Copyright
©The Author(s) 2016.
World J Cardiol. Nov 26, 2016; 8(11): 623-637
Published online Nov 26, 2016. doi: 10.4330/wjc.v8.i11.623
Published online Nov 26, 2016. doi: 10.4330/wjc.v8.i11.623
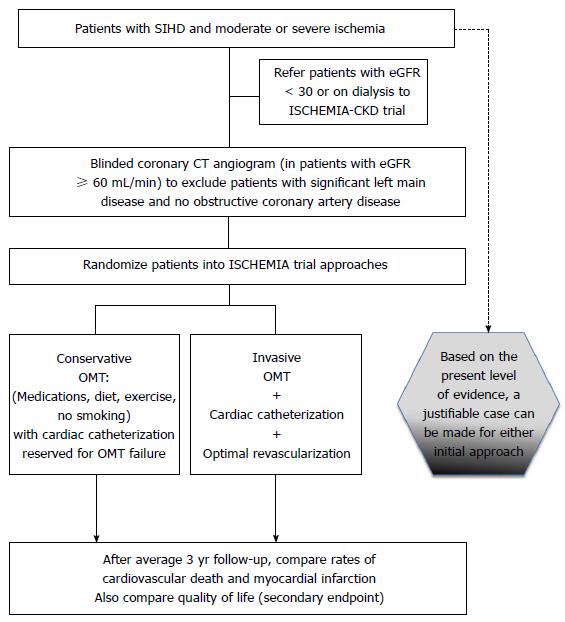
Figure 1 International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (NCT01471522) trial design.
After Stone et al[17]. CCTA may not be performed with estimated glomerular filtration rate < 60 mL/min. Participants in whom CCTA show significant left main disease (≥ 50% stenosis) or no obstructive disease are excluded. CCTA results are otherwise kept blinded. ISCHEMIA: International study of comparative health effectiveness with medical and invasive approaches; CCTA: Coronary computed tomographic angiography; eGFR: Estimated glomerular filtration rate; OMT: Optimal medical therapy = guideline-directed medical therapy; SIHD: Stable ischemic heart disease.
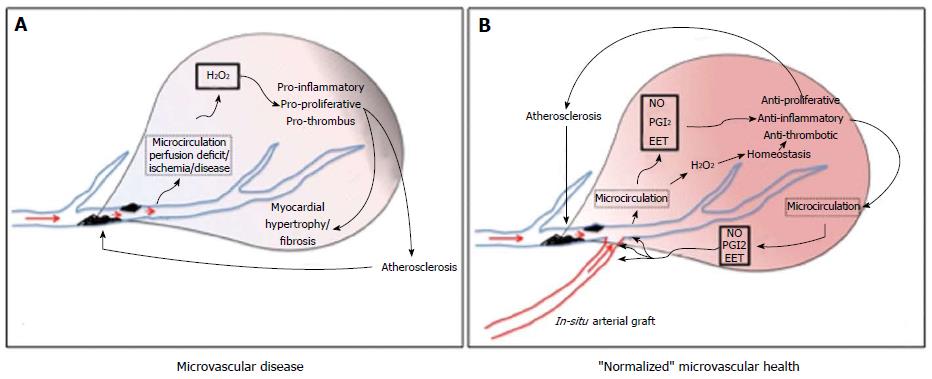
Figure 2 From Ferguson et al[37], with adaptation from Gutterman et al[62].
In a healthy heart, arteriolar endothelium produces NO, prostacyclin (PGI2, and EETs) as well as low levels of hydrogen peroxide, which support a quiescent non proliferative state. With the onset of disease (A), flow through the microvasculature releases hydrogen peroxide, creating a proinflammatory environment throughout the organ, potentially leading to hypertrophy, fibrosis, and atherosclerosis. In B, with bypass grafting of ischemic myocardium, the microvascular health of the myocardium is “normalized”. NO: Nitric oxide; PGI2: Prostacyclin; EET: Epoxyeicosatrienoic acids.
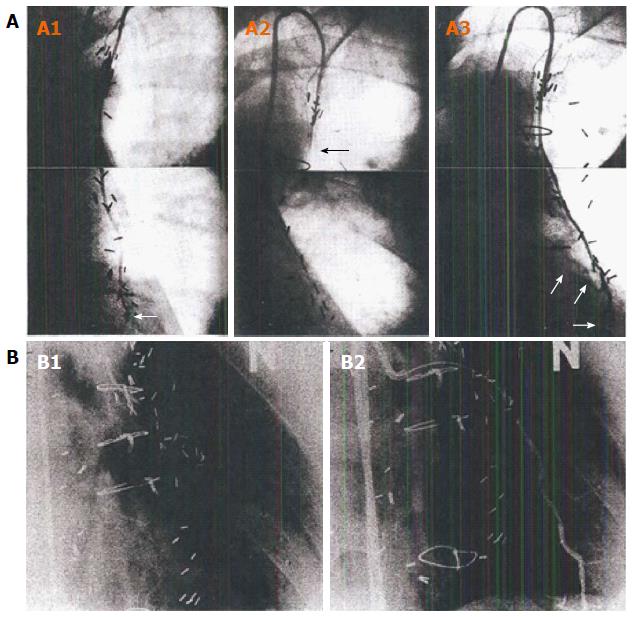
Figure 3 Composite of string sign data.
Angiographic documentation of the development of a “string-sign” IMA graft. A: Data from Dincer et al[98]. A1: Composite still images from angiogram of IMA-LAD graft at 8 d postop. White arrow show anastomotic site; A2: Composite still images from an angiogram at 1-year postop. Black arrow identifies “string-sign” IMA conduit with little if any distal flow; A3: Composite still images from angiogram at 5 years postop, documenting a widely patent IMA-LAD graft. The three white arrows outline the native TVECA LAD proximal and distal to the anastomosis. There is no angiographic evidence of atherosclerotic disease in the IMA, and no anastomotic evidence of narrowing; B: Data from Kitamura et al[99]. Images that clearly illustrate the physiology of arterial conduits. B1: A stringlike LIMA with no-flow into the LAD. Because of the limitations of conventional angiography, flow down the TVECA LAD cannot be simultaneously visualized, but was patent with good antegrade flow; B2: Repeat LIMA arteriography now showing anatomical patency of the graft, as a result of temporary occlusion of the recipient LAD with a percutaneous transluminal coronary angioplasty balloon. The acute influence of anterior wall hypoperfusion immediately translated into resumed functionality of the LIMA graft, documenting the coupling of physiologic IMA flow to the distal regional myocardial physiologic status. IMA: Internal mammary artery; LAD: Left anterior descending coronary artery; TVECA: Target vessel epicardial coronary artery.
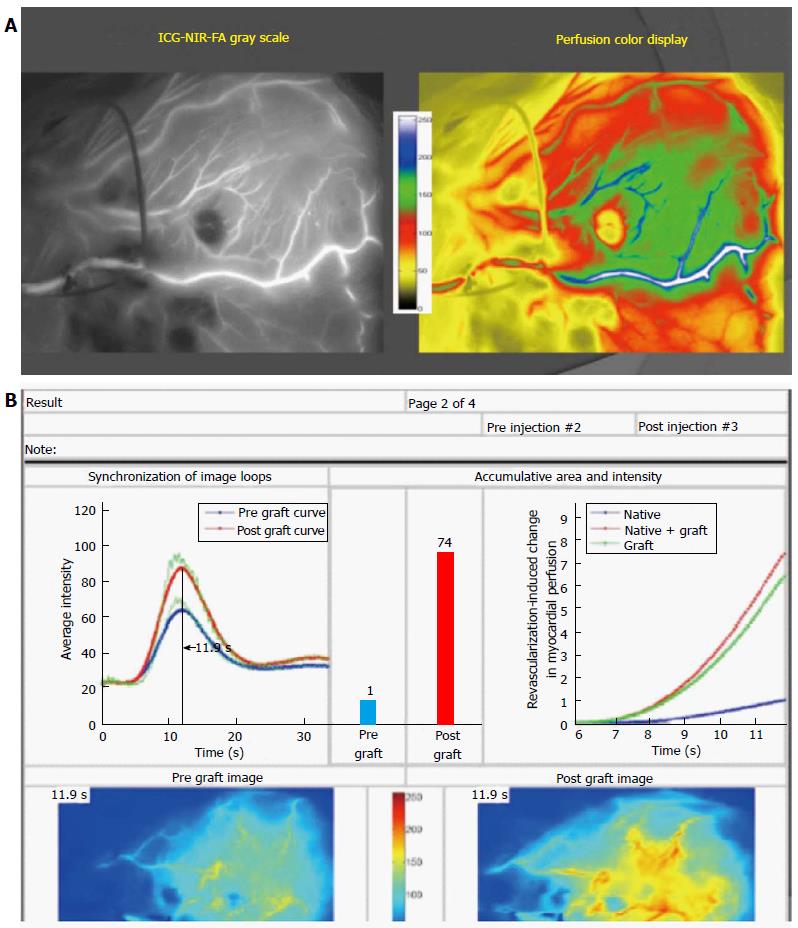
Figure 4 SPY near-infrared imaging of the physiology of revascularization and quantification of the change in regional myocardial perfusion as a result of bypass grafting.
A: Near-infrared frame from 34-s video of IMA graft to LAD in 256 grey scale (left panel) and more intuitive color scale (see color bar) to differentiate perfusion differences to the myocardium. The video shows the dynamic arterial and microvascular blood flow interaction between the native TVECA flow and the IMA graft flow in real-time and under true physiologic conditions; B: The Complex Angiography and Perfusion Analysis platform result from and IMA to LAD graft in a patient with prior anterior MI and regional myocardial ischemia preoperatively. The right upper panel quantitatively compares pre-bypass TVECA regional myocardial perfusion (blue line and bar) with post-bypass combination of TVECA + IMA perfusion (red line and bar). The green line in the graph is the relative contribution to perfusion of the IMA graft flow. The two bottom images are synchronized with respect to timing, as shown by the marker on the upper left graph. This patient with anterior ischemia had a 7-fold increase in perfusion to the anterior regional myocardium as a result of IMA grafting. In addition, the proximal LAD in this patient was 100% occluded, and the pre-grafting TVECA perfusion was entirely from flow through lateral and inferior collaterals. IMA: Internal mammary artery; LAD: Left anterior descending coronary artery; TVECA: Target vessel epicardial coronary artery.
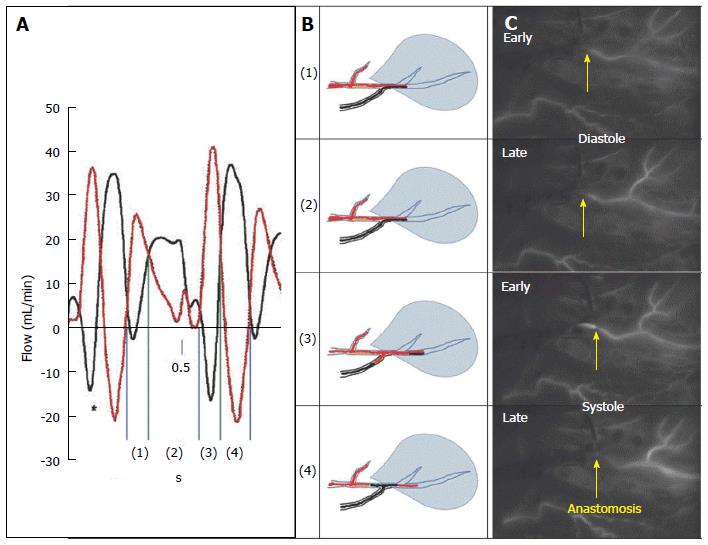
Figure 5 Intraoperative real-time documentation of competitive flow in arterial internal mammary artery-left anterior descending coronary anastomosis with > 70% stenosis.
Competitive flow documented in in situ arterial graft to TVECA with > 70% proximal stenosis. A: Dynamic flow data from Pagni et al[71] illustrating flow in IMA (red) and LAD (black) in an experimental model of competitive flow where the LAD has no proximal stenosis (maximal competitive flow). In phases 1 and 2, during diastole, there is antegrade flow in both the TVECA and the arterial graft. In early systole, there is antegrade flow in the TVECA but retrograde flow in the distal arterial graft, which reverses in late systole, where there is retrograde flow in the TVECA and antegrade flow in the arterial conduit; B: Diagrammatically the IMA-LAD interaction at the anastomosis in this patient; C: Four still frames taken from the 34-s video of this bypass graft using near-infrared imaging technology (SPY, Novadaq Technologies, Toronto, Ontario, CA). The arrow indicates the site of the anastomosis. The four frames are in temporal sequence but not consecutive frames; they are selected at the four diagram points indicated at the middle panel. Each diagram point is taken from the appropriate time-point within each of the four intervals (early diastole, late diastole, early systole, late diastole). This real-time intraoperative imaging shows identical flow patterns as demonstrated in the Pagni experimental model, despite the proximal > 70% stenosis. IMA: Internal mammary artery; LAD: Left anterior descending coronary artery; TVECA: Target vessel epicardial coronary artery.
- Citation: Ferguson Jr TB. Physiology of in-situ arterial revascularization in coronary artery bypass grafting: Preoperative, intraoperative and postoperative factors and influences. World J Cardiol 2016; 8(11): 623-637
- URL: https://www.wjgnet.com/1949-8462/full/v8/i11/623.htm
- DOI: https://dx.doi.org/10.4330/wjc.v8.i11.623