Published online Dec 27, 2017. doi: 10.4240/wjgs.v9.i12.288
Peer-review started: August 27, 2017
First decision: September 25, 2017
Revised: October 20, 2017
Accepted: November 11, 2017
Article in press: November 11, 2017
Published online: December 27, 2017
Processing time: 122 Days and 4.9 Hours
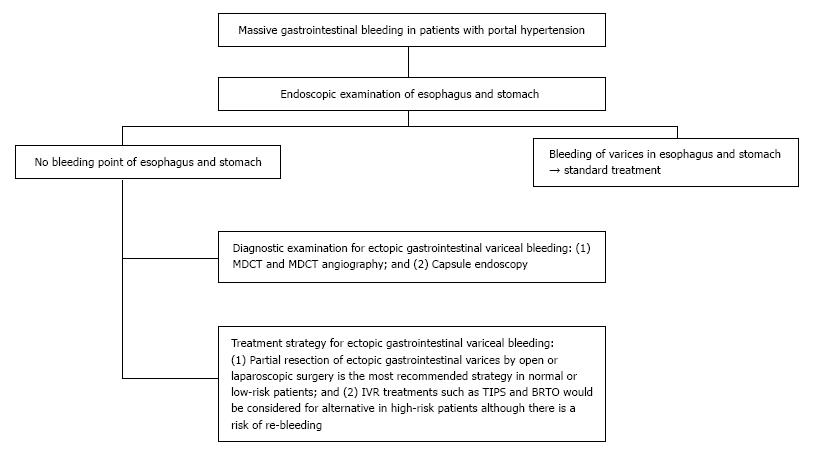
Massive gastrointestinal bleeding from gastrointestinal varices is one of the most serious complications in patients with portal hypertension. However, if no bleeding point can be detected by endoscopy in the predilection sites of gastrointestinal varices, such as the esophagus and stomach, ectopic gastrointestinal variceal bleeding should be considered as a differential diagnosis. Herein, we report a case of ectopic ileal variceal bleeding in a 57-year-old woman, which was successfully diagnosed by multi-detector row CT (MDCT) and angiography and treated by segmental ileum resection. To date, there have been no consensus for the treatment of ectopic ileal variceal bleeding. This review was designed to clarify the clinical characteristics of patients with ectopic ileal variceal and discuss possible treatment strategies. From the PubMed database and our own database, we reviewed 21 consecutive cases of ileal variceal bleeding diagnosed from 1982 to 2017. MDCT and angiography is useful for the rapid examination and surgical resection of an affected lesion and is a safe and effective treatment strategy to avoid further bleeding.
Core tip: Massive gastrointestinal bleeding from gastrointestinal varices is one of the most serious complications in patients with portal hypertension. If no bleeding point can be detected by endoscopy in the predilection sites of gastrointestinal varices, ectopic gastrointestinal variceal bleeding should be considered as a differential diagnosis. We report here a 57-year-old female case of ectopic ileal variceal bleeding, which were diagnosed by multi-detector row CT (MDCT) and its angiography and treated by segmental ileum resection. From the review results of previous reports, MDCT and its angiography is a rapid and useful examination. Moreover, surgical resection of responsible lesion is safe and effective treatment strategy to avoid further bleeding.
- Citation: Minowa K, Komatsu S, Takashina K, Tanaka S, Kumano T, Imura K, Shimomura K, Ikeda J, Taniguchi F, Ueshima Y, Lee T, Ikeda E, Otsuji E, Shioaki Y. Ectopic gastrointestinal variceal bleeding with portal hypertension. World J Gastrointest Surg 2017; 9(12): 288-292
- URL: https://www.wjgnet.com/1948-9366/full/v9/i12/288.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v9.i12.288
Massive gastrointestinal bleeding from a gastrointestinal varix is one of the most serious complications in patients with portal hypertension. However, if the point of continuous bleeding in the predilection sites of a gastrointestinal varix, such as the esophagus and stomach, is not found and no further strategy for the accurate diagnosis and effective treatment of the bleeding point exists, the condition may become life threatening.
Lebrec et al[1] classified the gastrointestinal varices other than those of the esophagus and stomach as ectopic varices. Ectopic gastrointestinal varices were reported in the sites of the duodenum, small intestine, colon, rectum, peristomal, biliary, peritoneal, umbilical, and other locations. Ectopic gastrointestinal varices cause an unusual hemorrhage and account for 5% of all variceal bleeding. In particular, ectopic ileal variceal bleeding is the major type of ectopic gastrointestinal variceal bleeding[2]. Herein, we report a case of ectopic ileal variceal bleeding, which was diagnosed by MDCT and angiography and was surgically treated. Moreover, we reviewed previous case reports regarding the clinical behaviors, diagnosis, and treatment strategies of ectopic ileal variceal bleeding, including our cases diagnosed between 1982 and 2017 from the PubMed database.
