Copyright
©2012 Baishideng Publishing Group Co.
World J Cardiol. Apr 26, 2012; 4(4): 103-111
Published online Apr 26, 2012. doi: 10.4330/wjc.v4.i4.103
Published online Apr 26, 2012. doi: 10.4330/wjc.v4.i4.103
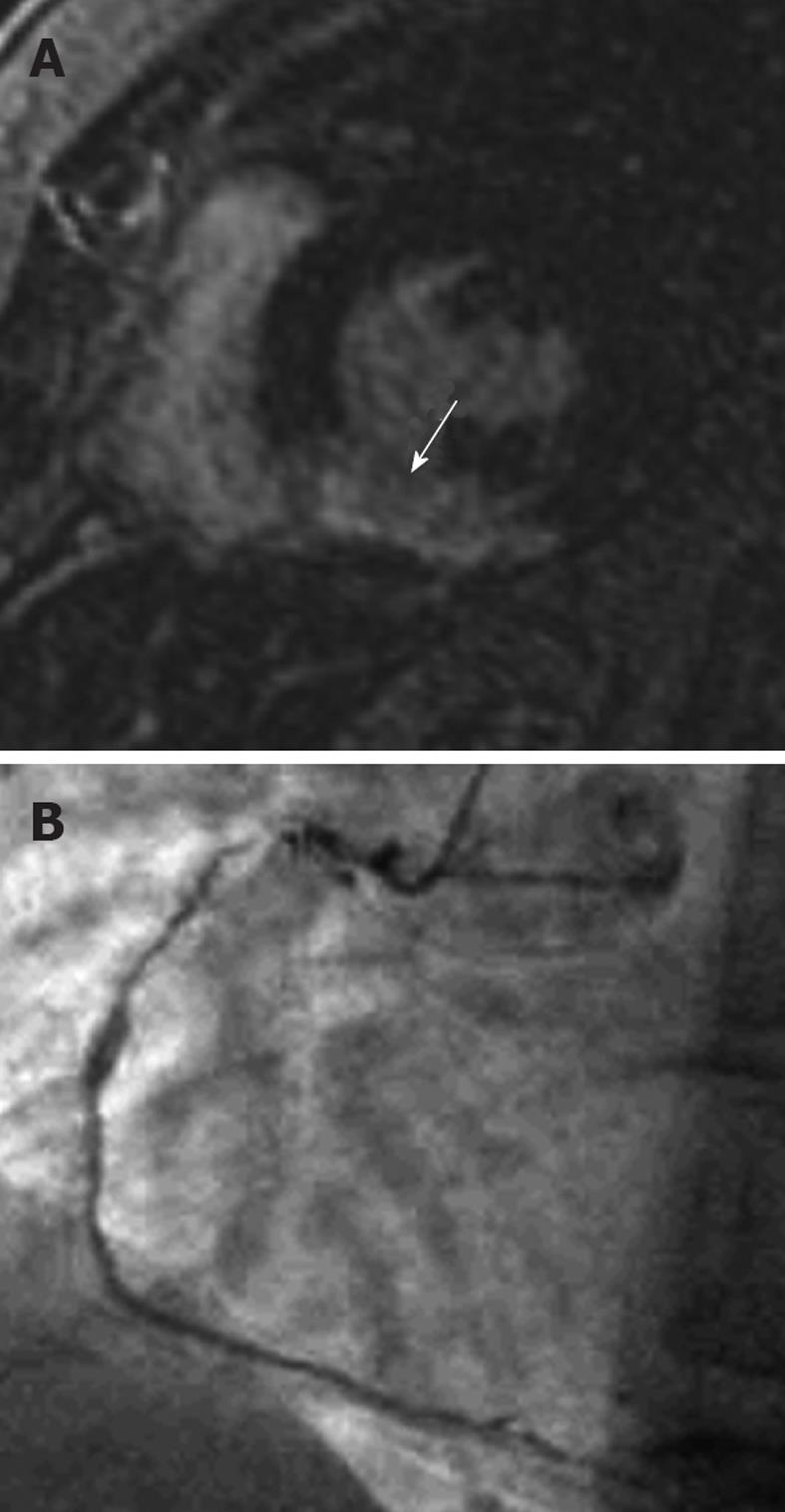
Figure 1 A 42-year-old female who presented with acute chest pain to the emergency department.
She had no risk factors for coronary artery disease and the clinical suspicion was of myocarditis. A: Late-enhancement short axis sequence shows a transmural area (arrow) of high signal involving the inferior segment consistent with an acute myocardial infarction involving the right coronary artery territory. Note that it is an acute rather than chronic infarct, because there is no wall thinning; B: An invasive angiogram confirmed diffuse coronary artery disease throughout the right coronary artery. Note that the likelihood of recovery of this segment with revascularization is extremely low because it is a transmural infarct.
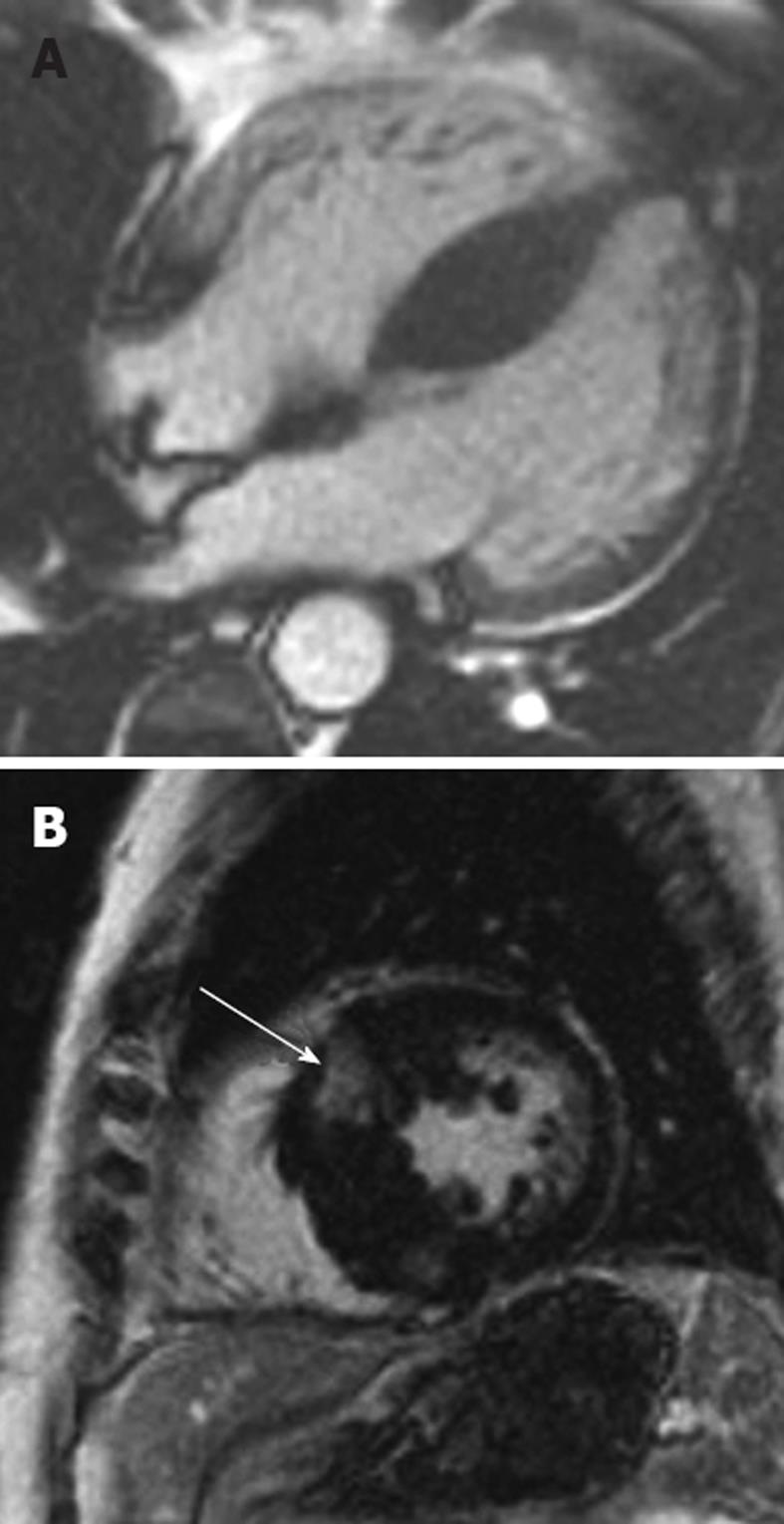
Figure 2 Hypertrophic cardiomyopathy.
A: 28-year-old man who presented with progressive heart failure and palpitations. The horizontal long-axis steady-state free precession sequence demonstrates a hypertrophic interventricular septum measuring 23 mm (normal ≤ 11 mm) consistent with hypertrophic cardiomyopathy (HCM); B: Late-enhancement short-axis image shows late-enhancement in the hypertrophied septum (arrow). Note that there are 2 abnormal areas of enhancement corresponding to the right superior and inferior ventricular insertion points. This is a characteristic pattern in HCM. Such late-enhancement has prognostic implications for patients with HCM, being associated with an increased prevalence of heart failure admissions, deterioration to New York Heart Association functional class III or IV, or heart failure-related death.
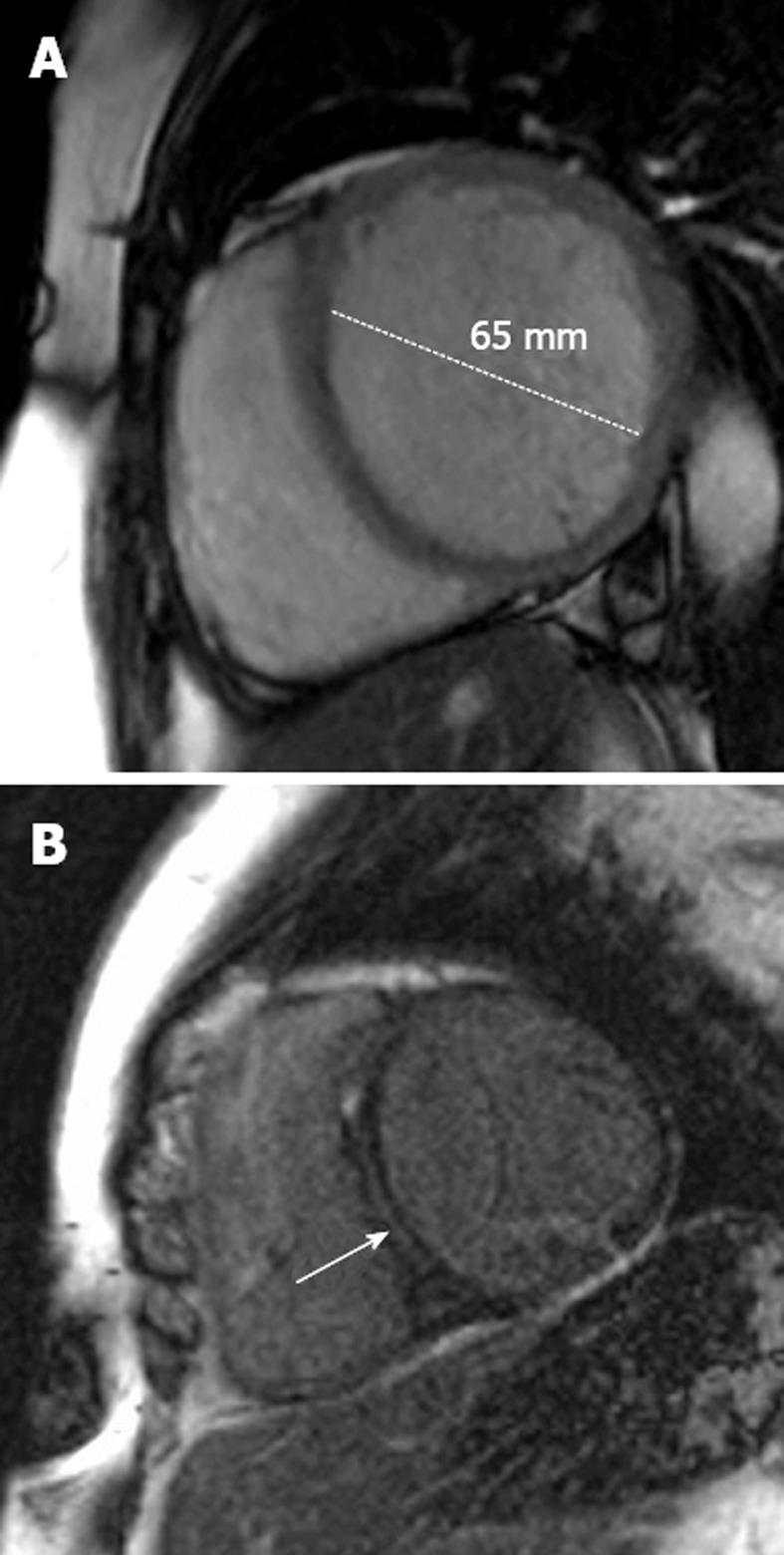
Figure 3 Dilated cardiomyopathy.
A: A 48-year-old man with progressive shortness of breath. The short-axis steady-state free precession sequence demonstrates a dilated left ventricle with a thin wall characteristic of dilated cardiomyopathy (DCM); B: Late-enhancement short-axis image shows late-enhancement in the interventricular septum (arrow). This is a characteristic location for fibrosis detection in idiopathic DCM and effectively excludes an ischemic etiology. Such late-enhancement has prognostic implications for patients with idiopathic DCM, being associated with an increased prevalence of all-cause death, hospitalization, sudden cardiac death and ventricular tachycardia.
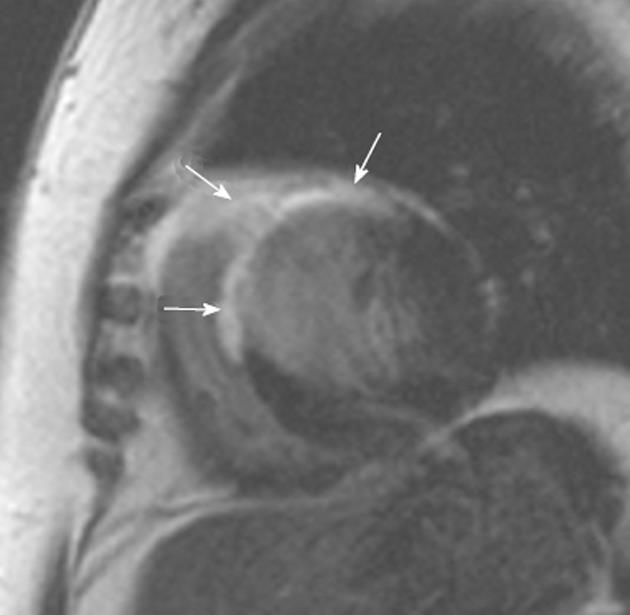
Figure 4 Cardiac sarcoidosis.
A 54-year-old woman who presented with recurring palpitations and progressive shortness of breath for several months before suddenly collapsing. Cardiac magnetic resonance imaging demonstrates extensive scarring throughout the anterior and anteroseptal segments of the left ventricle (arrows). However, the involvement of the anterior segment of the right ventricle is unusual for ischemia and suggests another cause for the images. An endomyocardial biopsy revealed cardiac sarcoidosis. There was no previous history of lung or mediastinal sarcoid.
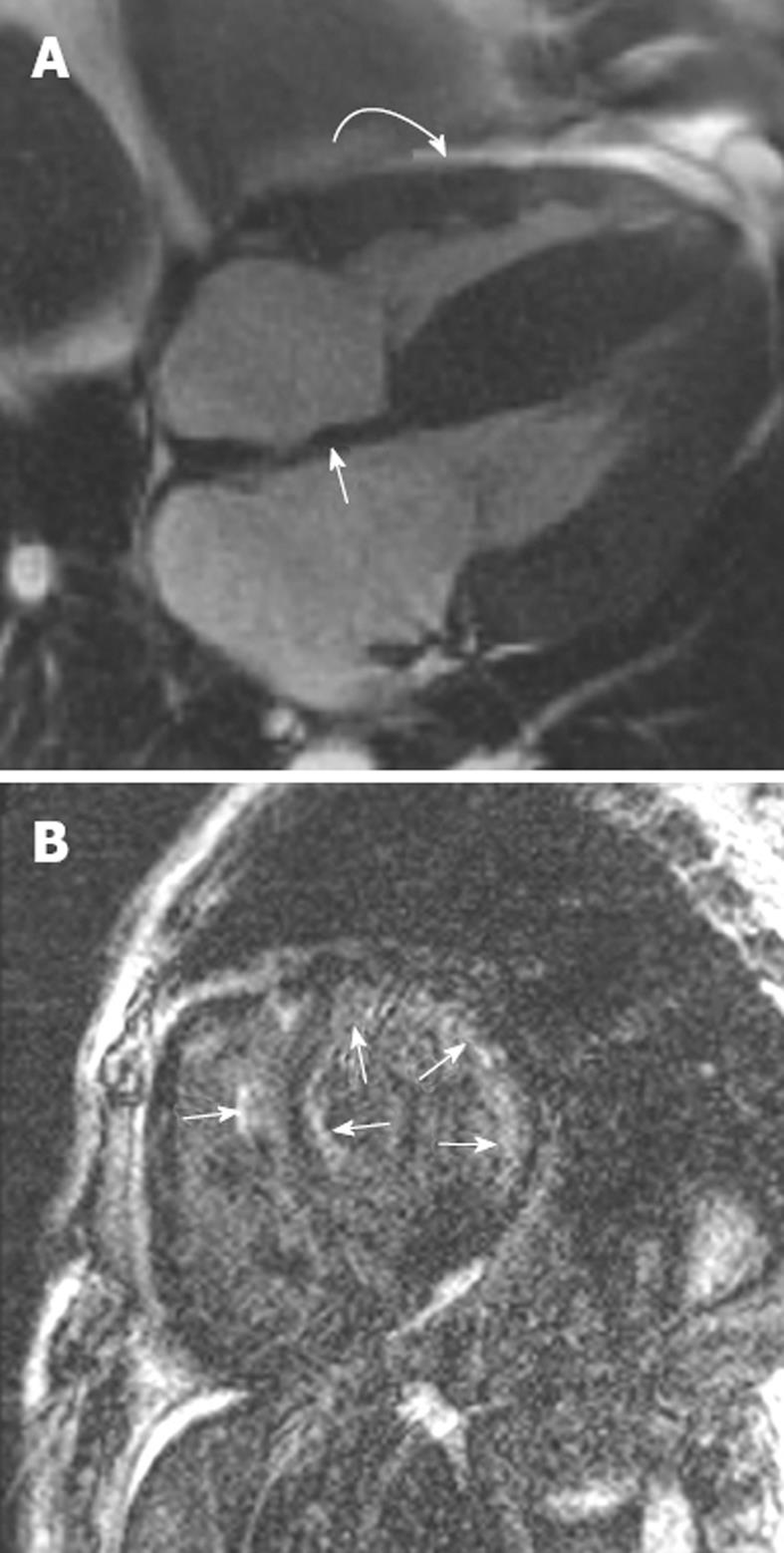
Figure 5 Right ventricular endomyocardial biopsy showed cardiac amyloid.
A: Horizontal long axis steady-state free precession sequence showing hypertrophy of the basal segments of the left ventricle (straight arrow), and bi-atrial enlargement and thickening of the interatrial septum (curved arrow). Note the small pericardial effusion; B: Late-enhanced sequence shows a circumferential subendocardial high signal. Note the high signal on the right ventricular side of the interventricular septum resulting in the tram track sign (arrow). Note also the small pericardial effusion.
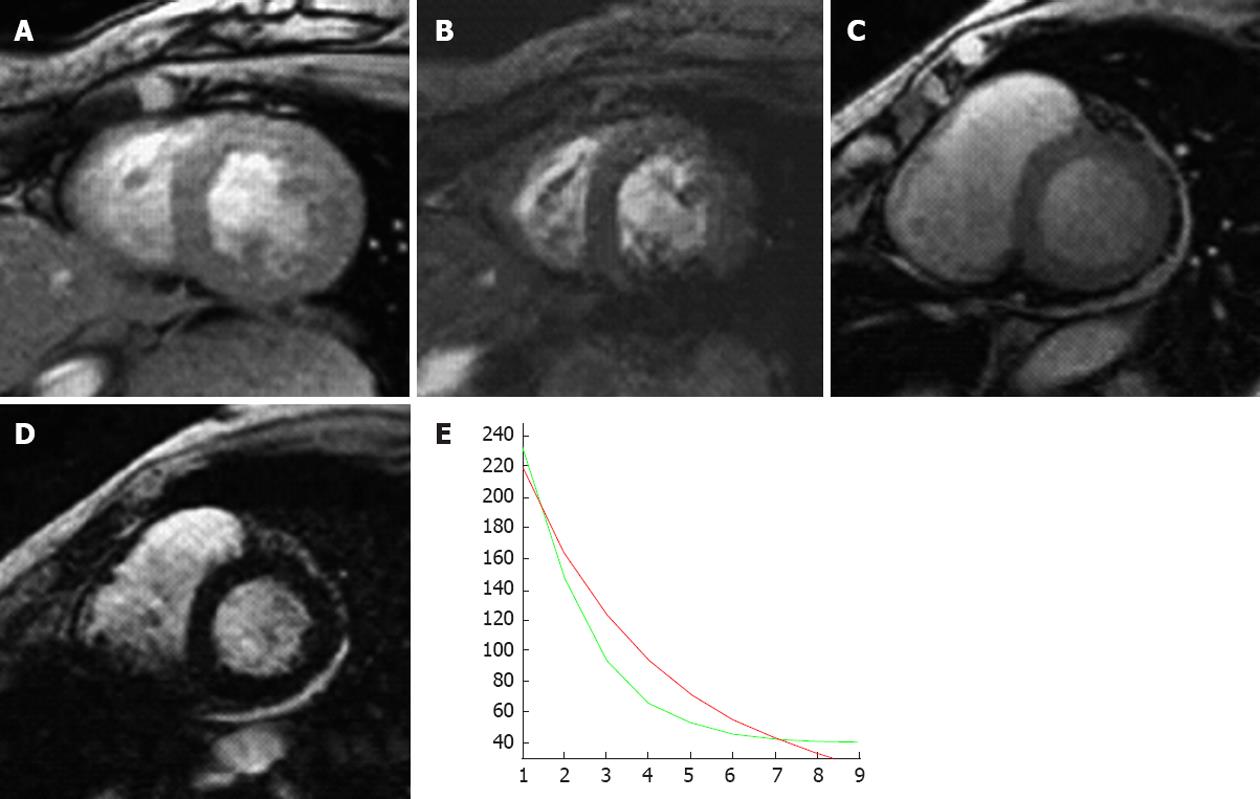
Figure 6 A 79-year-old woman with myelodysplasia treated with blood transfusions over many years.
A (echo time 10 ms) and B (echo time 20 ms) are two short axis T2star sequences from a normal patient with no evidence of myocardial iron overload; C (echo time 10 ms) and D (echo time 20 ms) are from the patient with myelodysplasia showing a progressive loss of signal with increasing T2 echo time indicating shortened T1 relation secondary to iron infiltration; E: Graph of decreasing T1 relaxation times (green line) compared with a normal patient (red line).
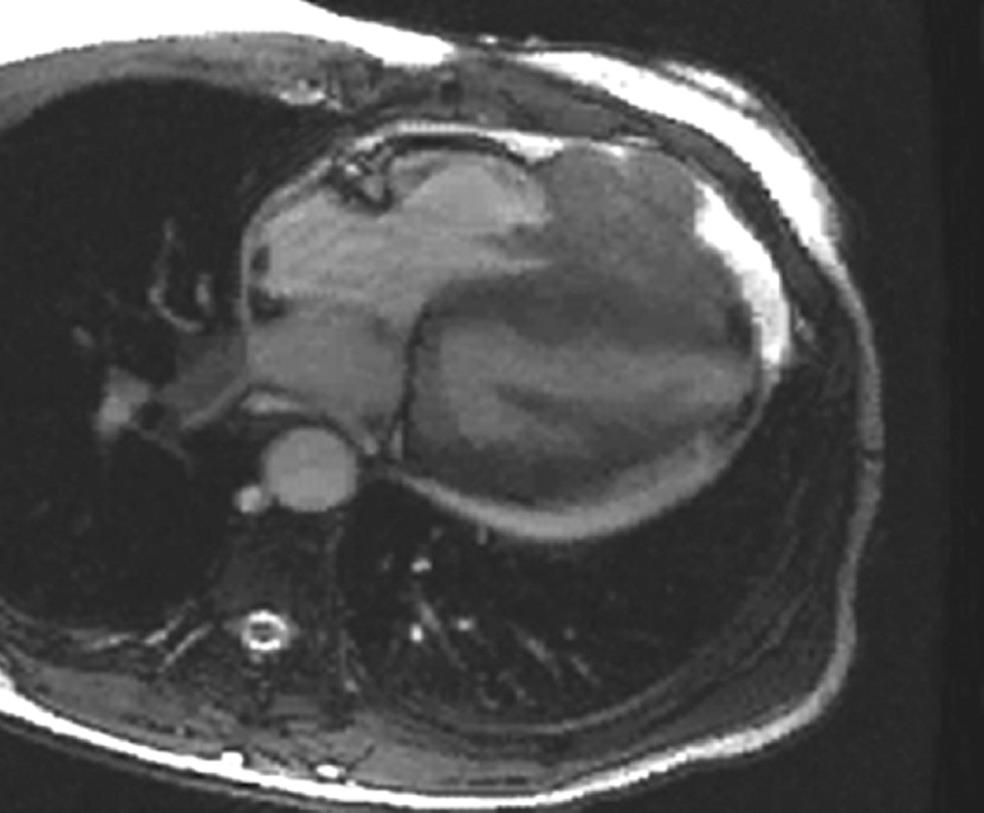
Figure 7 A 72-year-old woman with metastatic breast cancer to the heart.
Note the location of the metastatic nodules in the right heart chambers, the infiltration through the right ventricular free wall, the pericardial effusion and the pericardial metastasis. Any infiltrative appearing cardiac mass involving the right heart chambers in the presence of a pericardial effusion should be considered suspicious for malignancy.
- Citation: McDermott S, O’Neill AC, Ridge CA, Dodd JD. Investigation of cardiomyopathy using cardiac magnetic resonance imaging part 1: Common phenotypes. World J Cardiol 2012; 4(4): 103-111
- URL: https://www.wjgnet.com/1949-8462/full/v4/i4/103.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i4.103