Copyright
©2014 Baishideng Publishing Group Inc.
World J Cardiol. Aug 26, 2014; 6(8): 836-846
Published online Aug 26, 2014. doi: 10.4330/wjc.v6.i8.836
Published online Aug 26, 2014. doi: 10.4330/wjc.v6.i8.836
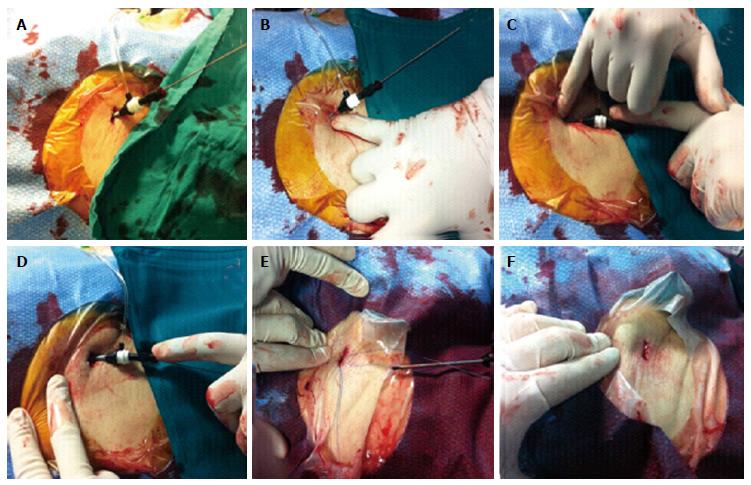
Figure 1 Pre-closure technique for hemostasis in transcatheter aortic valve implantation procedures.
After angiography-guided puncture of the anterior wall of the common femoral artery (CFA) and the insertion of a 6 F sheath, the preparation of vascular access for large sheath insertion (≥ 18 F) consists of the enlargement of the access site by the insertion of a 9 F sheath (A) and dilation of the subcutaneous tissue anteriorly (B) and posteriorly to the sheath (C), using one finger. Such a maneuver should achieve a less traumatic flaring of cutaneous and subcutaneous tissues at the vascular access site and create appropriate space for both large sheath introduction at the beginning of the procedure and optimal fastening of knots over the arterial wall at procedure end (D). After 9 F sheath removal, the suture-mediated vascular closure device is inserted in the correct position, the needles are unlocked and pulled through the arterial wall (E). At the end of transcatheter aortic valve implantation, the sheath and the guide wire are removed, the sutures are fastened individually with a sliding knot and a knot pusher is used to ensure approximation of the knot to the surface of the vessel wall. Vascular suture ends are cut well beneath the surface of the skin and an optimal closure of vascular access is obtained by a single cutaneous suture without residual bleeding (F).
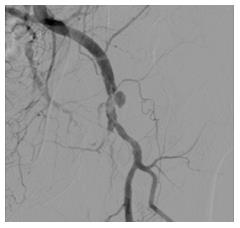
Figure 2 Post-transcatheter aortic valve implantation pseudoaneurysm.
After the transcatheter aortic valve implantation procedure, digital subtraction angiography of the left iliac-femoral artery by contralateral medium contrast injection showing a pseudoaneurysm of the left common femoral artery.
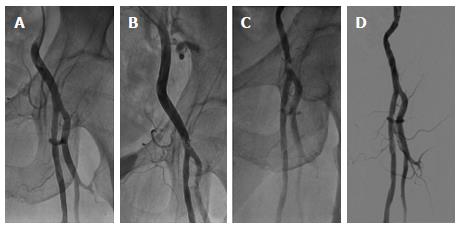
Figure 3 Post-transcatheter aortic valve implantation common femoral artery stenosis.
Standard angiography obtained before 18 F sheath insertion for transcatheter aortic valve implantation showed the absence of significant stenosis, tortuosity and calcification of left iliac-femoral artery (A); after vascular access closure by Prostar XL, angiography documented the presence of an intimal flap in the right common femoral artery (CFA) wall, not determining a significant flow limitation (B); 4-mo follow-up angiography showed progression of arterial damage and the development of significant stenosis of CFA, determining claudication (Fontaine-Leriche class IIb) (C); angioplasty of left CFA was performed by right transradial access, using a 125 cm 6 F Multipurpose guiding catheter and a 300 cm BMW Universal wire; a 4.0 mm x 15 mm non-compliant coronary balloon (NC Sprinter, Medtronic, North Carolina, United States) and a 6.0 mm x 20 mm peripheral balloon (Avion Plus, Invatec, Roncadelle, Italy) were inflated to 24 atm, obtaining an optimal final result (D).
