Copyright
©The Author(s) 2019.
World J Cardiol. Dec 26, 2019; 11(12): 282-291
Published online Dec 26, 2019. doi: 10.4330/wjc.v11.i12.282
Published online Dec 26, 2019. doi: 10.4330/wjc.v11.i12.282
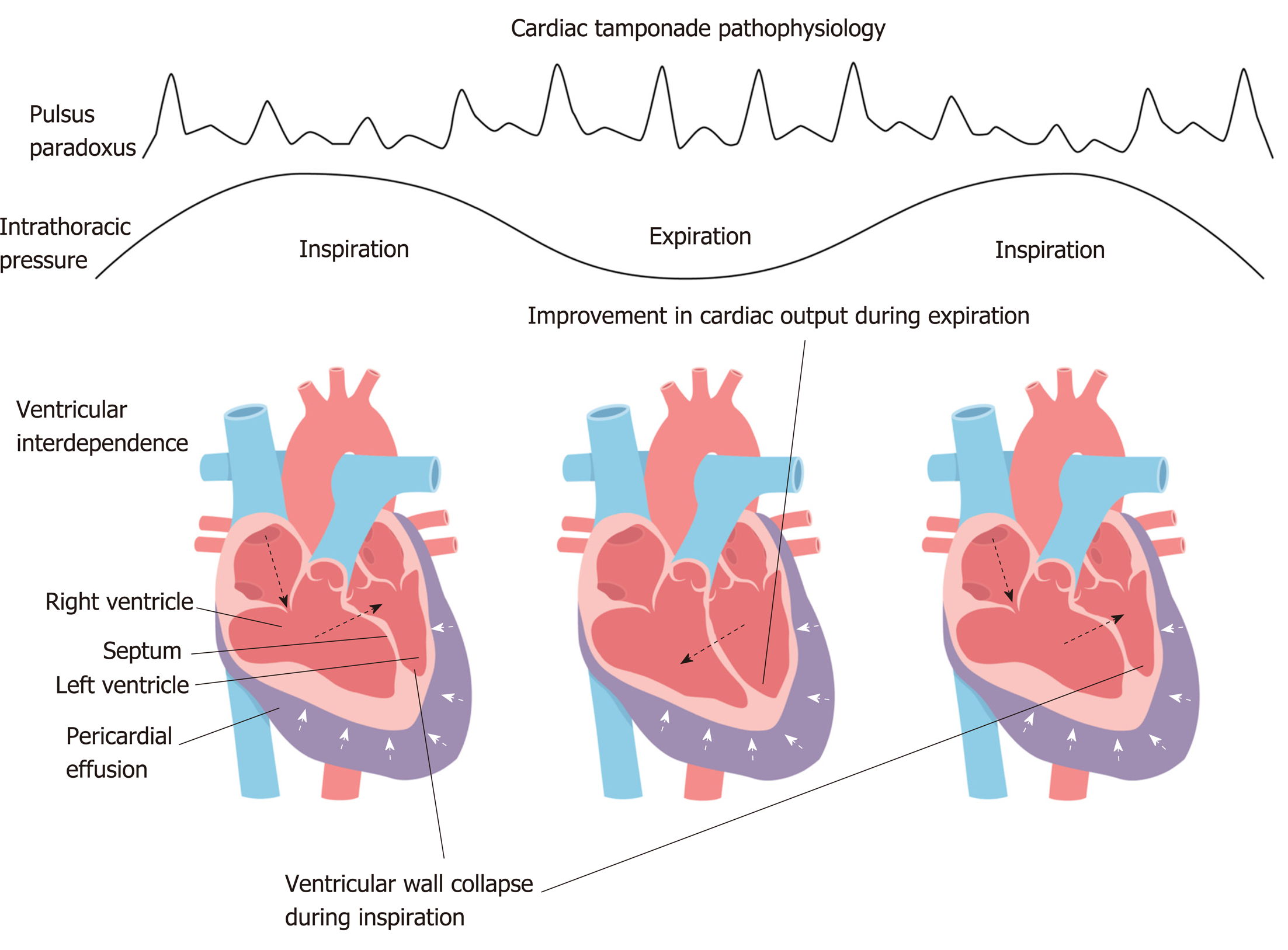
Figure 1 Cardiac tamponade physiology.
There is offset of the transmural pressure (intracardiac minus pericardial pressure) in cardiac tamponade. During inspiration, the right heart filling occurs at the expense of the left, so that its transmural pressure transiently improves and then reverts during expiration and this phenomenon is referred to as interventricular dependence.