A 57-year-old Asian woman with autoimmune portal hypertension due to polymyositis was admitted to our hospital with a 2-d history of hematochezia. She had a history of esophageal variceal rupture, which had been treated by endoscopy 3 years before. At admission, she had a blood pressure of 92/58 mmHg, heart rate of 85/min, respiratory rate of 16/min, and body temperature of 35.2 °C. Although she was pale and showed conjunctival pallor, and there was no jaundice, abdominal pain, or shifting dullness. Laboratory data were as follows: hemoglobin 7.3 g/dL, hematocrit 23.4%, platelets 112000/mm3, prothrombin time 98%, serum albumin 3.5 g/dL, total bilirubin 1.1 mg/dL, aspartate aminotransferase/alanine aminotransferase 35/51 IU/L. Hepatitis B surface antigen was positive and hepatitis C virus antibody was negative. There was no encephalopathy. Her Child-Pugh score was 6 (class A).
We performed an emergent upper gastrointestinal endoscopy, which showed a mild esophageal varix without bleeding. However, lower gastrointestinal endoscopy revealed a large blood clot at the ileocecum, but there was no active bleeding lesion during the endoscopy. MDCT showed no definitive liver cirrhosis, but dilation of the hepatic portal vein and umbilical vein and splenomegaly and portosystemic collaterals indicated portal hypertension. In addition, enhanced MDCT and MDCT and angiography revealed the presence of an ileal varix, which showed no active bleeding into the abdominal cavity. In particular, the ileal varix had a portosystemic shunt via the superior mesenteric vein into the right ovarian vein.
She was treated conservatively for 2 d with a blood transfusion. On the 3rd day after admission, she had massive hematochezia. We performed a second MDCT and angiography and diagnosed the patient as hematochezia due to massive ileal varix bleeding because there was a massive coagula at the distal ileal lumen of the ileal varix. We performed emergent segmental ileal resection, which included the ileal varix, via a small laparotomy (Figure 1). The varix was located at the 20-cm proximal portion of the ileocecal valve. Her postoperative condition was uneventful. She had no further bleeding and was discharged on the 8th day after surgery.
Portal hypertensive enteropathy is present in 5%-11% of patients with portal hypertension and often gives rise to gastrointestinal varices in the esophagus and stomach, which cause active bleeding[3]. Gastrointestinal varices other than those of the esophagogastric area are rare and are classified as ectopic gastrointestinal varices. Ectopic gastrointestinal varices occur at sites such as the duodenum, small intestine, colon, rectum, peristomal, biliary, peritoneal, umbilical, and other locations. Various related factors of an ectopic gastrointestinal varix such as portal hypertension due to cirrhosis, portal vein thrombosis, a history of abdominal surgery, chronic intraperitoneal inflammation, and hematochezia have been reported[4,5].
An ileal varix is the major type of ectopic gastrointestinal varix. In a review 169 cases of ectopic gastrointestinal variceal bleeding, 17% was the highest rate of bleeding among all sites and was derived from jejunal and ileal varices[2]. Ileal varices are associated with a history of abdominal surgery and adhesions[6]. Presumably, abdominal surgery and intraperitoneal inflammation may cause adhesion of the intestinal tract. Then, collateral vessels within the adhesion may give rise to ectopic intestinal varices, particularly, in the jejunum and ileum[7]. Ectopic ileal varices most commonly flow into systemic circulation through the gonadal veins and less commonly through branches of the internal iliac veins[7]. In our case, there were various compatible features such as autoimmune portal hypertension and previous surgeries for appendicitis and hematochezia. Moreover, a portosystemic shunt, which flowed from the superior mesenteric vein into the right ovarian vein, was detected.
From the PubMed database including our own, we reviewed 21 consecutive cases of ileal variceal bleeding diagnosed from 1982 to 2017. The clinical features of 21 patients are shown in Table 1. Patients with ileal variceal bleeding consisted of 5 male and 16 female patients with a median age of 57 years (range 33-80 years). From the medical history, 71.4% (15/21) of patients were associated with portal hypertension due to liver cirrhosis. Previous abdominal surgery was noted in 57.1% (12/21) of patients. Regarding the diagnosis, 61.9% (13/21) of patients were diagnosed by SMA angiography. Capsule endoscopy was used in two cases. However, recent cases were mainly diagnosed by MDCT or MDCT and angiography and treated by surgical resection with no further bleeding. Surgical resection was performed in 76.1% (16/21) of all patients. Some recent patients underwent interventional radiology (IVR) treatment methods such as transjugular intrahepatic portosystemic shunt (TIPS)[8-10] and balloon-occluded retrograde transvenous obliteration (BRTO)[11,12].