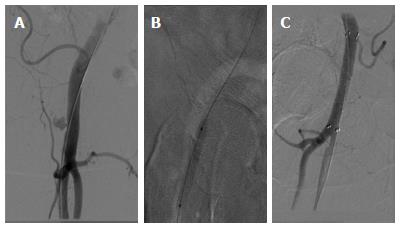
Figure 4 Post-transcatheter aortic valve implantation arterial perforation.
At the end of the transcatheter aortic valve implantation procedure, digital subtraction angiography of the right iliac-femoral artery showed a perforation of the right common femoral artery (CFA) (A); angioplasty of the right CFA was performed by the crossover approach via the contralateral iliac-femoral artery; a 7.0 mm x 40 mm peripheral balloon (Admiral Xtreme, Invatec, Roncadelle, Italy) was inflated to 10 atm at the perforation site (B); because of the persistence of hematic extravasation, a 8.0 mm x 60 mm covered stent (Fluency Stent-Graft, BARD Peripheral Vascular, AZ, United States) was implanted, followed by dilation of 7.0 mm x 40 mm and 8.0 mm x 20 mm balloons (Admiral Xtreme, Invatec, Roncadelle, Italy) to 12 atm. At final angiography, optimal sealing of the arterial breach without residual hematic extravasation was documented (C).
Figure 5 Post-transcatheter aortic valve implantation arterial dissection.
Post- transcatheter aortic valve implantation procedure, angiography of the right iliac-femoral axis via the contralateral groin showing a dissection of the right common femoral artery extending proximally to the external iliac artery and determining distally an occlusion of the superficial femoral artery (A); digital subtraction angiography after reaching true lumen by a .035” wire by the retrograde approach and peripheral balloon dilation (6.0 mm x 120 mm Admiral Xtreme, Invatec, Roncadelle, Italy) to 6 atm (B); final angiography after stenting (6.0 mm x 80 mm and 9.0 mm x 60 mm Lifestent Vascular Stent, BARD Peripheral Vascular, AZ, United States) and post-dilation (5.0 mm x 80 mm and 6.0 mm x 120 mm Admiral Xtreme; Invatec, Roncadelle, Italy) showing an optimal antegrade flow in the right iliac-femoral artery (C).
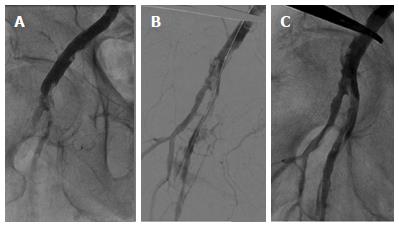
Figure 6 Post-transcatheter aortic valve implantation arterial thrombosis.
Post-transcatheter aortic valve implantation procedure, digital subtraction angiography showing acute thrombotic occlusion of the right common femoral artery (A); emergency percutaneous transluminal angioplasty was performed by the crossover approach via the contralateral femoral artery, and consisted of initial thromboaspiration using a 6 F Multipurpose guiding catheter (Vista Brite Tip, Cordis Inc., Miami Lakes, FL, United States), obtaining restoration of antegrade blood flow (B); after prolonged dilations by 5.0 mm × 40 mm and 6.0 mm × 40 mm balloons (Pacific Xtreme and Admiral Xtreme, Invatec, Roncadelle, Italy), a 7.0 mm × 20 mm stent (Cristallo Ideale, Invatec, Roncadelle, Italy) was implanted, dilated by a 7.0 mm × 30 mm balloon (Avion Plus, Invatec, Roncadelle, Italy) to 10 atm. Final angiography showed the absence of residual stenosis (C).
- Citation: Dato I, Burzotta F, Trani C, Crea F, Ussia GP. Percutaneous management of vascular access in transfemoral transcatheter aortic valve implantation. World J Cardiol 2014; 6(8): 836-846
- URL: https://www.wjgnet.com/1949-8462/full/v6/i8/836.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i8.836