Copyright
©2014 Baishideng Publishing Group Inc.
World J Cardiol. Jun 26, 2014; 6(6): 462-477
Published online Jun 26, 2014. doi: 10.4330/wjc.v6.i6.462
Published online Jun 26, 2014. doi: 10.4330/wjc.v6.i6.462
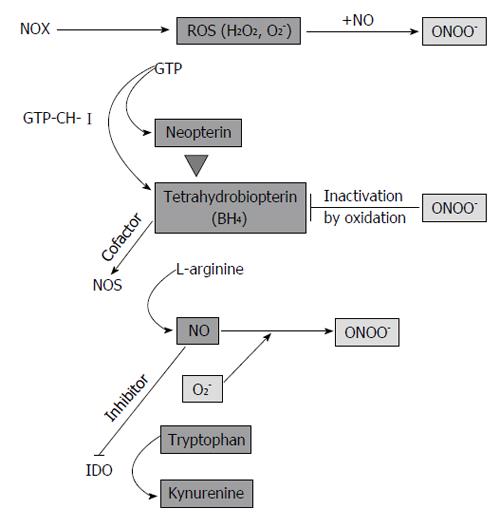
Figure 1 Regulatory circuits in inflammation and endothelial dysfunction.
During inflammation, NADPH oxidase (NOX) produces high levels of reactive oxygen species (ROS). T cells and natural killer cells produce interferon-γ, which activates enzyme GTP-cyclohydrolase I (GTP-CH-I), indoleamine 2,3-dioxygenase (IDO) and inducible nitric oxide synthase (iNOS) in monocyte-derived macrophages (M) and dendritic cells (DC). In endothelial cells, endothelial NOS (eNOS) is constitutively expressed and GTP-CH-I produces tetrahydrobioterin (BH4), which is a NOS cofactor. BH4 deficiency leads to NOS uncoupling and superoxide anion (O2-) formation, which reacts with NO to form peroxynitrite (ONOO-). In a vicious cycle, ONOO- oxidizes BH4. In M/DC, GTP-CH-I synthesizes neopterin at expense of BH4, which contributes to the low activity of iNOS in human M/DC. Furthermore, NO is a reversible inhibitor of the immunoregulatory enzyme IDO. IDO degrades the essential amino acid tryptophan to kynurenine.
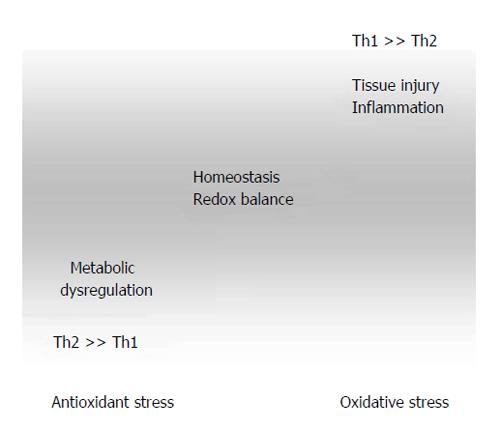
Figure 2 Dysregulation of redox- and Th1/Th2-balance in the course of atherogenesis.
Excessive antioxidant intake in combination with other risk factors such as high caloric diet and low physical exercise lead to suppression of Th1-type immunity, thereby favoring Th2-associated development of allergies and asthma and promoting juvenile obesity. Factors such as high blood pressure and hyperlipidemia lead to shear stress and tissue injury. Inflammatory reactions are associated with high reactive oxygen species generation, which results in immunotoxicity due to oxidation of biomolecules (lipids, proteins, etc.).
- Citation: Mangge H, Becker K, Fuchs D, Gostner JM. Antioxidants, inflammation and cardiovascular disease. World J Cardiol 2014; 6(6): 462-477
- URL: https://www.wjgnet.com/1949-8462/full/v6/i6/462.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i6.462