| Case | Year | Age | Sex | Past history | Previous abdominal surgery | Diagnosis | Treatment | Outcome | |
| 1 | 1982 | Falchuk | 52 | F | liver cirrhosis | Cholecystectomy | SMA angiography | Partial enterectomy | Dead |
| 2 | 1984 | Shimada | 49 | M | liver cirrhosis | Ruputured esophageal varix | SMA angiography | Partial enterectomy | Alive |
| 3 | 1986 | Hojhus | 80 | F | Periappendicular abscess | (-) | SMA angiography | Partial enterectomy | Dead |
| 4 | 1986 | Arst | 56 | F | Liver cirrhosis | (-) | Laparotomy | Ileocolectomy | Dead |
| 5 | 1990 | Lewis | 72 | F | Liver cirrhosis | Hysterectomy | SMA angiography | Ileocolectomy | Alive |
| 6 | 1994 | Kurihara | 43 | M | (-) | (-) | SMA angiography | Partial enterectomy | Alive |
| 7 | 1997 | Ahn | 54 | M | Liver cirrhosis | (-) | SMA angiography | ileocolEctomy | Dead |
| 8 | 1999 | Ohtani | 66 | F | Liver cirrhosis | Ectopic pregnancy | SMA angiography | Partial enterectomy | Alive |
| 9 | 2001 | Kobayashi | 62 | F | Hepatocellular carcinoma | Hysterectomy | SMA angiography | Ligation of ileocecal and ovarian vein | Alive |
| 10 | 2006 | Ueda | 72 | F | Liver cirrhosis | Abdominal aortic aneurysm | MDCT | Partial enterectomy | Alive |
| 11 | 2007 | Lopez | 56 | F | Liver cirrhosis | Pelvic surgery | SMA angiography | TIPS | Alive |
| 12 | 2007 | Mashimo | 33 | F | Liver cirrhosis | Endometriosis | SMA angiography | Partial enterectomy | Alive |
| 13 | 2009 | Suzuki | 74 | F | Liver cirrhosis | Acute appendicitis | MDCT | Partial enterectomy | Alive |
| 14 | 2009 | Traina | 58 | F | Liver cirrhosis | (-) | ES | Sclerotherapy + TIPS | Alive |
| 15 | 2009 | Sato | 55 | M | Liver cirrhosis | Laparotomy for colonic tumor | Retrograde transvenous venography | BRTO | Alive |
| 16 | 2010 | Konishi | 54 | F | (-) | (-) | CE | Partial enterectomy | Alive |
| 17 | 2011 | Ambiru | 62 | F | Liver cirrhosis | Ectopic pregnancy | MDCT | Partial enterectomy | Alive |
| 18 | 2011 | Castagna | 70 | M | Liver cirrhosis | (-) | CE | TIPS | Alive |
| 19 | 2013 | Vamadevan | 48 | F | Liver cirrhosis | (-) | MDCT | TIPS | Alive |
| 20 | 2015 | Garcia | 74 | F | Venous thromboembolism | (-) | MDCT | Partial enterectomy | Alive |
| 21 | 2017 | Our case | 57 | F | Portal hypertension | Acute appendicitis | MDCT | Partial enterectomy | Alive |
There were no patients with re-bleeding in previous reports of ileal variceal bleeding. However, re-bleeding rates of 23%-39% have been reported in TIPS and 5%-16.6% in BRTO in all reports of ectopic gastrointestinal variceal bleeding[13-16]. Although non-invasive treatment such as IVR may be desirable for ectopic gastrointestinal variceal bleeding in high-risk patients with co-morbidities, surgical resection of an affected intestine is currently a safe and effective treatment strategy to avoid further re-bleeding. Moreover, laparoscopic surgical resection of an affected intestine could be possible effective strategy as a minimally invasive procedure (Figure 2).
Ectopic gastrointestinal varices bleeding, especially ileal variceal bleeding, in patients with portal hypertension might be considered as a differential diagnosis if upper or lower endoscopy cannot detect a bleeding point such as in the esophagus or stomach. MDCT or MDCT angiography is useful for the rapid examination and surgical resection of an affected ileum and is a safe and effective treatment strategy to avoid further bleeding.
A 57-year-old Asian woman with autoimmune portal hypertension due to polymyositis was admitted to our hospital with a 2-d history of hematochezia. She had a history of esophageal variceal rupture, which had been treated by endoscopy 3 years before.
On the 3rd day after admission, she had massive hematochezia. The authors performed a second multi-detector row CT (MDCT) and angiography and diagnosed as massive ileal varix bleeding because there was a massive coagula at the distal ileal lumen of the ileal varix.
There was no differential diagnosis because upper and lower endoscopic examinations could not detect the responsible lesion.
