Copyright
©The Author(s) 2017.
World J Cardiol. Aug 26, 2017; 9(8): 710-714
Published online Aug 26, 2017. doi: 10.4330/wjc.v9.i8.710
Published online Aug 26, 2017. doi: 10.4330/wjc.v9.i8.710
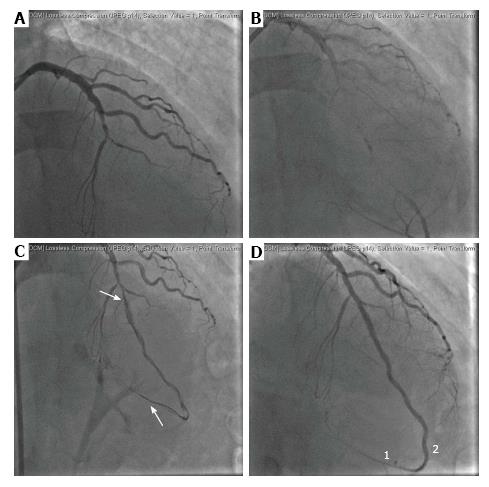
Figure 1 Baseline chronic total occlusion-percutaneous revascularization of the left anterior descending.
A and B: Mid-LAD occlusion with omolateral reperfusion of the distal segment; C: Dissected segment after CTO recanalization and balloon dilation (white arrows); D: Final result after four BVS implantation and (2) contrast staining at the distal LAD suggesting the presence of subintimal hematoma with the occlusion of the distal apical branch (1). BVS: Bioresorbable vascular scaffolds; LAD: Left anterior descending; CTO: Chronic total occlusion.
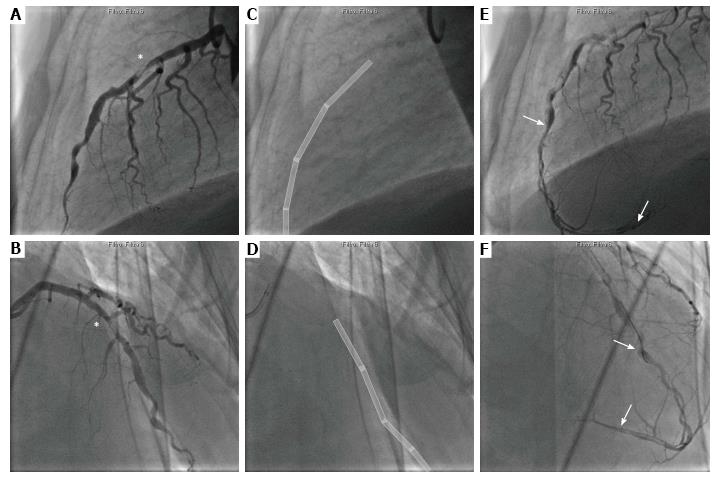
Figure 2 Coronary angiography of the left anterior descending at 28 mo after chronic total occlusion recanalization.
A and B: Large in-scaffold thrombus at the proximal edge of the previously implanted BVS (C, D, white boxes), at the mid LAD (*); E and F: Dissected segment (white arrows) from the mid-LAD up to the distal segment, with a resulting image of a “dual lumen” LAD. LAD: Left anterior descending; BVS: Bioresorbable vascular scaffolds.
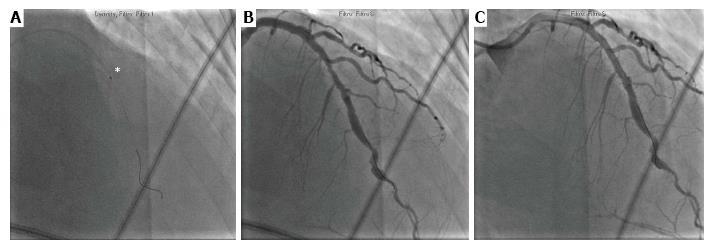
Figure 3 Percutaneous revascularization of the left anterior descending.
A and B: After coronary wire crossing, thrombus aspiration was successfully performed (*) and a drug eluting stent was finally implanted with good final result (C).
- Citation: Di Serafino L, Cirillo P, Niglio T, Borgia F, Trimarco B, Esposito G, Stabile E. Very late bioresorbable scaffold thrombosis and reoccurrence of dissection two years later chronic total occlusion recanalization of the left anterior descending artery. World J Cardiol 2017; 9(8): 710-714
- URL: https://www.wjgnet.com/1949-8462/full/v9/i8/710.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i8.710