Copyright
©2014 Baishideng Publishing Group Inc.
World J Cardiol. Nov 26, 2014; 6(11): 1175-1191
Published online Nov 26, 2014. doi: 10.4330/wjc.v6.i11.1175
Published online Nov 26, 2014. doi: 10.4330/wjc.v6.i11.1175
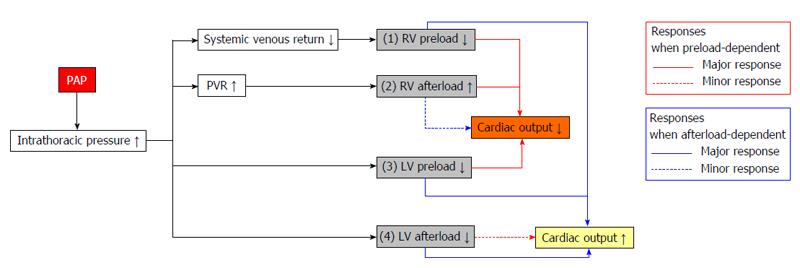
Figure 1 Effects of positive airway pressure on hemodynamics.
First, PAP decreases systemic venous return and RV preload by increasing intrathoracic pressure; Second, PAP increases PVR by increasing lung volume. Thus, it is possible that RV afterload can be increased by PAP; Third, a decrease in RV preload and an increase in RV afterload lead to reductions in pulmonary venous return and limitations of LV inflow, filling and preload; Fourth, increased intrathoracic pressure relative to atmospheric pressure causes a pressure difference between the intrathoracic and extrathoracic cavities. Therefore, PAP may decrease LV afterload. In subjects without HF who are generally preload-dependent or in HF patients who manifest preload-dependent reduction, decreased RV and LV preload in addition to the increase in RV afterload may cause a net decrease in cardiac output, whereas a decrease in LV afterload may cause a minor response toward increasing cardiac output. Conversely, patients with HF are more sensitive to decreased afterload and are thus predominantly afterload-dependent. PAP therapy causes a net increase in cardiac output through decreases in RV preload, LV preload and afterload, whereas an increase in RV afterload may cause a minor response toward decreasing cardiac output. LV: Left ventricular; PAP: Positive airway pressure; PVR: Pulmonary vascular resistance; RV: Right ventricular; HF: Heart failure.
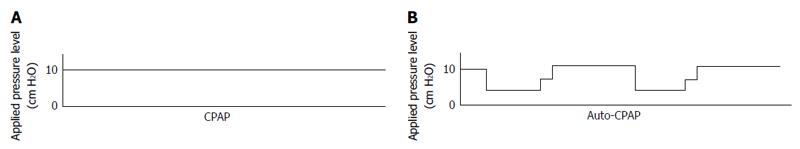
Figure 2 Differences between continuous positive airway pressure and automated continuous positive airway pressure.
A: CPAP provides a constant level of positive pressure to the airway during spontaneous breathing; B: Automated CPAP devices are designed to detect various degrees of upper airway obstruction and consequently adjust the pressure level to keep the airway open. CPAP: Continuous positive airway pressure.
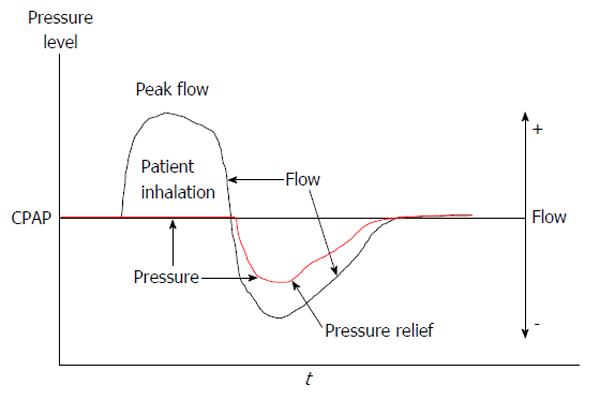
Figure 3 Algorithm of early expiratory phase pressure relief.
The pressure is lowered in the early phase of expiration to enhance comfort, but the pressure returns to the critical pressure needed to keep the airway open before the next inspiration. CPAP: Continuous positive airway pressure.
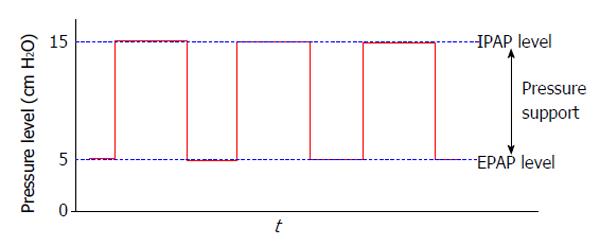
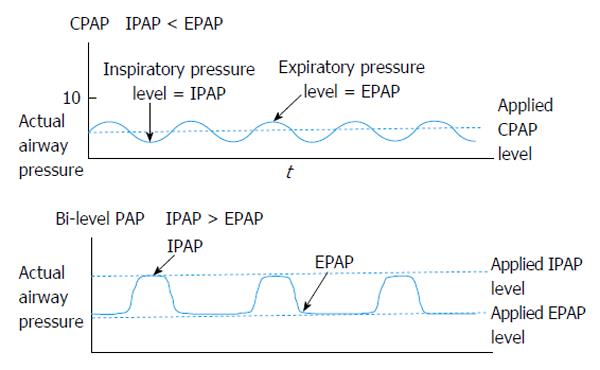
Figure 4 Bi-level positive airway pressure.
Bi-level PAP provides two fixed levels of PAP, a higher level of pressure during inspiration (i.e., IPAP) and a lower level of pressure during expiration (i.e., EPAP), and thus provides pressure support during inspiration. EPAP: Expiratory positive airway pressure; IPAP: Inspiratory positive airway pressure; PAP: Positive airway pressure.
Figure 5 Differences in actual airway pressure between continuous positive airway pressure and bi-level positive airway pressure.
While on CPAP, although a constant CPAP level is applied, actual airway pressure is not constant and oscillates. During inspiration, actual airway pressure decreases below the applied CPAP level, whereas during expiration, actual airway pressure increases above the applied CPAP level. Thus, the inspiratory pressure level in the airway (i.e., IPAP) is lower than the expiratory pressure level in the airway (i.e., EPAP). Conversely, while on bi-level PAP, the actual airway pressure increases during inspiration due to pressure support. Thus, IPAP is greater than EPAP according to the level of pressure support. CPAP: Continuous positive airway pressure; EPAP: Expiratory positive airway pressure; IPAP: Inspiratory positive airway pressure; PAP: Positive airway pressure.
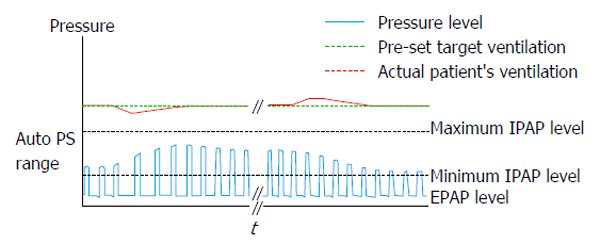
Figure 6 Volume assured pressure support.
Using the volume assured pressure support mode, the device alters the level of pressure support from the minimum to maximum levels to maintain the pre-set ventilation or pre-set target tidal volume. This figure shows algorithm based on ventilation. EPAP: Expiratory positive airway pressure; IPAP: Inspiratory positive airway pressure; PS: Pressure support.
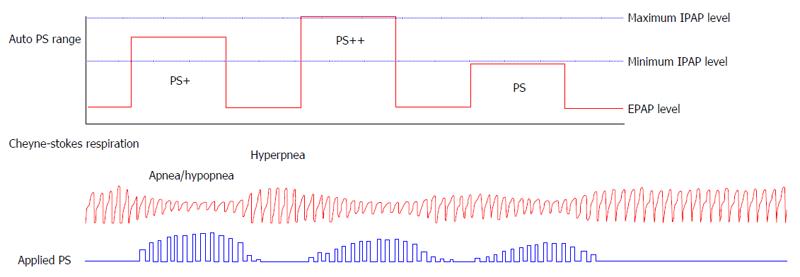
Figure 7 Adaptive servo-ventilation.
Adaptive servo-ventilation devices automatically provide altering pressure support for each inspiration, ranging from a pre-set minimum level to a pre-set maximum level, to maintain moving target ventilation (determined based on volume or flow) determined by the patient’s current breathing in addition to the back-up ventilation with variable respiratory rates. This stabilizes the abnormal breathing pattern (i.e., cheyne-stokes respiration) and maintains the PaCO2 levels to prevent hypocapnia, which can otherwise trigger apnea reentry cycles. EPAP: Expiratory positive airway pressure; IPAP: inspiratory positive airway pressure; PaCO2: Arterial partial pressure of carbon dioxide; PS: Pressure support.
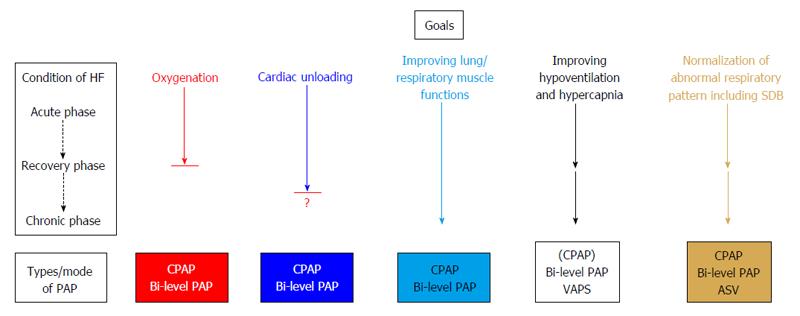
Figure 8 Importance of each goal of positive airway pressure therapy according to different heart failure conditions.
In the wide spectrum of HF care, PAP therapy is used to help oxygenation, provide relief from cardiac load, improve lung and respiratory muscle function, reduce hypoventilation and hypercapnia, and normalize abnormal respiratory patterns, including SDB. The importance of each goal can differ according to the condition of HF. Improving oxygen is one of the most important goals in the acute phase. However, after recovery from acute decompensation, this goal becomes less important or is no longer considered. Providing cardiac unloading is another important goal in the acute phase to the recovery phase. However, the importance of this goal remains to be elucidated after recovery from acute decompensation. Improving lung and respiratory muscle function is sometimes important in the acute phase and after recovery. Improving hypoventilation is important in cases with hypercapnia in the acute phase. In addition, HF patients with hypoventilation and daytime hypercapnia can be treated by PAP therapy in the recovery or chronic phase. Normalization of abnormal respiratory patterns, particularly SDB suppression, is sometimes important in the recovery phase and is most important in the chronic phase. The specific types/modes of PAP that should be used differ according to each therapeutic purpose. ASV: Adaptive servo-ventilation; CPAP: Continuous positive airway pressure; HF: Heart failure; PAP: Positive airway pressure; SDB: Sleep disordered breathing; VAPS: Volume assured pressure support.
- Citation: Kato T, Suda S, Kasai T. Positive airway pressure therapy for heart failure. World J Cardiol 2014; 6(11): 1175-1191
- URL: https://www.wjgnet.com/1949-8462/full/v6/i11/1175.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i11.1175