Laboratory diagnosis was a severe anemia with hemoglobin 7.3 g/dL and hematocrit 23.4% because other data showed no apparent disorder.
Imaging diagnosis by MDCT and its angiography was massive ileal varix bleeding because there was a massive coagula at the distal ileal lumen of the ileal varix.
Pathological diagnosis was the leal varix.
The authors performed emergent segmental ileal resection, which included the ileal varix, via a small laparotomy. The varix was located at the 20-cm proximal portion of the ileocecal valve.
Jejunal varices as a cause of massive gastrointestinal bleeding. Am J Gastroenterol 1992; 87: 514-517.
The authors used common terms, which were used in previous reports.
Ectopic gastrointestinal variceal bleeding might be considered as a differential diagnosis if upper or lower endoscopy could not detect bleeding point. From the review results of previous reports including our case, MDCT and its angiography is a rapid and useful examination. Moreover, surgical resection of responsible lesion is safe and effective treatment strategy to avoid further bleeding.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Boukerrouche A, Dinc B, Hoyuela C, Katuchova J, Tomazic A S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Lebrec D, Benhamou JP. Ectopic varices in portal hypertension. Clin Gastroenterol. 1985;14:105-121. [PubMed] |
| 2. | Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. 1998;28:1154-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 253] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 3. | De Palma GD, Rega M, Masone S, Persico F, Siciliano S, Patrone F, Matantuono L, Persico G. Mucosal abnormalities of the small bowel in patients with cirrhosis and portal hypertension: a capsule endoscopy study. Gastrointest Endosc. 2005;62:529-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 133] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Yuki N, Kubo M, Noro Y, Kasahara A, Hayashi N, Fusamoto H, Ito T, Kamada T. Jejunal varices as a cause of massive gastrointestinal bleeding. Am J Gastroenterol. 1992;87:514-517. [PubMed] |
| 5. | Joo YE, Kim HS, Choi SK, Rew JS, Kim HR, Kim SJ. Massive gastrointestinal bleeding from jejunal varices. J Gastroenterol. 2000;35:775-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Kotfila R, Trudeau W. Extraesophageal varices. Dig Dis. 1998;16:232-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Akhter NM, Haskal ZJ. Diagnosis and management of ectopic varices. Ganstrointestinal Intervention. 2012;1:3-10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 8. | Castagna E, Cardellicchio A, Pulitanò R, Manca A, Fenoglio L. Bleeding ileal varices: a rare cause of chronic anemia in liver cirrhosis. Intern Emerg Med. 2011;6:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | López-Benítez R, Seidensticker P, Richter GM, Stampfl U, Hallscheidt P. [Case report: massive lower intestinal bleeding from ileal varices: treatment with transjugular intrahepatic portosystemic shunt (TIPSS)]. Radiologe. 2007;47:407-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Vamadevan S, Haltmeier T, Groebli Y. Portosystemic shunt via the superior mesenteric and right ovarian vein leading to small intestine bleeding in alcoholic liver cirrhosis. BMJ Case Rep. 2013;2013:pii: bcr2013008959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Akaike J. Ileal Varices Treated with Balloon-Occluded Retrograde Transvenous Obliteration. Gastroenterology Res. 2009;2:122-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Konishi H, Kikuchi S, Miyashita A, Ichikawa D, Fujiwara H, Kubota T, Ochiai T, Kokuba Y, Yasukawa S, Yanagisawa A. Minimally invasive surgery for obscure idiopathic ileal varices diagnosed by capsule endoscopy and double balloon endoscopy: report of a case. Surg Today. 2010;40:1088-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Vidal V, Joly L, Perreault P, Bouchard L, Lafortune M, Pomier-Layrargues G. Usefulness of transjugular intrahepatic portosystemic shunt in the management of bleeding ectopic varices in cirrhotic patients. Cardiovasc Intervent Radiol. 2006;29:216-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Vangeli M, Patch D, Terreni N, Tibballs J, Watkinson A, Davies N, Burroughs AK. Bleeding ectopic varices--treatment with transjugular intrahepatic porto-systemic shunt (TIPS) and embolisation. J Hepatol. 2004;41:560-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 148] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 15. | Hashimoto N, Akahoshi T, Yoshida D, Kinjo N, Konishi K, Uehara H, Nagao Y, Kawanaka H, Tomikawa M, Maehara Y. The efficacy of balloon-occluded retrograde transvenous obliteration on small intestinal variceal bleeding. Surgery. 2010;148:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Saad WE, Wagner CC, Lippert A, Al-Osaimi A, Davies MG, Matsumoto AH, Angle JF, Caldwell S. Protective value of TIPS against the development of hydrothorax/ascites and upper gastrointestinal bleeding after balloon-occluded retrograde transvenous obliteration (BRTO). Am J Gastroenterol. 2013;108:1612-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |