Published online Aug 27, 2017. doi: 10.4240/wjgs.v9.i8.182
Peer-review started: November 29, 2016
First decision: February 20, 2017
Revised: March 20, 2017
Accepted: April 23, 2017
Article in press: April 24, 2017
Published online: August 27, 2017
Processing time: 268 Days and 16.3 Hours
A 62-year-old man who had acute rectal obstruction due to a large rectal cancer is presented. He underwent emergency laparoscopic colostomy. We used the laparoscopic puncture needle to inject analgesia with the novel transperitoneal approach. In this procedure, both ultrasound and laparoscopic images assisted with the accurate injection of analgesic to the correct layer. The combination of laparoscopic visualization and ultrasound imaging ensured infiltration of analgesic into the correct layer without causing damage to the bowel. Twenty-four hours postoperatively, the patient’s pain intensity as assessed by the numeric rating scale was 0-1 during coughing, and a continuous intravenous analgesic was not needed. Colostomy is often necessary in colon obstruction. Epidural anesthesia for postoperative pain cannot be used in patients with a coagulation disorder. We report the use of a novel laparoscopic rectus sheath block for colostomy. There has been no literature described about the nerve block with transperitoneal approach. The laparoscopic rectus sheath block was performed safely and had enough analgesic efficacy for postoperative pain. This technique could be considered as an optional anesthetic regimen in acute situations.
Core tip: This report demonstrated that transperitoneal rectal sheath block can be performed safely in achieving analgesia in patients undergoing laparoscopic colostomy. This transperitoneal rectal sheath block technique has the potential to become an additional postoperative regimen for various forms of laparoscopic abdominal surgery.
- Citation: Nagata J, Watanabe J, Sawatsubashi Y, Akiyama M, Arase K, Minagawa N, Torigoe T, Hamada K, Nakayama Y, Hirata K. Novel technique of abdominal wall nerve block for laparoscopic colostomy: Rectus sheath block with transperitoneal approach. World J Gastrointest Surg 2017; 9(8): 182-185
- URL: https://www.wjgnet.com/1948-9366/full/v9/i8/182.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v9.i8.182
Colostomy is often necessary in acute colon obstruction. The indications for laparoscopic colostomy for large bowel obstruction caused by benign colorectal disease have been described previously[1]. The laparoscopic approach is associated with a significant reduction in postoperative pain, faster recovery, and shorter hospital day compared with open surgery[2]. However, there is still considerable postoperative pain associated with the laparoscopic procedure as a result of the transabdominal sutures, even in the small incisions.
Strategies for analgesia after laparoscopic colostomy are based on the concepts for the open procedure; epidural analgesia is the standard technique. However, epidural use is sometimes limited because of perioperative anticoagulant therapy and the potential for undesirable complications such as epidural hematomas and infections. Therefore, recently published guidelines from the United Kingdom no longer recommend epidural analgesia as standard pain management after laparoscopic colorectal surgery[3]. Furthermore, patients with acute colorectal obstruction often have a coagulation disorder and higher risks. For patients with obstruction, especially in emergency cases, regional anesthetic techniques such as the ultrasound-guided rectus sheath (RS) block have become increasingly popular as methods to provide analgesia for laparoscopic surgery. The RS block has gained popularity owing to a relatively high success rate[4]. However, even the RS block has potential complications such as RS hematoma if the vessels are damaged, and it is possible to puncture the posterior RS, peritoneum, and/or bowel. In this report, we describe a novel laparoscopic transperitoneal approach and assess its efficacy. This is the first report of laparoscopic colostomy using the transperitoneal approach for the RS block.
After approval by the Research Ethics Board of our institution and the patient’s informed consent. A 62-year-old man with acute rectal obstruction due to a large rectal cancer underwent laparoscopic colostomy. The procedure was performed as an emergency operation, with the patient placed under general anesthesia with 8% sevoflurane via a face mask. Epidural anesthesia was not performed, as the patient had a coagulation disorder.
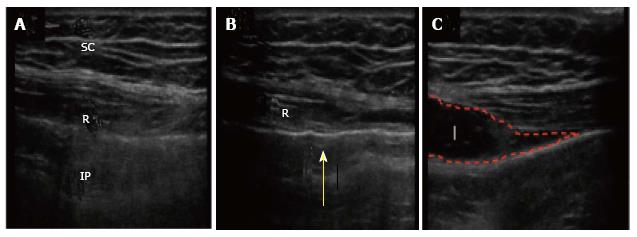
Laparoscopic colostomy was conducted via two incisions; the first incision was made via the stoma site (25 mm), and a second navel incision (5 mm) was made. After making the skin incisions, pneumoperitoneum was created with the pressure standardized to 10 mmHg. Intraoperatively, under laparoscopic visualization, a bilateral transperitoneal RS block was performed with ultrasound guidance to reduce unexpected abdominal wall pain. Ultrasound was performed with a linear array probe, 13-6 MHz, SonoSite M-Turbo™ (SonoSite Inc., Bothell, WA, United States). The probe was placed longitudinally on the patient’s abdominal wall while the tip of a Peti-needle™ (Hakko Co., Ltd., Adachi-ku, Tokyo, Japan) was inserted through the peritoneum under laparoscopic visualization. A Peti-needle™ was inserted through the 5-mm port at the stoma site, and 20 mL of 0.25% levobupivacaine was injected though the peritoneum (Figure 1): Posterior to the rectus muscle and above the underlying RS block. Infiltration into the correct layer without leakage was checked by both laparoscopic visualization and ultrasound (Figure 2). The technique was repeated on the other site. Surgery was completed successfully and the anesthetic procedure did not affect the operation.
Postoperatively, the patient was brought to the post-anesthesia care unit for continuous monitoring of vital signs. Nurses administered intravenous analgesic as needed. Pain severity was assessed at rest and during coughing using a numeric rating scale (NRS), where no pain = 0, and the worst pain = 10. Three hours postoperatively, the patient’s pain intensity as assessed by the NRS was 3 at rest and 4 during coughing. Twenty-four hours postoperatively, the patient’s NRS pain intensity was 0-1 during coughing, and an intravenous analgesic was no longer needed. There were no other postoperative problems such as hematoma or severe infection in the muscle.
The RS block is a regional anesthetic procedure that was first reported in 1899[5]. It has been used in the treatment of pediatric chronic abdominal wall pain[6]. Any regional technique carries a risk of introducing infection, causing bleeding, or damaging local structures[7]. Proposed benefits of these regional blocks include the avoidance of neuroaxial techniques such as epidural analgesia and their associated risks, as well as a reported reduction in opioid consumption[8-10].
Laparoscopic-assisted transversus abdominis plane block has been performed for ventral hernia repair[11] and cholecystectomy[12]; however, this procedure was done only with ultrasound guidance, and the needle was inserted transcutaneously. Using the transperitoneal approach via laparoscopy and ultrasound guidance, the RS block has been demonstrated to be simpler and safer.
RS block via the transperitoneal approach in laparoscopic colostomy provided effective and safe postoperative analgesia in a patient with acute colon obstruction. When compared with the open procedure, laparoscopic colostomy itself carries several advantages including early postoperative recovery, less postoperative pain, and rapid restoration of bowel function[13]. A laparoscopic RS block can be performed by the operating surgeon without perforation of the bowel. This procedure could be performed in high-risk patients who have a coagulation disorder, and also in highly obese patients. Currently, there are no published trials examining the role of the laparoscopically performed RS block via the transperitoneal approach for the management of perioperative pain in laparoscopic abdominal surgery. In the present case, the procedure was performed safely and the transperitoneal RS block provided the effective analgesia in abdominal surgery.
