low-density lipoprotein is a useful marker to identify patients with vulnerable plaque. Circ J. 2012;76:2211-2217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 47. | Ikenaga H, Kurisu S, Kono S, Sumimoto Y, Watanabe N, Shimonaga T, Higaki T, Iwasaki T, Mitsuba N, Ishibashi K. Impact of Malondialdehyde-Modified Low-Density Lipoprotein on Tissue Characteristics in Patients With Stable Coronary Artery Disease - Integrated Backscatter-Intravascular Ultrasound Study. Circ J. 2016;80:2173-2182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Yu M, Zhang Y, Li Y, Li M, Li W, Zhang J. Assessment of Myocardial Bridge by Cardiac CT: Intracoronary Transluminal Attenuation Gradient Derived from Diastolic Phase Predicts Systolic Compression. Korean J Radiol. 2017;18:655-663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 49. | Takagi Y, Takahashi J, Yasuda S, Miyata S, Tsunoda R, Ogata Y, Seki A, Sumiyoshi T, Matsui M, Goto T. Prognostic stratification of patients with vasospastic angina: a comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J Am Coll Cardiol. 2013;62:1144-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 139] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 50. | Sato K, Kaikita K, Nakayama N, Horio E, Yoshimura H, Ono T, Ohba K, Tsujita K, Kojima S, Tayama S. Coronary vasomotor response to intracoronary acetylcholine injection, clinical features, and long-term prognosis in 873 consecutive patients with coronary spasm: analysis of a single-center study over 20 years. J Am Heart Assoc. 2013;2:e000227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 119] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 51. | Teragawa H, Fujii Y, Oshita C, Ueda T. Importance of the spasm provocation test in diagnosing and clarifying the activity of vasospastic angina. Interv Cardiol J. 2017;3:58. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Sueda S, Kohno H, Ochi T, Uraoka T. Overview of the Acetylcholine Spasm Provocation Test. Clin Cardiol. 2015;38:430-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 53. | Sueda S, Kohno H. Overview of complications during pharmacological spasm provocation tests. J Cardiol. 2016;68:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 54. | Sueda S, Kohno H. The acetylcholine administration time plays the key role for provoked spasm in the spasm provocation test. J Cardiol. 2017;70:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 55. | Okumura K, Yasue H, Matsuyama K, Goto K, Miyagi H, Ogawa H, Matsuyama K. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am Coll Cardiol. 1988;12:883-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 237] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 56. | Ahn JM, Lee KH, Yoo SY, Cho YR, Suh J, Shin ES, Lee JH, Shin DI, Kim SH, Baek SH. Prognosis of Variant Angina Manifesting as Aborted Sudden Cardiac Death. J Am Coll Cardiol. 2016;68:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 57. | Sueda S, Kohno H, Miyoshi T, Sakaue T, Sasaki Y, Habara H. Maximal acetylcholine dose of 200 μg into the left coronary artery as a spasm provocation test: comparison with 100 μg of acetylcholine. Heart Vessels. 2015;30:771-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 58. | Sueda S, Miyoshi T, Sasaki Y, Sakaue T, Habara H, Kohno H. Sequential spasm provocation tests might overcome a limitation of the standard spasm provocation tests. Coron Artery Dis. 2015;26:490-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 59. | Cosentino F, Lüscher TF. Endothelial function in coronary artery disease. Cardiologia. 1997;42:1221-1227. [PubMed] |
| 60. | Sueda S, Kohno H, Sakaue T, Higaki T. Acetylcholine test is less sensitive to provoke coronary artery spasm in young rest angina patients: limitations of single pharmacological spasm provocation tests. J Jpn Coron Assoc. 2013;19:347-354. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 61. | Sueda S, Kohno H, Fukuda H, Watanabe K, Ochi N, Kawada H, Uraoka T. Limitations of medical therapy in patients with pure coronary spastic angina. Chest. 2003;123:380-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 62. | Teragawa H, Fujii Y, Ueda T, Murata D, Nomura S. Case of angina pectoris at rest and during effort due to coronary spasm and myocardial bridging. World J Cardiol. 2015;7:367-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 63. | Teragawa H, Fujii Y, Uchimura Y, Oshita C, Ueda T, Kihara Y. Usefulness of a pressure wire for the diagnosis of vasospastic angina during a spasm provocation test. J Clin Exp Res Cardiol. 2017;3:203. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 64. | Teragawa H, Fujii Y, Uchimura Y, Ueda T. Importance of a second spasm provocation test: Four cases with an initial negative spasm provocation test. World J Cardiol. 2017;9:289-295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 65. | Oikawa Y, Matsuno S, Yajima J, Nakamura M, Ono T, Ishiwata S, Fujimoto Y, Aizawa T. Effects of treatment with once-daily nifedipine CR and twice-daily benidipine on prevention of symptomatic attacks in patients with coronary spastic angina pectoris-Adalat Trial vs Coniel in Tokyo against Coronary Spastic Angina (ATTACK CSA). J Cardiol. 2010;55:238-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 66. | Sueda S, Kohno H, Fukuda H, Ochi N, Kawada H, Hayashi Y, Uraoka T. Frequency of provoked coronary spasms in patients undergoing coronary arteriography using a spasm provocation test via intracoronary administration of ergonovine. Angiology. 2004;55:403-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 67. | Teragawa H, Fujii Y, Oshita C, Uchimura Y, Ueda T. What factors contribute to chest symptoms during exercise in patients with vasospastic angina? Angiol. 2017;5:202. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 68. | Teragawa H, Nishioka K, Fujii Y, Idei N, Hata T, Kurushima S, Shokawa T, Kihara Y. Worsening of coronary spasm during the perioperative period: A case report. World J Cardiol. 2014;6:685-688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 69. | Goto-Semba R, Fujii Y, Ueda T, Oshita C, Teragawa H. Increased frequency of angina attacks caused by switching a brand-name vasodilator to a generic vasodilator in patients with vasospastic angina: Two case reports. World J Cardiol. 2018;10:15-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 70. | Park T, Park JY, Rha SW, Seo HS, Choi BG, Choi SY, Byun JK, Park SH, Park EJ, Choi JY. Impact of Diltiazem Alone versus Diltiazem with Nitrate on Five-Year Clinical Outcomes in Patients with Significant Coronary Artery Spasm. Yonsei Med J. 2017;58:90-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 71. | Shin ES, Lee JH, Yoo SY, Park Y, Hong YJ, Kim MH, Lee JY, Nam CW, Tahk SJ, Kim JS. A randomised, multicentre, double blind, placebo controlled trial to evaluate the efficacy and safety of cilostazol in patients with vasospastic angina. Heart. 2014;100:1531-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 72. | Yasue H, Mizuno Y, Harada E, Itoh T, Nakagawa H, Nakayama M, Ogawa H, Tayama S, Honda T, Hokimoto S, Ohshima S, Hokamura Y, Kugiyama K, Horie M, Yoshimura M, Harada M, Uemura S, Saito Y; SCAST (Statin and Coronary Artery Spasm Trial) Investigators. Effects of a 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, fluvastatin, on coronary spasm after withdrawal of calcium-channel blockers. J Am Coll Cardiol. 2008;51:1742-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 124] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 73. | Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, Tabata N, Arima Y, Sueta D, Sakamoto K. Impact of statin therapy on clinical outcome in patients with coronary spasm. J Am Heart Assoc. 2016;5:pii: e003426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 74. | Lim AY, Park TK, Cho SW, Oh MS, Lee da H, Seong CS, Gwag HB, Yang JH, Song YB, Hahn JY. Clinical implications of low-dose aspirin on vasospastic angina patients without significant coronary artery stenosis; a propensity score-matched analysis. Int J Cardiol. 2016;221:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 75. | Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, Tabata N, Arima Y, Sueta D, Sakamoto K. Impact of aspirin on the prognosis in patients with coronary spasm without significant atherosclerotic stenosis. Int J Cardiol. 2016;220:328-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 76. | Akasaka T, Yoshida K, Hozumi T, Takagi T, Kawamoto T, Kaji S, Morioka S, Yoshikawa J. Comparison of coronary flow reserve between focal and diffuse vasoconstriction induced by ergonovine in patients with vasospastic angina. Am J Cardiol. 1997;80:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 77. | Sueda S, Kohno H, Fukuda H, Uraoka T. Coronary flow reserve in patients with vasospastic angina: correlation between coronary flow reserve and age or duration of angina. Coron Artery Dis. 2003;14:423-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 78. | Morikawa Y, Mizuno Y, Harada E, Katoh D, Kashiwagi Y, Morita S, Yoshimura M, Uemura S, Saito Y, Yasue H. Aerobic interval exercise training in the afternoon reduces attacks of coronary spastic angina in conjunction with improvement in endothelial function, oxidative stress, and inflammation. Coron Artery Dis. 2013;24:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 79. | Takagi Y, Yasuda S, Tsunoda R, Ogata Y, Seki A, Sumiyoshi T, Matsui M, Goto T, Tanabe Y, Sueda S. Clinical characteristics and long-term prognosis of vasospastic angina patients who survived out-of-hospital cardiac arrest: multicenter registry study of the Japanese Coronary Spasm Association. Circ Arrhythm Electrophysiol. 2011;4:295-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 147] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 80. | Rodríguez-Mañero M, Oloriz T, le Polain de Waroux JB, Burri H, Kreidieh B, de Asmundis C, Arias MA, Arbelo E, Díaz Fernández B, Fernández-Armenta J. Long-term prognosis of patients with life-threatening ventricular arrhythmias induced by coronary artery spasm. Europace. 2018;20:851-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 81. | Sueda S, Kohno H, Miyoshi T, Sasaki Y, Sakaue T, Habara H. Spasm provocation tests performed under medical therapy: a new approach for treating patients with refractory coronary spastic angina on emergency admission. Intern Med. 2014;53:1739-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |