Copyright
©The Author(s) 2022.
Figure 1 Radiation protection in the catheterization lab should be based on four principles.
Time: radiation dose depends linearly on the exposure time. Distance: The amount of radiation exposure depends on the distance from the source proportionally to the inverse of the distance squared from the X-ray source, so staff can lower their exposure levels by a factor of four by doubling their distance from the source. Shielding: barriers of lead protection can be accomplished with different forms such as personal protective equipment or mobile shields. The greater the shielding around the source, the smaller the exposure. Education: training and education in radiation protection is one of the basic components of radiation protection programs.
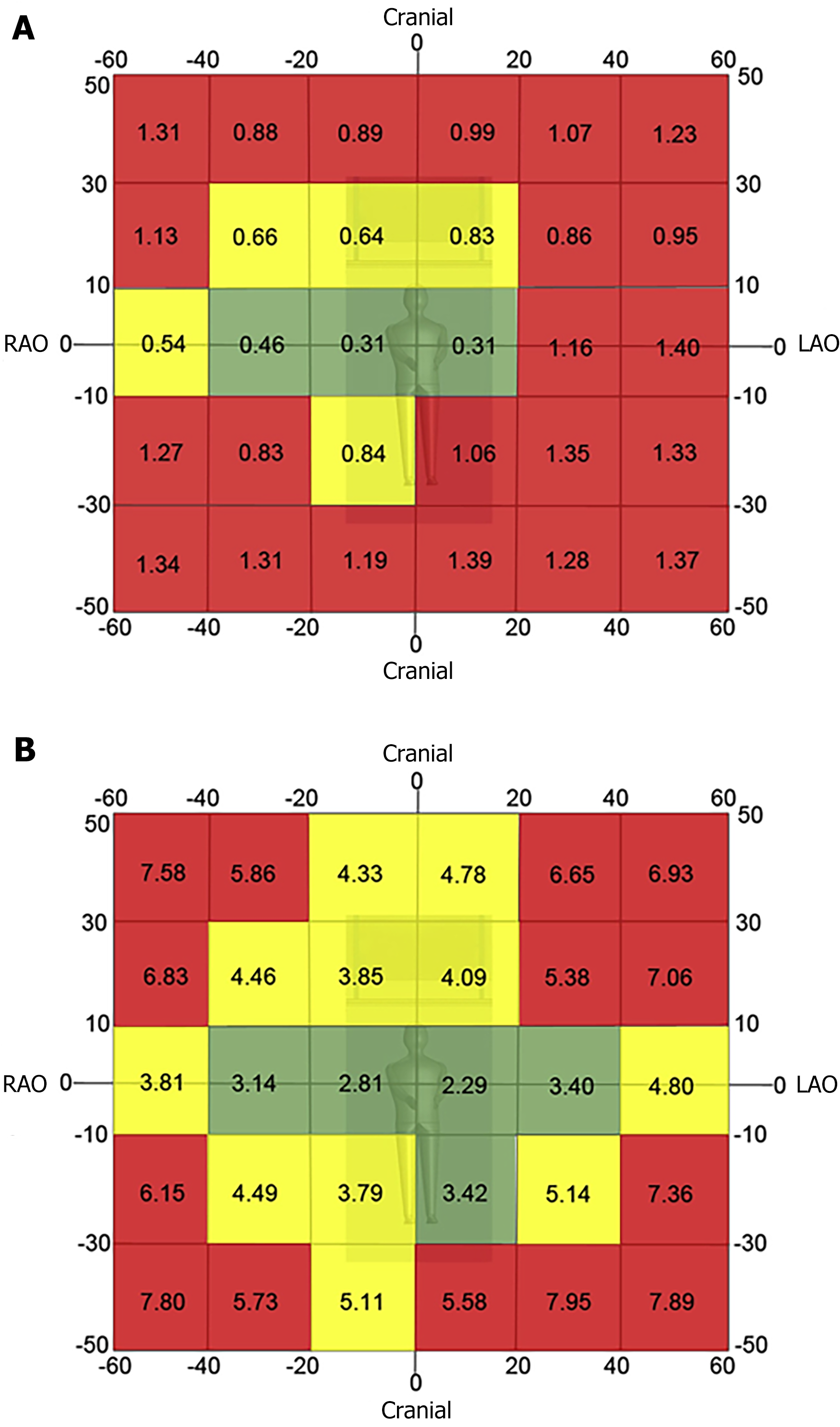
Figure 2 Two-dimensional radiation map for fluoroscopy (A) and acquisition imaging (B).
The red zone denotes projections where < 26% of the image procurement occurred in the lowest tertile of Air Kerma rate. The yellow zone denotes projection where 26% to 40% of the images were procured in the lowest tertile of air kerma rate the value in each cell represents the median Air Kerma rate for the respective projection. Reproduced with permission from reference 8[3]. LAO: Left anterior oblique view; RAO: Right anterior oblique view.
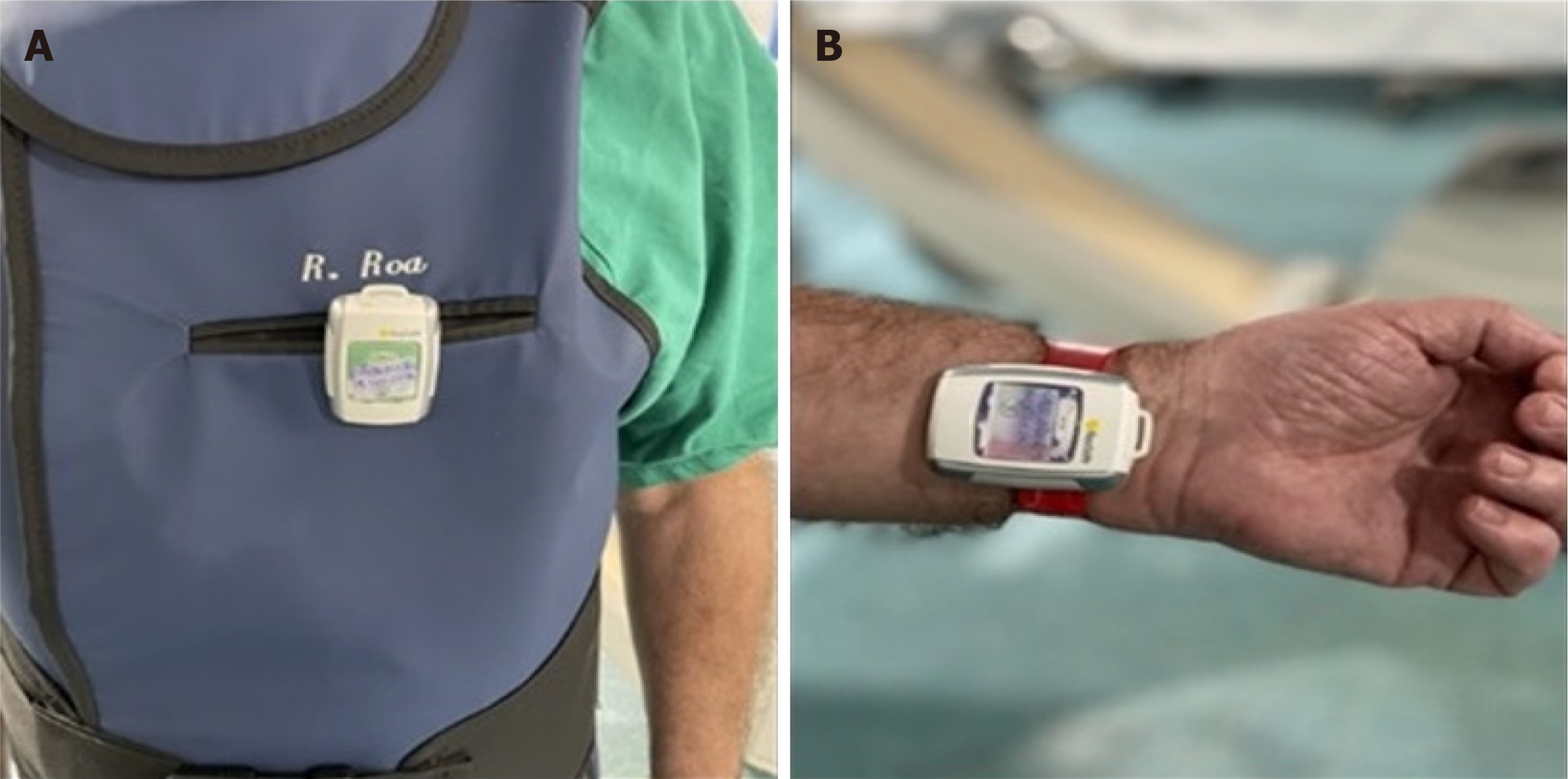
Figure 3 Real time electronic personal dosimeters placed over the apron (A) and on the left wrist of the operator (B).
Figure 4 Zero Gravity® and Cathpax® AIR.
A: Two hinged swing arm zero gravity systems installed in a hybrid room. This system consists of a single fixation point of the hinged swing arm. It can be used on both sides of the table if there is a fixation point available; B: A floor zero gravity unit. The suspended body and face shield can be repositioned for a broad range of procedures and room configurations; C, D: Photographs of the radiation protection cabin (Cathpax® AIR) in use during a coronary chronic total occlusion intervention.
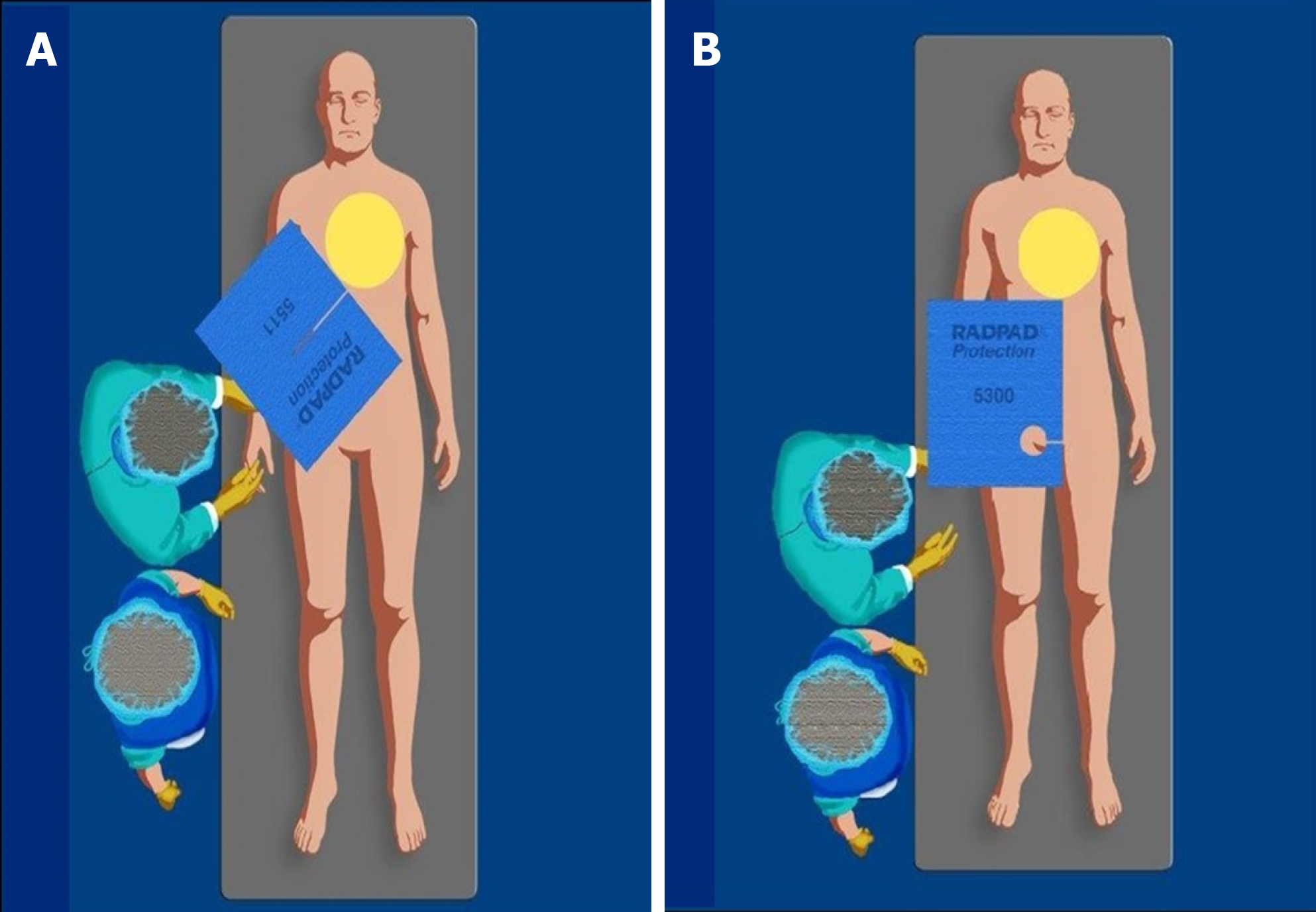
Figure 5 Correct positioning of the RadPad radioprotective drapes.
A-B: The radioprotective drapes should be placed on the patient, between the image intensifier and the operator during (A) femoral and (B) radial procedures.
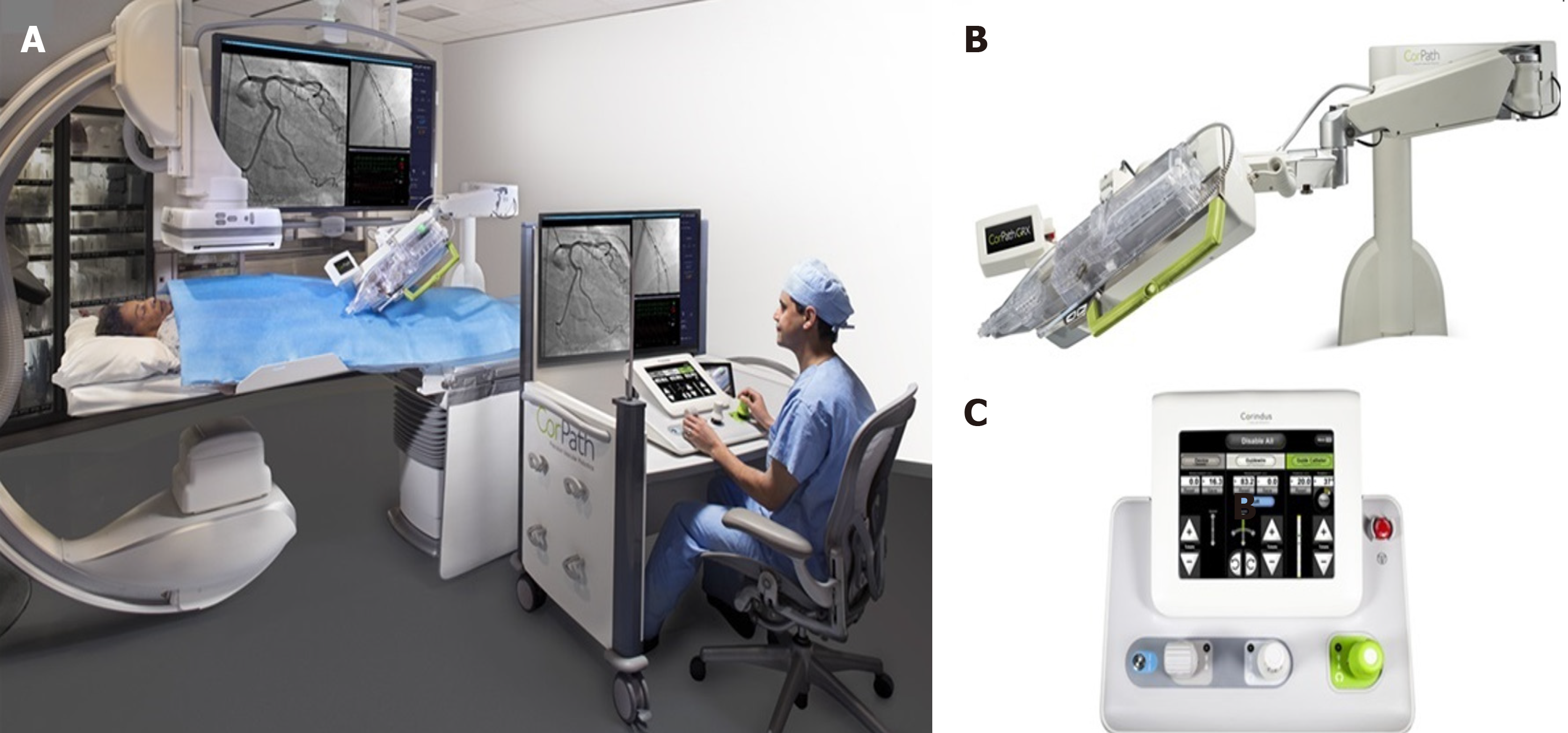
Figure 6 During robotic-assisted intervention, the interventional cardiologist sits in a radiation-shielded workstation and uses a set of joysticks and touchscreen controls that translate the physician’s movements into device control.
A: Control console; B: Extended-reach arm; C: CorPath cassette of the robotic system.
- Citation: Gutierrez-Barrios A, Cañadas-Pruaño D, Noval-Morillas I, Gheorghe L, Zayas-Rueda R, Calle-Perez G. Radiation protection for the interventional cardiologist: Practical approach and innovations. World J Cardiol 2022; 14(1): 1-12
- URL: https://www.wjgnet.com/1949-8462/full/v14/i1/1.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i1.1