Although the RS block, known as a compartment block, is thought to require a large amount of local anesthetic to provide an analgesic effect, our result showed that it was possible to produce sufficient analgesia with a small dosage of local anesthetic with ultrasonic and laparoscopic visualization. The RS block has no hemodynamic effects, and is ideal for patients with hypotension related to sepsis or hypovolemia. Unlike epidurals and continuous intravenous analgesia, the RS block does not require connection to pumps and stands, thereby enabling early patient mobilization. Our novel analgesia technique has potential use as a regimen for postoperative pain of various laparoscopic surgeries. This study had a limitation; the Peti-needle™ costs twice as much as the needle used for the percutaneous approach. Additional prospective studies are required to evaluate the benefits of laparoscopic transperitoneal RS block in other techniques such as local anesthetic wound infiltration, patient-controlled intravenous opioid administration, and the percutaneous approach.
The authors thank Dr. Reiko Horishita and Dr. Kentaro Kida for their technical assistance. And all the authors declare that there are no conflict of interest.
A 62-year-old man who had huge rectal cancer underwent laparoscopic colostomy and a novel nerve block with transperitoneal injection of analgesia.
A huge rectal tumor of his pelvic space occurred acute colon obstruction.
Gastrointestinal tumor, neuroendocrine tumor.
Only carcino-embryonic antigen was arized, other labs were within normal limits.
A huge rectal tumor of his pelvic space occurred acute colon obstruction.
Moderately differentiated adenocarcinoma.
This is a case report that is describing a novel rectus sheath block technique for laparoscopic colostomy in an adult. However, the authors would like to point out the following. Generally, the manuscript is good written.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Tang ST, Uygun I S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Panis Y. [Laparoscopic surgery for benign colorectal diseases]. J Chir (Paris). 2000;137:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Joshi GP, Bonnet F, Kehlet H. Evidence-based postoperative pain management after laparoscopic colorectal surgery. Colorectal Dis. 2012;15:146-155. [RCA] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (1)] |
| 3. | Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, Macfie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O; Enhanced Recovery After Surgery (ERAS) Society, for Perioperative Care; European Society for Clinical Nutrition and Metabolism (ESPEN); International Association for Surgical Metabolism and Nutrition (IASMEN). Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37:259-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 850] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 4. | Sites BD, Brull R. Ultrasound guidance in peripheral regional anesthesia: philosophy, evidence-based medicine, and techniques. Curr Opin Anaesthesiol. 2006;19:630-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Schleich DL. Schmerzlose operation. Berlin: Springer Verlag 1899; 240-258. |
| 6. | Skinner AV, Lauder GR. Rectus sheath block: successful use in the chronic pain management of pediatric abdominal wall pain. Paediatr Anaesth. 2007;17:1203-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Lancaster P, Chadwick M. Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;104:509-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 118] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis. 2012;14:e635-e642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 181] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 9. | Gupta M, Naithani U, Singariya G, Gupta S. Comparison of 0.25% Ropivacaine for Intraperitoneal Instillation v/s Rectus Sheath Block for Postoperative Pain Relief Following Laparoscopic Cholecystectomy: A Prospective Study. J Clin Diagn Res. 2016;10:UC10-UC15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Uchinami Y, Sakuraya F, Tanaka N, Hoshino K, Mikami E, Ishikawa T, Fujii H, Ishikawa T, Morimoto Y. Comparison of the analgesic efficacy of ultrasound-guided rectus sheath block and local anesthetic infiltration for laparoscopic percutaneous extraperitoneal closure in children. Paediatr Anaesth. 2017;27:516-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Fields AC, Gonzalez DO, Chin EH, Nguyen SQ, Zhang LP, Divino CM. Laparoscopic-Assisted Transversus Abdominis Plane Block for Postoperative Pain Control in Laparoscopic Ventral Hernia Repair: A Randomized Controlled Trial. J Am Coll Surg. 2015;221:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Elamin G, Waters PS, Hamid H, O’Keeffe HM, Waldron RM, Duggan M, Khan W, Barry MK, Khan IZ. Efficacy of a Laparoscopically Delivered Transversus Abdominis Plane Block Technique during Elective Laparoscopic Cholecystectomy: A Prospective, Double-Blind Randomized Trial. J Am Coll Surg. 2015;221:335-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Shah A, Moftah M, Al-Furaji HN, Cahill RA. Standardized technique for single port laparoscopic ileostomy and colostomy. Colorectal Dis. 2014;16:248-252. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |