Published online Sep 27, 2016. doi: 10.4240/wjgs.v8.i9.651
Peer-review started: April 26, 2016
First decision: June 16, 2016
Revised: July 8, 2016
Accepted: July 20, 2016
Article in press: July 22, 2016
Published online: September 27, 2016
Processing time: 152 Days and 21.5 Hours
To review clinical experience with barium appendicitis at a single institution.
A retrospective review of patients admitted with a diagnosis of acute appendicitis, from January 1, 2013 to December 31, 2015 was performed. Age, gender, computed tomography (CT) scan findings if available, past history of barium studies, pathology, and the presence of perforation or the development of complications were reviewed. If the CT scan revealed high density material in the appendix, the maximum CT scan radiodensity of the material is measured in Hounsfield units (HU). Barium appendicitis is defined as: (1) patients diagnosed with acute appendicitis; (2) the patient has a history of a prior barium study; and (3) the CT scan shows high density material in the appendix. Patients who meet all three criteria are considered to have barium appendicitis.
In total, 396 patients were admitted with the diagnosis of acute appendicitis in the study period. Of these, 12 patients (3.0%) met the definition of barium appendicitis. Of these 12 patients, the median CT scan radiodensity of material in the appendix was 10000.8 HU, ranging from 3066 to 23423 HU (± 6288.2). In contrast, the median CT scan radiodensity of fecaliths in the appendix, excluding patients with barium appendicitis, was 393.1 HU, ranging from 98 to 2151 HU (± 382.0). The CT scan radiodensity of material in the appendices of patients with barium appendicitis was significantly higher than in patients with nonbarium fecaliths (P < 0.01).
Barium appendicitis is not rare in Japan. Measurement of the CT scan radiodensity of material in the appendix may differentiate barium appendicitis from routine appendicitis.
Core tip: This is a retrospective study to review clinical experience with barium appendicitis at a single institution in Japan. In the three years of study period, 12 patients (3.0%) were diagnosed as barium appendicitis among 396 patients with acute appendicitis. The computed tomography (CT) scan radiodensity of material in the appendices of patients with barium appendicitis was significantly higher than in patients with nonbarium fecaliths. Barium appendicitis is not rare in Japan. Measurement of the CT scan radiodensity of material in the appendix may differentiate barium appendicitis from routine appendicitis.
- Citation: Katagiri H, Lefor AK, Kubota T, Mizokami K. Barium appendicitis: A single institution review in Japan. World J Gastrointest Surg 2016; 8(9): 651-655
- URL: https://www.wjgnet.com/1948-9366/full/v8/i9/651.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i9.651
Acute appendicitis is one of the most common surgical problems encountered in clinical surgical practice. While the exact etiology of acute appendicitis remains unclear, an obstruction of the appendiceal lumen can result in the development of acute appendicitis[1]. In Japan, upper gastrointestinal imaging using barium sulfate is widely used in mass screening programs for gastric cancer[2]. Barium sulfate is not harmful to the intestinal mucosa and complications after a barium study are considered to be very rare[2-4]. Acute appendicitis caused by residual barium is also thought to be a very rare complication after a barium study[3-5]. General surgeons in Japan often encounter patients with acute appendicitis who have residual barium felt to be the responsible etiologic agent.
We performed a retrospective review of patients admitted with a diagnosis of acute appendicitis, and specifically reviewed those with acute appendicitis suspected to be caused by residual barium.
Tokyo Bay Urayasu Ichikawa Medical Center is a secondary referral hospital in Chiba prefecture, Japan, providing acute surgical care. A retrospective analysis was conducted of patients seen from January 1, 2013 to December 31, 2015. Patients for review were identified based on their medical records including patients admitted with the diagnosis of acute appendicitis. Age, gender, computed tomography (CT) scan findings if available, past history of barium studies, pathology, and the presence of perforation or the development of complications were reviewed. If the CT scan revealed high density material in the appendix, the maximum CT scan radiodensity of the material is measured in Hounsfield units (HU).
Barium appendicitis is defined as: (1) patients diagnosed with acute appendicitis; (2) the patients have a history of a prior barium study; and (3) the CT scan shows high density material in the appendix. Patients who meet all three criteria are considered to have barium appendicitis.
Data were analyzed with Fisher’s exact test and the Mann-Whitney U test. A P-value less than 0.05 is considered statistically significant.
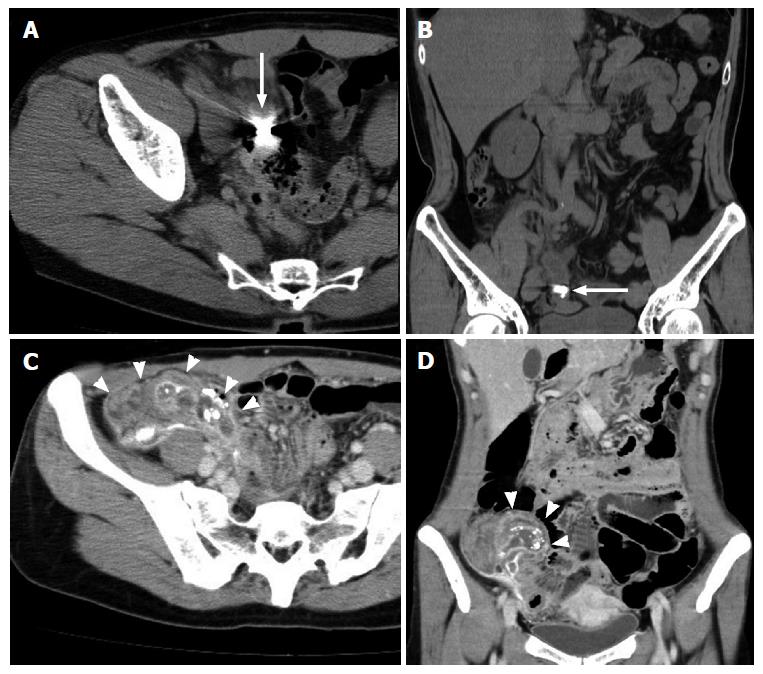
From January 1, 2013 to December 31, 2015, 396 patients were admitted with the diagnosis of acute appendicitis, including 210 males and 186 females. The median age is 37 years, ranging from 5 to 86 years. Of these, 12 patients (3.0%) met the definition of barium appendicitis (Table 1, Figure 1), including ten males and two females, with a median age of 48 years, ranging from 37 to 62 years. Of these 12 patients, the median CT scan radiodensity of material in the appendix was 10000.8 HU, ranging from 3066 to 23423 HU (± 6288.2). According to these data, the CT scan radiodensity of residual barium is generally higher than 3000 HU. If we apply this value as a cutoff, we can identify seven more patients with suspected barium appendicitis based on CT scan radiodensity alone. According to the medical records, these seven patients had no definite history of a preceding barium study, excluding one patient who specifically denied having a barium study. The median CT scan radiodensity of fecaliths in the appendix, excluding patients with barium appendicitis, was 393.1 HU, ranging from 98 to 2151 HU (± 382.0). The CT scan radiodensity of material in patients with barium appendicitis was significantly higher than patients with non-barium fecaliths (P < 0.01).
| Age | Gender | Maximum CT density (HU) | Perforation | Appendix pathology | Interval between barium study and diagnosis | Treatment |
| 52 | M | 10243 | + | Phlegmonous | 8 mo | Laparoscopic appendectomy |
| 37 | M | 23423 | - | Gangrenous | 2 d | Laparoscopic appendectomy |
| 45 | M | 6620 | - | Gangrenous | 1 mo | Laparoscopic appendectomy |
| 49 | M | 15286 | - | Phlegmonous | 16 d | Laparoscopic appendectomy |
| 44 | M | 3066 | - | Gangrenous | 1 mo | Laparoscopic appendectomy |
| 62 | M | 18286 | + | Gangrenous | Not documented | Laparoscopic appendectomy |
| 45 | M | 8192 | + | Chronic appendicitis | 3 mo | Primary non-operative management followed by interval appendectomy |
| 46 | M | 11514 | - | Phlegmonous | 10 mo | Laparoscopic appendectomy |
| 60 | F | 3178 | - | Gangrenous | Not documented | Laparoscopic appendectomy |
| 44 | M | 8727 | - | Gangrenous | 3 mo | Laparoscopic appendectomy |
| 45 | M | 7806 | - | Gangrenous | 5 mo | Laparoscopic appendectomy |
| 41 | F | 3669 | + | N/A | 1 mo | Non-operative management without interval appendectomy |
Ten of 12 patients with barium appendicitis underwent laparoscopic appendectomy urgently. One patient underwent interval laparoscopic appendectomy after initially successful non-operative management. In one patient, there was obvious perforation with abscess formation and non-operative management was initially undertaken. Following this, the patient refused interval appendectomy. The interval from barium study to the diagnosis of appendicitis was variable, ranging from 2 d to 10 mo.
The pathological results in patients with barium appendicitis are available for 11 patients. Seven patients had gangrenous appendicitis and three had phlegmonous appendicitis. One patient, who underwent interval appendectomy, had chronic inflammation of the appendix. The rate of gangrenous appendicitis is 58.3% in patients with barium appendicitis and 56.4% in patients without barium appendicitis. The rate of gangrenous appendicitis is almost the same in patients with typical (unassociated with barium) appendicitis compared to patients with barium appendicitis. Four out of 12 patients had a perforation (33.3%), confirmed by intraoperative or imaging findings. The perforation rate in patients with barium appendicitis was higher than in patients without barium appendicitis (18.8% in this study), which is not statistically significant (P = 0.25). Interestingly, although the rate of gangrenous appendicitis is almost the same in patients with barium appendicitis and typical appdndicitis the perforation rate was higher in patients with barium appendicitis.
Barium appendicitis is a rare complication after barium examinations and was first described by Gubler et al[6] in 1954. Although retained barium in the appendix after barium studies is very common[7], especially after colon studies, more than 90% of patients evacuate the barium within 72 h[3,4,7]. The true pathophysiology of barium appendicitis remains unclear. The true incidence of barium appendicitis is also unknown because only a few case reports or small case series have been reported to date[3-7]. The time interval between the barium study and the diagnosis of barium appendicitis in several previous studies ranges from four hours to four years[5,8]. In the present study, the range is 10 d to 10 mo. The wide range of values suggests that retained barium in the appendix alone does not result in appendicitis. There would appear to be other factors that contribute to the development of acute appendicitis.
Acute appendicitis is one of the most common surgical emergencies encountered by general surgeons. Obstruction of the appendiceal lumen, often due to a fecalith, lymphoid hyperplasia, or rarely a cecal or appendiceal tumor, is generally thought to be the cause of acute appendicitis in many patients[1,9]. Fecaliths are a cause of obstruction of the appendiceal lumen, although they are not always found at surgery. Fecaliths are composed of inspissated stool, mucus with trapped calcium phosphate and inorganic salts, which finally obstructs the appendiceal lumen[10,11]. In this study, fecaliths were identified in 34% of patients with acute appendicitis based on imaging findings. It is unknown if the high density material in the appendix in patients with barium appendicitis is composed of only barium or if it is combined with other material such as that found in a fecalith. However, luminal obstruction of the appendix by residual barium resulted in the development of acute appendicitis. As mentioned, an additional cause of barium appendicitis may be a pre-existing fecalith in the appendix. Fecaliths not only cause appendicitis, but also are considered to be associated with appendiceal perforation[11,12]. In this study, the perforation rate in patients with barium appendicitis was higher than in patients without barium appendicitis. Although it is not statistically significant, this suggests that residual barium may be a risk factor for appendiceal perforation, similar to a fecalith. The fact that typical appendicitis has the same rate of gangrenous inflammation in this study also supports this hypothesis.
In this study, the CT scan radiodensity of material in the appendix in patients with barium appendicitis is significantly higher than that of fecaliths in patients with typical appendicitis. These data suggest that the CT scan radiodensity of material in the appendix may differentiate barium from normal fecaliths. We acknowledge that in general, not all patients undergo CT scans to establish the diagnosis of acute appendicitis. However, during the study period, about 3% of patients presented with acute appendicitis believed to be caused by residual barium. Since acute appendicitis is one of the most common surgical emergencies, and the fact that in Japan, barium is widely used in studies screening for gastric cancer[2], we believe that the diagnosis and recognition of barium appendicitis as a complication of barium studies is worthwhile, especially in Japan.
According to data reporting the complications after gastric cancer screening in Japan, the total complication rate after barium studies is reported to be less than 0.04%[13]. The most common reported complication after barium studies was aspiration, followed by allergic reaction and bowel obstruction. There have also been severe complications reported such as intestinal perforation due to residual barium[13]. Interestingly, there were no reports of barium appendicitis[13], although barium appendicitis occurred in 3% of patients with acute appendicitis in this study. There is an approximate 7% lifetime risk of developing appendicitis[1,9], thus, a 3% incidence in patients with acute appendicitis is a significant number. Since acute appendicitis is often treated with appendectomy no matter what the etiology, the true incidence of barium appendicitis is likely underestimated.
Several limitations are acknowledged in this study. First, this is a single institution retrospective analysis. Second, there is no confirmation of what the high density material in the resected appendices actually was. Pathological confirmation may support the results of this study, if it is specifically checked in a prospective study.
In conclusion, barium appendicitis is not rare in Japan. Measurement of the CT scan radiodensity of material in the appendix may differentiate barium appendicitis from routine appendicitis. Since barium is widely used in Japan for gastric cancer screening, determination of the true incidence of barium appendicitis is important.
This material was presented in part at the 116th annual congress of the Japan Surgical Society (April 15th 2016, Osaka, Japan).
Barium appendicitis is a rare complication of gastrointestinal imaging using barium sulfate. The true incidence of barium appendicitis is unknown. However, general surgeons in Japan often encounter patients with acute appendicitis where the etiology appears to be a barolith in the appendix. The authors review their clinical experience with barium appendicitis at a single institution in Japan.
The exact incidence of barium appendicitis is unknown. This study reviews their experience with appendicitis and the incidence of barium appendicitis among all patients who presented with acute appendicitis.
Barium appendicitis is thought to be a rare complication of gastrointestinal imaging. However, this study shows that barium appendicitis represents about 3% of all patients with acute appendicitis.
Measurement of the computed tomography (CT) scan radiodensity of high density material in the appendix may help to differentiate barium appendicitis from typical appendicitis. This may also help elucidate the true incidence of barium appendicitis in future studies.
HU: Hounsfield units.
Barium appendicitis is a rare clinical condition. Barolith can occur due to post-examination retained barium in appendix lumen and it can cause appendicitis. CT definings in this manuscript is well-thought evidence and helps diagnose.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Charfi S, Ince V S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 684] [Article Influence: 68.4] [Reference Citation Analysis (0)] |
| 2. | Hamashima C, Shibuya D, Yamazaki H, Inoue K, Fukao A, Saito H, Sobue T. The Japanese guidelines for gastric cancer screening. Jpn J Clin Oncol. 2008;38:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 275] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 3. | Urade M, Shinbo T. Barium appendicitis 1 month after a barium meal. Int Surg. 2012;97:296-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Fang YJ, Wang HP, Ho CM, Liu KL. Barium appendicitis. Surgery. 2009;146:957-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Novotny NM, Lillemoe KD, Falimirski ME. Barium appendicitis after upper gastrointestinal imaging. J Emerg Med. 2010;38:148-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Gubler JA, Kukral AJ. Barium appendicitis. J Int Coll Surg. 1954;21:379-384. [PubMed] |
| 7. | Maglinte DD, Bush ML, Aruta EV, Bullington GE. Retained barium n the appendix: diagnostic and clinical significance. AJR Am J Roentgenol. 1981;137:529-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Cohen N, Modai D, Rosen A, Golik A, Weissgarten J. Barium appendicitis: fact or fancy? Report of a case and review of the literature. J Clin Gastroenterol. 1987;9:447-451. [PubMed] |
| 9. | Engin O, Muratli A, Ucar AD, Tekin V, Calik B, Tosun A. The importance of fecaliths in the aetiology of acute appendicitis. Chirurgia (Bucur). 2012;107:756-760. [PubMed] |
| 10. | Maatouk M, Bunni J, Schuijtvlot M. Perihepatic abscess secondary to retained appendicolith: A rare complication managed laparoscopically. J Surg Case Rep. 2011;2011:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Alaedeen DI, Cook M, Chwals WJ. Appendiceal fecalith is associated with early perforation in pediatric patients. J Pediatr Surg. 2008;43:889-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Singh JP, Mariadason JG. Role of the faecolith in modern-day appendicitis. Ann R Coll Surg Engl. 2013;95:48-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Shibuya D, Ishikawa T, Ichinose M, Iriguchi Y, Kitagawa S, Tobori F, et . al. Annual report of complications related to gastric cancer screening: results of the Japanese Society of Gastrointestinal Cancer Screening survey from April 1, 2012 to March 31, 2013. (Title and article in Japanese). J Gastrointestinal Cancer Screen. 2015;53:233-238. [DOI] [Full Text] |