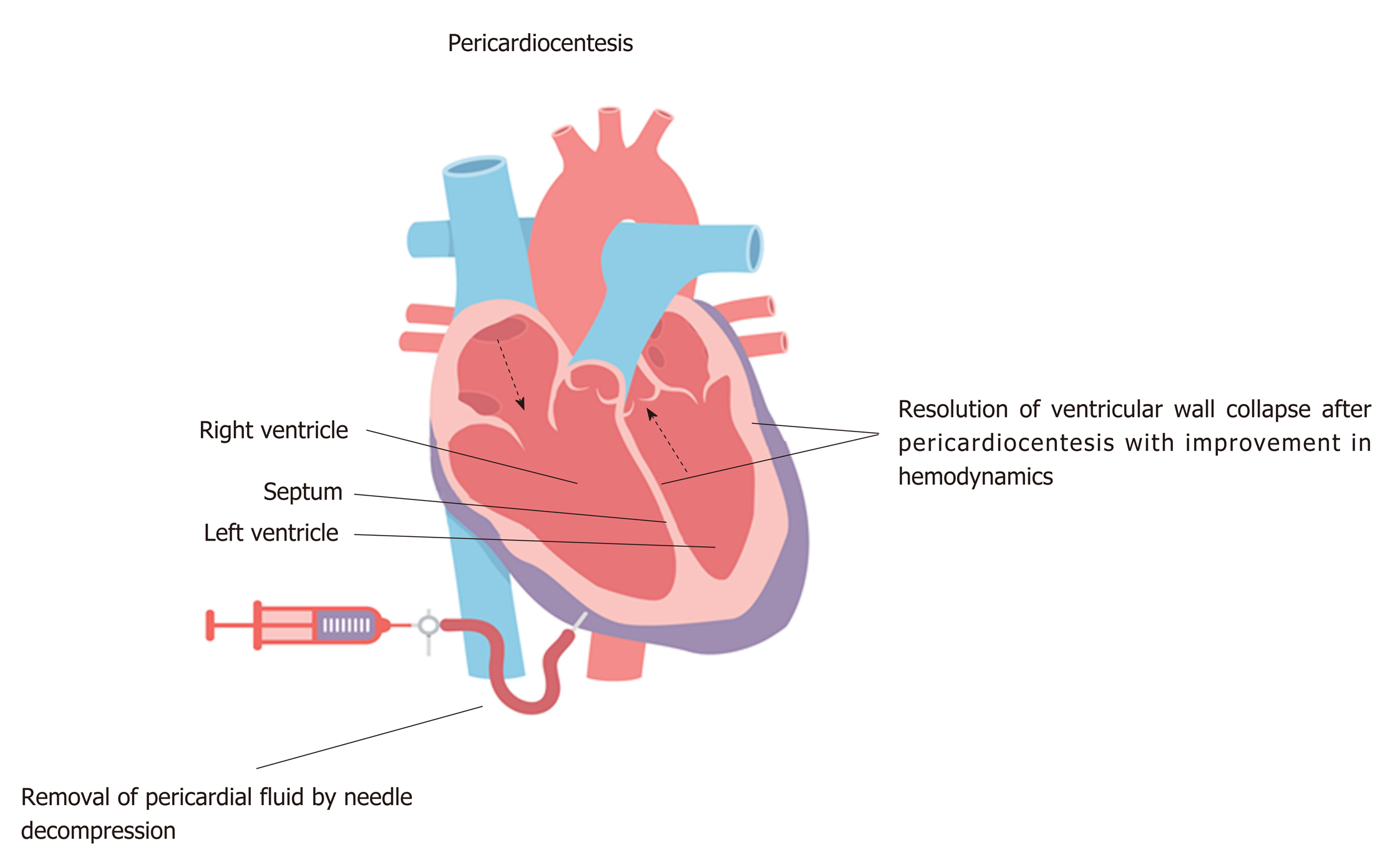
Figure 2 Pericardiocentesis.
Emergent needle decompression of the pericardial fluid with pericardiocentesis is often required in tamponade as it helps in restoration of a normal transmural pressure and thus ultimately restores normal hemodynamics. Interventricular dependence has resolved with pericardial decompression.
