Copyright
©The Author(s) 2017.
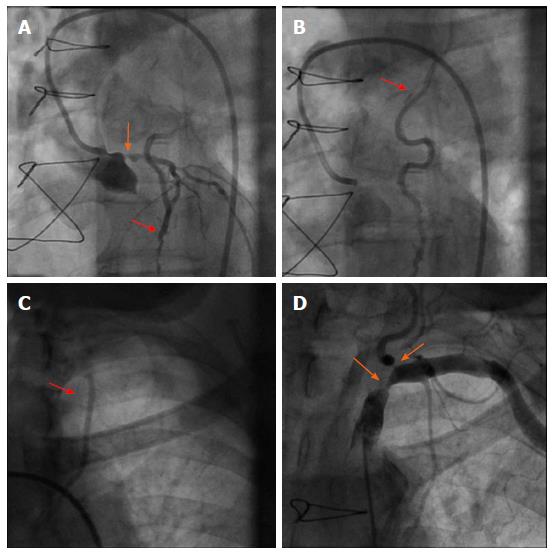
Figure 1 Reverse blood flow was observed from the left artery disease to the left internal mammary artery graft.
During coronary angiography (red arrows in A and B) despite 75% stenosis of the left main coronary artery (orange arrow in A), contrast injection could be followed up to the insertion of the graft in the subclavian artery (red arrow in C). Angiography of the subclavian artery revealed high grade lesions in the subclavian and left vertebral artery (orange arrows in D).
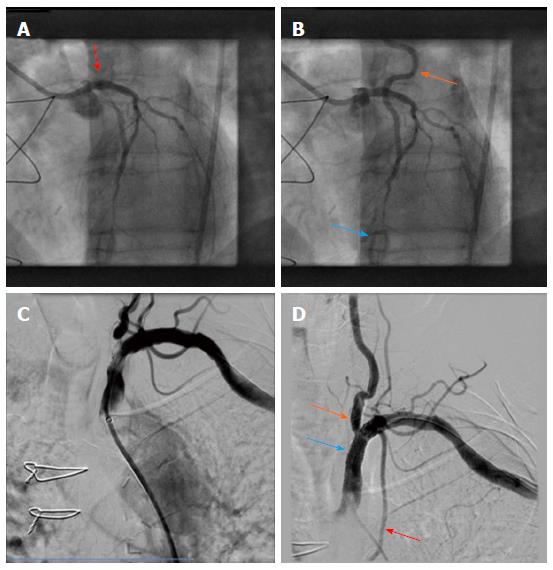
Figure 2 Percutaneous coronary intervention of left main artery and stent placement.
It was performed with a good angiographic result (red arrow in A) However, retrograde flow from the left artery disease LAD to the LIMA graft remained after PCI, and sparse flow was seen in the distal LAD (orange and blue arrows in B, respectively). DSA confirmed the presence of high grades stenosis of the left subclavian and vertrebral artery (C). After angioplasty and bifurcation stent implantation a good angiographic result can be appreciated (orange and blue arrows in D) with normal opacification of the LIMA graft (red arrow in D). PCI: Percutaneous coronary intervention; LAD: Left artery disease; LIMA: Left internal mammary artery; DSA: Digital subtraction angiography.
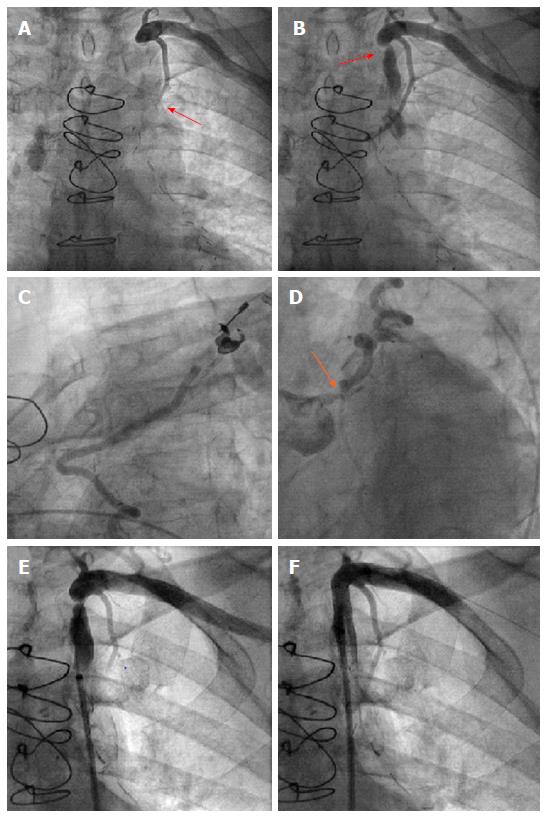
Figure 3 After selective contrast injection into the left internal mammary artery graft no contrast opafication.
It was shown in the left artery disease (red arrow in A). Subsequently, a high grade stenosis of the left subclavian artery was observed (red arrow in B). During coronary angiography retrograde flow from the left artery disease up to the origin of the LIMA graft could be demonstrated (C), despite left main stenosis (orange arrow in D). After angioplasty and stent placement (E) antegrade flow could be re-established in the subclavian artery (F). LIMA: Left internal mammary artery.
- Citation: Heid J, Vogel B, Kristen A, Kloos W, Kohler B, Katus HA, Korosoglou G. Interventional treatment of the left subclavian in 2 patients with coronary steal syndrome. World J Cardiol 2017; 9(1): 65-70
- URL: https://www.wjgnet.com/1949-8462/full/v9/i1/65.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i1.65