Copyright
©The Author(s) 2015.
World J Cardiol. Feb 26, 2015; 7(2): 86-100
Published online Feb 26, 2015. doi: 10.4330/wjc.v7.i2.86
Published online Feb 26, 2015. doi: 10.4330/wjc.v7.i2.86
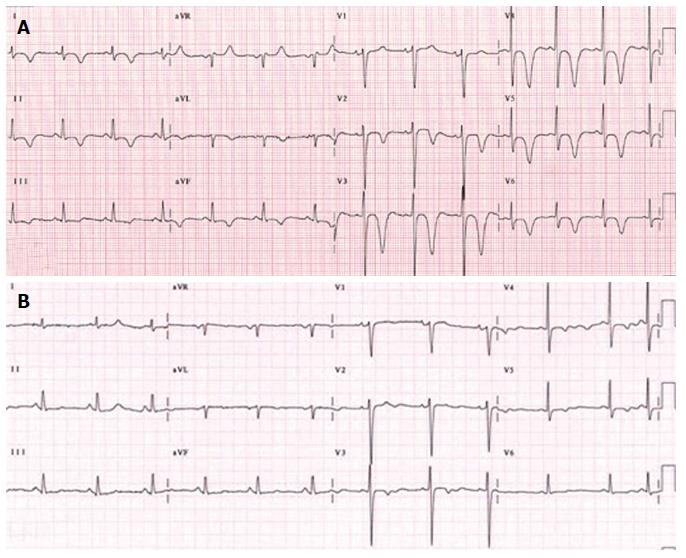
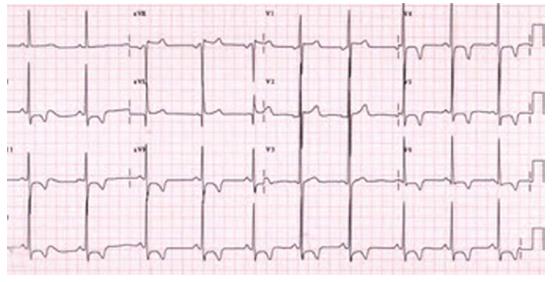
Figure 1 Patient 1.
A: An electrocardiographic (ECG) tracing, illustrating the negative T-wave in the precordial leads V2-6, of a 51-year-old-female patient presented with palpitation following electroconvulsive therapy for her depression. In 2001, she underwent catheter ablation for atrioventricular nodal reentry tachycardia. She complained of palpitation after a shock of electroconvulsive therapy for treatment of depression. Post-electroconvulsive therapy, the ECG showed giant T-wave inversion in the precordial leads. The cardiac enzymes were minimally raised. Takotsubo cardiomyopathy is suggested due to emotional stress and electrical shock. Transthoracic echocardiography demonstrated apical hypokinesia and basal normokinesia with trivial valvular regurgitation without massive pericardial effusion. The estimated right ventricular systolic pressure was 35 mmHg. Coronary angiography and cardiac magnetic resonance imaging demonstrated normal findings. Medical treatment with beta blocker was initiated and the symptoms disappeared and (B) the ECG returned to base line in 2 wk time. The antidepressant drug was not discontinued.
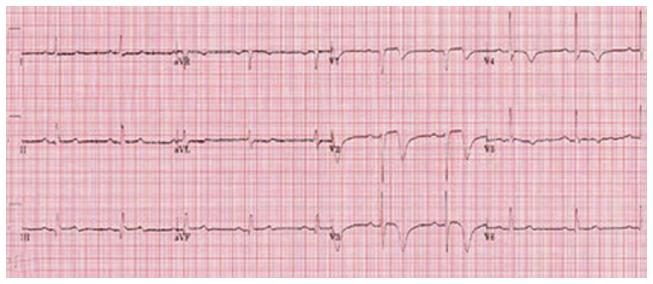
Figure 2 Patient 2.
An electrocardiographic (ECG) tracing, illustrating the negative T-wave with minimal ST segment elevation in the precordial leads V1-4, of a 82-year-old-female patient presented with acute coronary syndrome due to non ST elevation myocardial infarction. Her previous medical history included hormonal substitution for hypothyroidism, ablatio retinae, polymylagia rheumatica, arterial hypertension, mild concentric left ventricular hypertrophy, aortic valvular stenosis with a peak gradient of 18 mmHg and mild aortic regurgitation grade 2/4. In 2011, analysis with ambulatory ECG recording for a syncopal attack revealed no abnormalities. Transthoracic echocardiography demonstrated apicoinferior hypokinesia. The patient was treated medically and remained free of symptoms. Her maintenance drug therapy consisted of BB, aspirin (ASA), clopidogrel, Angiotensin-II antagonist, prednisolon, diuretic and statin.
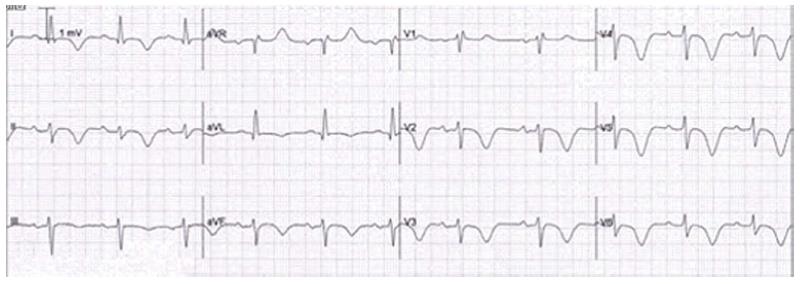
Figure 3 Patient 3.
An electrocardiographic (ECG) tracing, illustrating the negative T-wave in the precordial leads V2-6, of a 72-year-old-woman who underwent 6 mo earlier direct current electric cardioversion for persistent atrial fibrillation. Her concomitant medical history includes temporal arteritis, carotid endarterectomy and cluster headache. She presented with abnormal rest ECG during out-patient follow-up. Her spouse died 2 wk prior to presentation. The cardiac markers were minimally elevated. The diagnosis of Takotsubo cardiomyopathy was strongly suggested as the emotional stress may have been the trigger. Transthoracic echocardiography depicted biventricular normokinesia with hypertrophic LV. Pulmonary perfusion-ventilation scintigraphy, Coronary angiography and cardiac MRI were all normal. She did well on pharmacological treatment with oral vit K antagonist, class 3 antiarrhythmic drug, anti-depressive drug and diuretics. The ECG alterations returned to baseline over a 6 mo period.
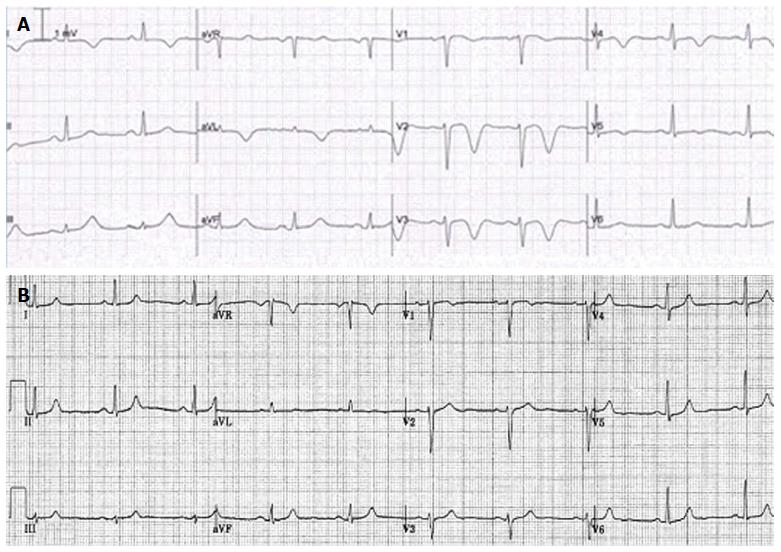
Figure 4 Patient 4.
A: An electrocardiographic (ECG) tracing, demonstrating negative T wave in the precordial leads V2-5, of a 69-year female patient with past medical history of transient ischemic attack two years previously, presented with interscapular pain. She had no emotional or physical stress. Normal results were found on transthoracic echocardiography, perfusion-ventilation scintigraphy, Coronary angiography and cardiac MRI. Brain CT scan revealed mild cerebral atrophy and minimal ischemic changes; B: The ECG showed spontaneous regression in 2 mo time. The etiology of the negative T wave inversion remains undetermined. Her medical regimen included aspirin, beta blocker, statin and diuretic.
Figure 5 Patient 5.
An electrocardiographic (ECG) tracing, showing negative T wave in the precordial leads V1-3 and S1 Q3 T3, of a 55-year obese male patient without antecedent medical history presented with chest pain and minimally elevated serum cardiac biomarkers. Transthoracic echocardiography revealed dilated and hypokinetic RV with pulmonary hypertension and distended inferior caval vein. Coronary angiography was normal and pulmonary CT angiography confirmed the clinical diagnosis showing massive bilateral pulmonary embolism with central and peripheral localization. A continuous positive airway pressure was implemented for newly detected severe obstructive sleep apnea syndrome. He was successfully treated with medical regimen and on follow-up he became asymptomatic and the abnormal ECG findings gradually disappeared.
Figure 6 Patient 6.
An electrocardiographic (ECG)tracing, showing voltage criteria for left ventricular hypertrophy with ST depression and negative T wave in the precordial and inferior leads V3-6, of a 52-year female patient with non-obstructive hypertrophic cardiomyopathy (thickness of septum 20 mm and posterior wall of 24 mm without septal anterior movement or obstruction of outflow tract). Normal coronary arteries were found on coronary angiography. She refused genetic counseling and invasive intervention. She was treated medically with beta blocker.
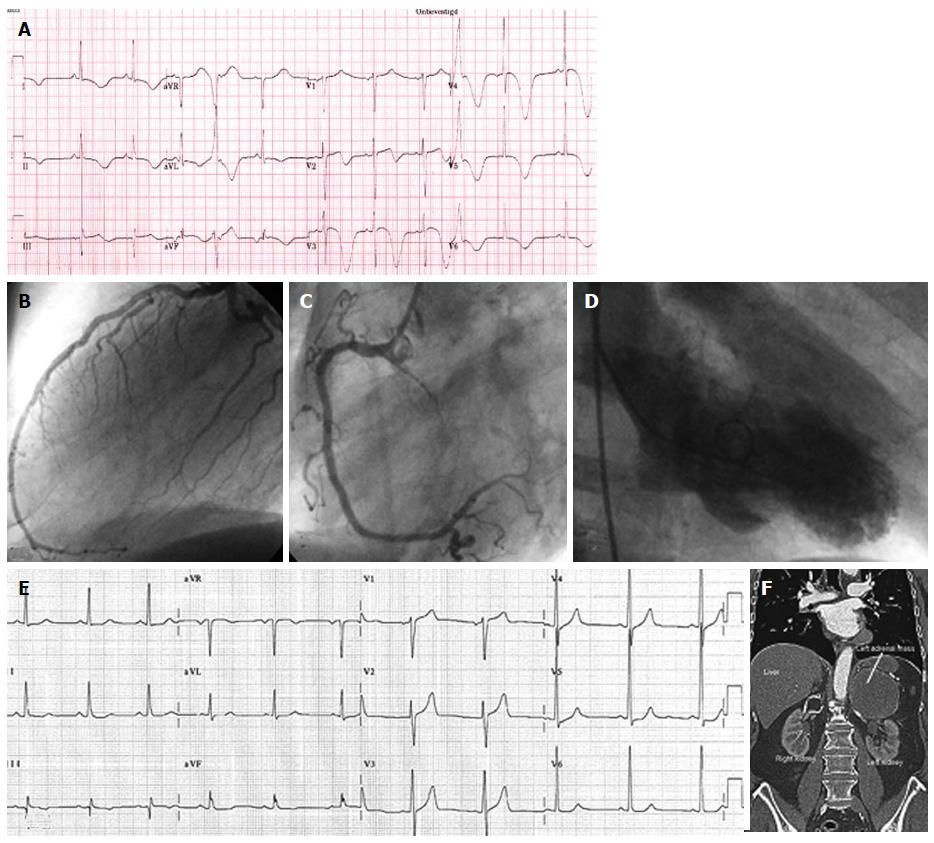
Figure 7 Patient 7.
A: An electrocardiographic (ECG) tracing, showing giant T wave inversion in the precordial leads V2-6, of a 76-year Caucasian male with a past medical history of an old inferior myocardial infarction, percutaneous coronary intervention of the right coronary artery (RCA) and left anterior descending coronary artery, acutely presented with left abdominal pain, psychomotor unrest, diaphoresis and blood pressure difference between the right and left arm. Acute aortic dissection was excluded as well as recurrent MI. Coronary angiography frame of (B) the left coronary artery and (C) the RCA depicting no significant stenosis of the arterial tree. Serum cardiac markers were slightly elevated. Echocardiographic (hypokinesia of the mid and apical regions and hyperkinesia of the basal segments) findings and (D) ventriculography (apical ballooning) were all compatible with Takotsubo cardiomyopathy; E: Base line ECG. The abdominal ultrasound and (F) CT demonstrated a pheochromocytoma in the left adrenal region which was confirmed with 123I-MIBG scan and dihydroxyphenylalanine-Positron Emission tomography and proved by pathological results. Plasma and urine metanephrin and normetanephrin were highly elevated. After removal of the hormonally active tumor, the patient became symptom free and the ECG normalized. The medical treatment continued including calcium reentry blocker, beta blocker, aspirin, angiotensin converting enzyme inhibitor, statin and an α-blocker.
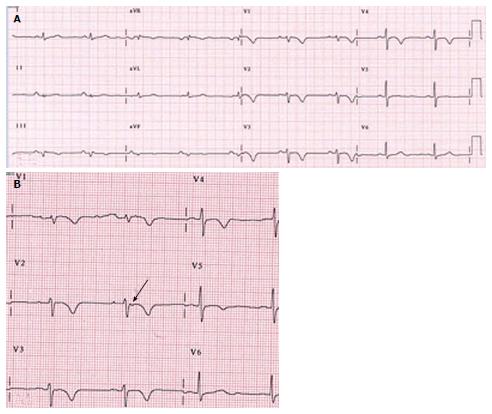
Figure 8 Patient 8.
Electrocardiographic (ECG) tracing, demonstrating negative T-wave in the precordial leads V1-5, microvoltage in the standard leads and an Epsilon wave (arrow) which can be appreciated on magnification of ECG lead V2, of a 73-year-old man, amateur marathon runner after successful resuscitation for OHCA due to ventricular fibrillation. His coronary angiography and transthoracic echocardiography were normal. Genetic counseling revealed mutation 1238C > A (Tyr616X) in the plakophilline2 gen, compatible with AC. He refused implantable cardioverter defibrillator implantation and remained on medical treatment including class III antiarrhythmic drug. He was advised to refrain from marathon running and other strenuous exercise.
- Citation: Said SA, Bloo R, Nooijer R, Slootweg A. Cardiac and non-cardiac causes of T-wave inversion in the precordial leads in adult subjects: A Dutch case series and review of the literature. World J Cardiol 2015; 7(2): 86-100
- URL: https://www.wjgnet.com/1949-8462/full/v7/i2/86.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i2.86