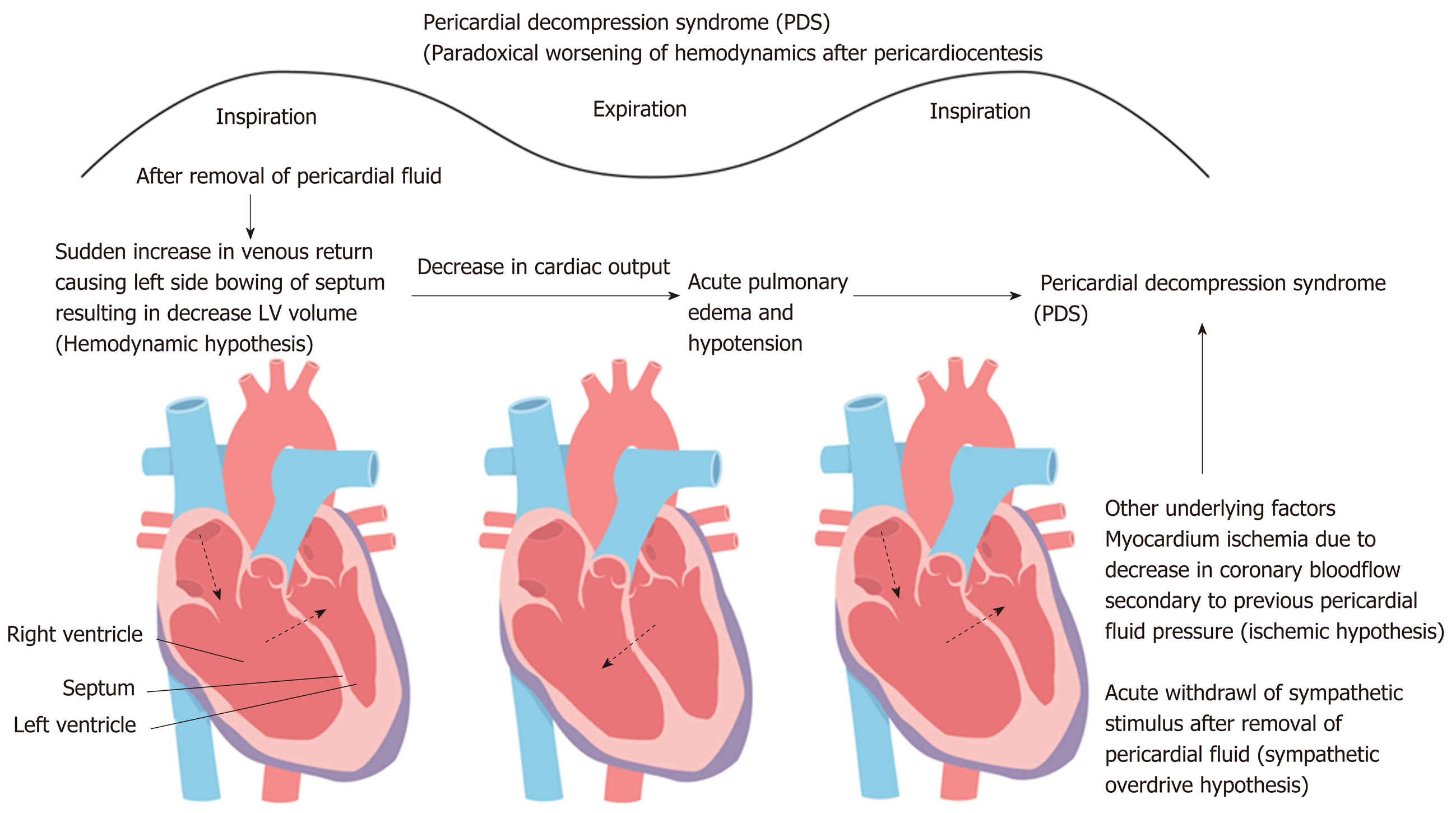
Figure 3 Pericardial decompression syndrome.
Following the rapid removal of the pericardial fluid originally compressing the right sided chambers during tamponade, may lead to an increased venous return causing significant right ventricular expansion at the expense of the left chamber resulting in the reduced left ventricle volume/output and thus ensuing decompensated left heart failure and/or pulmonary edema. The rapid tamponade release is also followed by a net increase in the pulmonary venous return (left ventricular preload) while adaptive systemic vascular resistance (after-load) being still high and may result in preload/afterload mismatch thus precipitating an acute onset heart failure.
