Copyright
©2014 Baishideng Publishing Group Co.
World J Cardiol. Apr 26, 2014; 6(4): 175-182
Published online Apr 26, 2014. doi: 10.4330/wjc.v6.i4.175
Published online Apr 26, 2014. doi: 10.4330/wjc.v6.i4.175
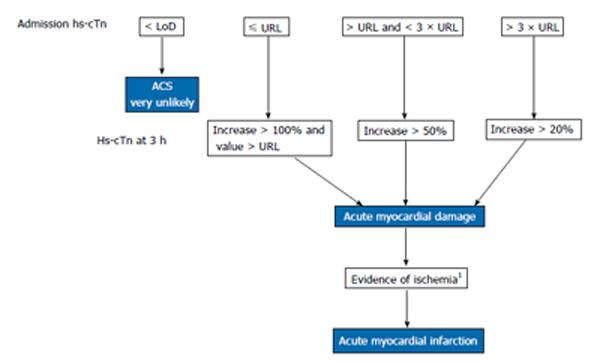
Figure 1 Algorithm for the rapid evaluation of clinically suspected acute myocardial infarction with high-sensitivity cardiac troponin testing.
This algorithm is based on best current knowledge and may have to be modified with upcoming new data. This approach at least guarantees that the changes will be above the analytical and biological variation. It is important to note that hs-cTn changes over a 3 h period in patients presenting late after AMI onset may be less than 20%. For hs-cTnT some studies favour absolute changes over relative concentration changes. 1Evidence of acute myocardial ischemia by new ECG changes and/or new imaging corroborations. Hs-cTn: High-sensitivity cardiac troponin; URL: 99th percentile upper reference limit of healthy controls; ACS: Acute coronary syndrome; LoD: Lower limit of detection; AMI: Acute myocardial infarction; ECG: Electrocardiogram.
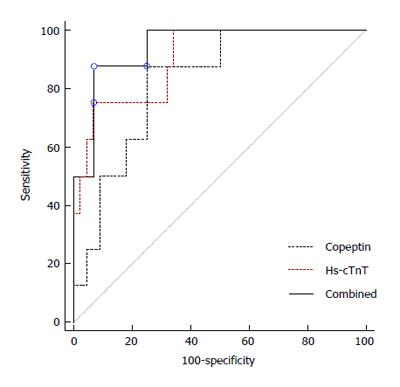
Figure 2 Diagnostic performances of high-sensitivity troponin T and copeptin for the diagnosis of acute myocardial infarction in chest pain patients.
Own unpublished results, the area under receiver operator characteristic curves of the combination of copeptin with hs-cTnT (0.94) was not significantly different from the area under hs-cTnT curve (0.90). The worthless test is indicated as reference line. Hs-cTnT: High-sensitivity cardiac troponin T.
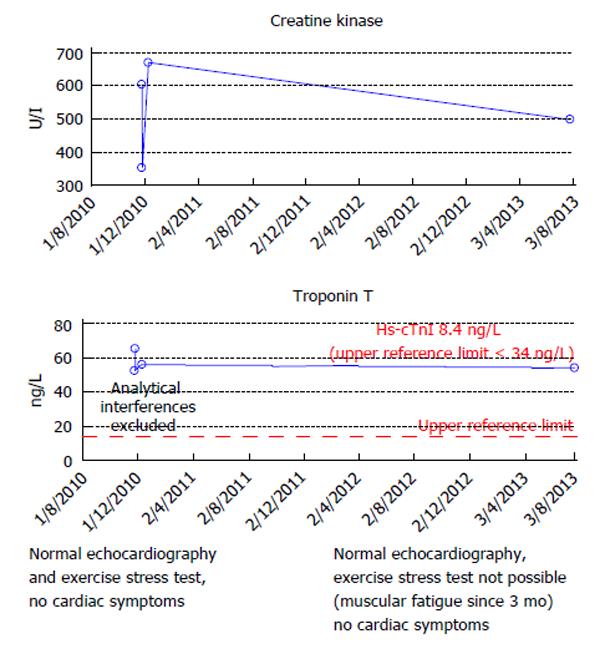
Figure 3 Creatine kinase and high-sensitivity cardiac troponin T and I in a 72-year-old male with late onset limb-girdle muscular dystrophy.
This patient presented first to our outpatient clinic in 2010 because of clinically unexplained increased high-sensitivity cardiac troponin T (hs-cTnT) concentrations. The echocardiography, exercise stress test and renal function were completely normal, the patient was free of any cardiac symptoms. In 2010 analytical interferences with the hs-cTnT assay were excluded by serial dilution experiments and an interference by heterophilic antibodies could be ruled out by addition of antibody blocking agents to the sample. There was no evidence for macro creatine kinase as well. As the patient had no cardiac symptoms or symptoms suggesting skeletal muscle disease no further work-up was done. In 2013 the patient developed typically symptoms of muscular dystrophy and was again seen in our outpatient clinic. The electrocardiogram and echocardiogram remained normal, he still had no cardiac symptoms but an exercise stress test was no longer possible because of skeletal muscle fatigue. At this visit we found a marked discrepancy between hs-cTnT (moderately increased) and hs-cTnI (normal) suggesting a release of hs-cTnT from chronically injured skeletal muscle by previously already described reexpression of cardiac cTnT isoforms. In retrospect, unexplained hs-cTnT increase in this patient was an early sign of late onset muscular dystrophy.
- Citation: Mair J. High-sensitivity cardiac troponins in everyday clinical practice. World J Cardiol 2014; 6(4): 175-182
- URL: https://www.wjgnet.com/1949-8462/full/v6/i4/175.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i4.175