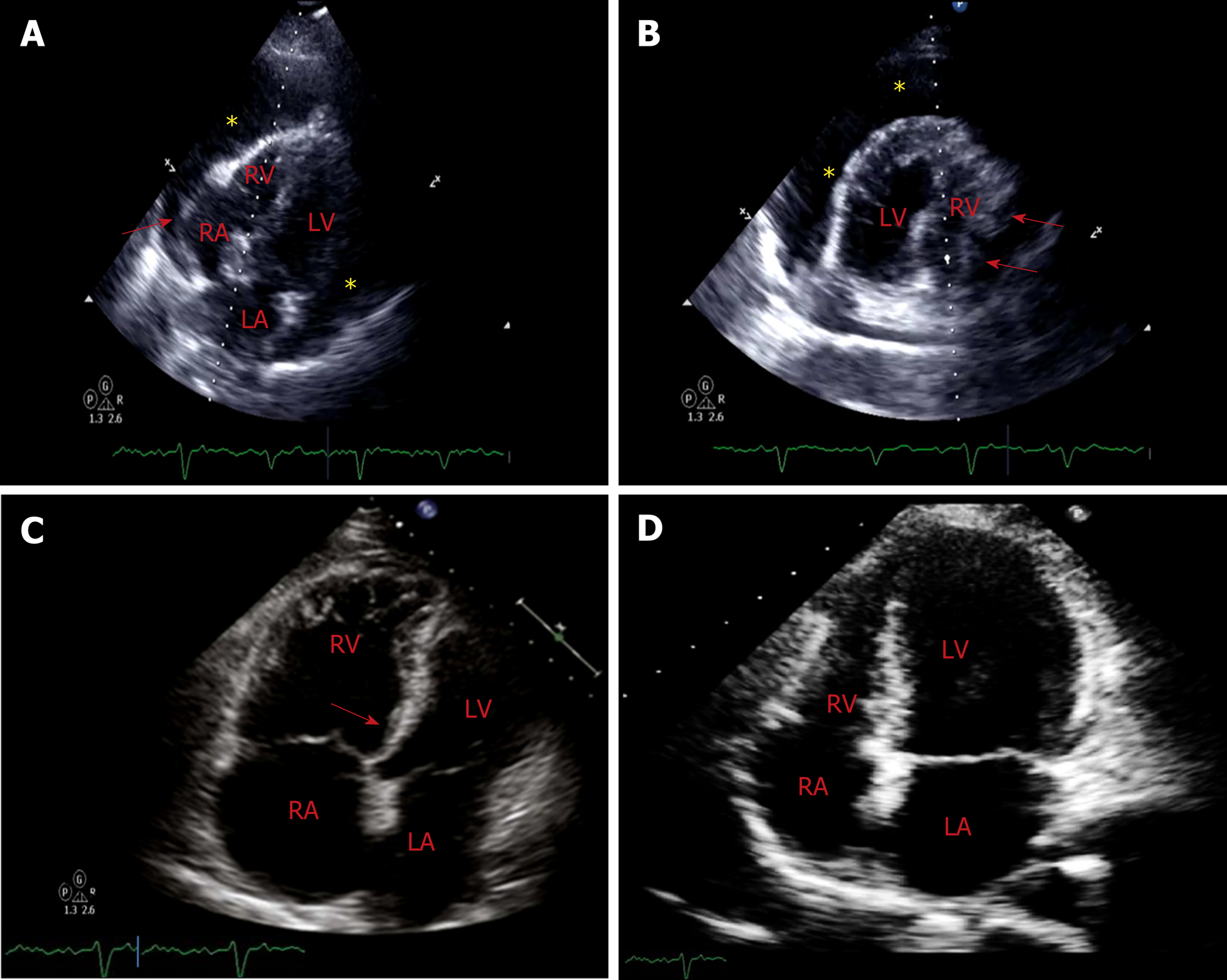
Figure 4 Computed tomography.
A: Off-axis 4-chamber view of transthoracic echocardiogram demonstrates a large circumferential pericardial effusion (marked by *) with evidence of end diastolic right chamber compression (marked by red arrow) and normal left ventricular ejection fraction. Swinging heart sign was also noted which is used to describe pendular swinging of the heart inside the pericardial space and is associated with a large pericardial effusion; B: 4-chamber view (mirror-view) demonstrates RA inversion, RV diastolic compression (marked by red arrows) and the swinging heart sign; C: Limited surface echocardiogram after pericardiocentesis demonstrated interval resolution of pericardial effusion and mild to moderately dilated right ventricle with mild RV hypokinesis and septal shift towards the left ventricle(as marked by red arrow). Patient demonstrated paradoxical worsening of blood pressure. Rapid pericardial fluid decompression may have resulted in paradoxical worsening of hemodynamics likely secondary to a combination of two factors: the first being a sudden increase in the venous return with still relatively higher systemic vascular resistance posing to a preload-afterload mismatch (hemodynamic hypothesis) and secondly likely being focal RV hypokinesis, predisposed by an increased sympathetic tone; D: A repeat echocardiogram on day 5 demonstrated normalized ventricular function. RV: Right ventricular; LV: Left ventricular; RA: Right atrial; LA: Left atrial.
- Citation: Prabhakar Y, Goyal A, Khalid N, Sharma N, Nayyar R, Spodick DH, Chhabra L. Pericardial decompression syndrome: A comprehensive review. World J Cardiol 2019; 11(12): 282-291
- URL: https://www.wjgnet.com/1949-8462/full/v11/i12/282.htm
- DOI: https://dx.doi.org/10.4330/wjc.v11.i12.282