Published online Aug 27, 2016. doi: 10.4240/wjgs.v8.i8.564
Peer-review started: March 28, 2016
First decision: April 26, 2016
Revised: May 4, 2016
Accepted: May 17, 2016
Article in press: May 27, 2016
Published online: August 27, 2016
Processing time: 151 Days and 22.5 Hours
This work is a topic highlight on the surgical treatment of the right colon pathologies, focusing on the literature state of art and comparing the open surgery to the different laparoscopic and robotic procedures. Different laparoscopic procedures have been described for the treatment of right colon tumors: Totally laparoscopic right colectomy, laparoscopic assisted right colectomy, laparoscopic facilitated right colectomy, hand-assisted right colectomy, single incision laparoscopic surgery colectomy, robotic right colectomy. Two main characteristics of these techniques are the different type of anastomosis: Intracorporeal (for totally laparoscopic right colectomy, single incision laparoscopic surgery colectomy, laparoscopic assisted right colectomy and robotic technique) or extracorporeal (for laparoscopic assisted right colectomy, laparoscopic facilitated right colectomy, hand-assisted right colectomy and open right colectomy) and the different incision (suprapubic, median or transverse on the right side of abdomen). The different laparoscopic techniques meet the same oncological criteria of radicalism as the open surgery for the right colon. The totally laparoscopic right colectomy with intracorporeal anastomosis and even more the single incision laparoscopic surgery colectomy, remain a technical challenge due to the complexity of procedures (especially for the single incision laparoscopic surgery colectomy) and the particular right colon vascular anatomy but they seem to have some theoretical advantages compared to the other laparoscopic and open procedures. Data reported in literature while confirming the advantages of laparoscopic approach, do not allow to solve controversies about which is the best laparoscopic technique (Intracorporeal vs Extracorporeal Anastomosis) to treat the right colon cancer. However, the laparoscopic techniques with intracorporeal anastomosis for the right colon seem to show some theoretical advantages (functional, technical, oncological and cosmetic advantages) even if all studies conclude that further prospective randomized trials are necessary. Robotic technique may be useful to overcome the problems related to inexperience in laparoscopy in some surgical centers.
Core tip: We report a topic highlight of the mini-invasive treatment of the right colon pathologies, focusing on the Literature State of Art and comparing the open surgery vs the different laparoscopic and robotic procedures. We try to analyze the different current approaches to right colon cancer treatment focusing in particular light and shadows of totally laparoscopic right colectomy compared to other mini-invasive (single incision laparoscopic colectomy, laparoscopic assisted right colectomy, laparoscopic facilitated right colectomy, hand-assisted right colectomy, robotic right colectomy) and open procedure. The two main characteristics of these techniques are the different type of anastomosis: Intracorporeal or extracorporeal and the different incision (suprapubic vs median vs transverse on right side of abdomen). The different laparoscopic techniques meet the same oncological criteria of radicalism as the open surgery for the right colon. The laparoscopic techniques with intracorporeal anastomosis for the right colon remain a technical challenge but they seem to have some theoretical advantages compared to the other laparoscopic and open procedures described in our study even if further prospective randomized trials are necessary to confirm it.
- Citation: Fabozzi M, Cirillo P, Corcione F. Surgical approach to right colon cancer: From open technique to robot. State of art. World J Gastrointest Surg 2016; 8(8): 564-573
- URL: https://www.wjgnet.com/1948-9366/full/v8/i8/564.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i8.564
The laparoscopic treatment for benign and malignant pathologies of the left colon and rectum is actually accepted and validated. Laparoscopy advantages are widely demonstrated in term of: Post-operative pain reduction, early resumption of the intestinal function, decreasing in hospital stay, time to return to work and better cosmetic results. The oncologic outcomes are the same than open surgery[1]. These results are also achieved thanks to the development of Kehlet “Fast-Track” recovery protocols. The laparoscopic technique for the right colon instead, had a slower diffusion probably for the complexity of right colon laparoscopic anatomy and the variability of the vascular peduncles that require a greater laparoscopic experience than left colon and rectum surgery. For these reasons, many surgeons consider the laparoscopic approach to right colon an useless and complex waste of time[2].
Different laparoscopic hybrid procedures developed but there are not sure evidences which is the best one and also the role of laparoscopy itself in the right colon treatment remains controversial.
The aim of the study is to critically analyze the literature state of art on right colectomy, focusing on the lights and shadows of laparoscopic and robotic approach in relation to open surgery and comparing the different laparoscopic procedures.
Right colectomy is indicated for malignant pathologies involving the intestinal tract between the ileocecal Bahuino valve and the colonic hepatic flexure. Laparoscopic resection must respect the same oncologic criteria as the open approach including: “no-touch isolation technique’’, isolation and ligation of the vascular pedicles at the origin, oncologic lymphadenectomy and “distal and radial clearance’’ of the neoplasm from resection margins[3,4].
Different laparoscopic procedures have been described for the treatment of right colon tumors: (1) totally laparoscopic right colectomy (TLC) which provides all steps conducted in laparoscopy including Intracorporeal ileo-colic Anastomosis (IA)[5]; (2) single incision laparoscopic surgery (SILS) for right colon (SILC) allows to perform the intervention laparoscopically (with intracorporeal anastomosis) through larger multichannel single (about 3 cm diameter) trocar and curved instruments[6,7]; (3) laparoscopic assisted right colectomy (LAC) which provides laparoscopic vessel ligations and right colon mobilization but the ileo-colic Anastomosis is performed extracorporeally by open incision (EA)[8,9]; (4) laparoscopic facilitated right colectomy (LFC), a variant of laparoscopic assisted, which provides only the laparoscopic right colon mobilization while the vessels ligation and anastomosis are extracorporeally (EA)[10]; (5) hand-assisted right colectomy (HAC) with laparoscopic mobilization of colon by hand help through a right side minilaparotomy and extracorporeal anastomosis[11,12]; and (6) robotic right colectomy (RRC) with manual intracorporeal anastomosis[13].
The two main characteristics of these techniques are the different type of anastomosis and minilaparotomies. The anastomosis may be performed in intracorporeal way for TLC, SILC and RRC or extracorporeally for LAC, LFC, HAC and open right colectomy. The minilaparotomy is generally performed in suprapubic region (a Pfannestiel of about 5-6 cm) in the TLC, SILC[14,15] and RRC for the specimen extraction while it is performed median in periumbilical site or transverse in right side of abdomen (about 10-12 cm of length) in LAC, LFC, HAC and open surgery to extract the specimen and to make the EA.
In the SILC, the specimen extraction can also be performed through the umbilicus eventually used to make the anastomosis extracorporeally[16].
Several studies including meta-analysis demonstrated the advantages of laparoscopic vs open approach for the treatment of right colon cancer in short term outcomes (Table 1): Minimal invasiveness, reduced blood loss, less postoperative pain, earlier first flatus, shorter hospital stay and reduced rate of wound infections and incisional hernias. No differences, instead, were found between the two techniques for other complications such as: pneumonia, anastomotic leaks, ileus, deep venous thrombosis or pulmonary embolism[17]. The number of nodes taken out, the post-operative (p.o.) mortality and cancer recurrence were not statistically different in the two groups[17-26].
| Ref. | Patient number LS/OS | Mean operative time (min) LS/OS | Blood loss (mL) LS/OS | Harvested nodes LS/OS | First flatus/defecation (d) LS/OS | P.O. Complications (patients) LS/OS | Hospital stay LS/OS | Mortality LS/OS |
| Ramacciato et al[20] | 33/33 | 251/222.91 | 135/4041 | 12.7/181 | 3.15/3 | 1/41 | 11.2/13.81 | 0/0 |
| Khan et al[21] | 89/75 | 120/NR | NR | 15/13 | NR | 0/41 | 4/81 | 0/41 |
| Veldkamp et al[22] | 627/621 | 145/1151 | 100/1751 | NS | 3.6/4.61 | NS | 8.2/9.31 | NS |
| Lohsiriwat et al[23] | 13/20 | 207.7/104.51 | 120/107 | 29.2/18.8 | 2.4/2.6 | 1/0 | 6.2/7.1 | 0/0 |
| Guillou et al[24] | 484/253 | NR | NR | 12/35 | 5/6 | NR | 9/11 | 21/13 |
| Abdel-Halim et al[25] | 22/34 | 187/1301 | NR | 23.8/21.2 | 3/41 | 4/9 | 6/101 | 1/2 |
| Zhao et al[26] | 119/101 | 170.7/244.4 | 100/1501 | 22.3/21.8 | 2.7/3.21 | 11.8/17.6% | 11.4/12.81 | 1/1 |
In some studies, the operative time was statistically longer in laparoscopy (LS) and it is connected to the learning curve[27].
The limits of the studies reported in literature are related to the lack of double blinded randomized clinical trials which determines selection bias, to the different experience of the Surgical Centers which cannot be judged by a single paper and to different patient’s management. Consequently, more randomized clinical trials with same standardized preoperative and postoperative enhanced protocols for patient’s management must be conducted by High Specialized Surgical Centers.
About long term outcomes, the study of Guerrieri et al[28] reported in the open surgery group an increased risk of local recurrence, metastasis and cancer-related mortality, while a meta-analysis of Reza et al[29] showed no difference between LS and open surgery (OS) groups for cancer related mortality or disease recurrence during five-year follow-up. Han et al[30] confirmed the same results with no statistically difference between LS and OS groups for overall survival at 1-, 3- and 5-year follow-up for all tumor stages.
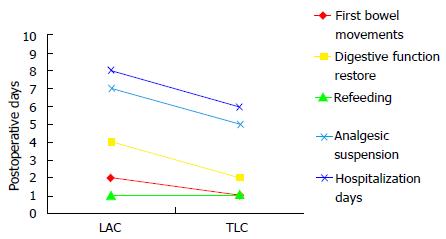
A recent meta-analysis of Feroci et al[31] compares the intracorporeal and extracorporeal anastomosis considering short term outcomes. The two techniques do not show significant differences in term of mortality, surgical and non surgical complications. In Fabozzi et al[32] study, the TLC (with IA) group presents some advantages about post-operative recovery in particular regarding: Earlier first flatus, earlier food intake, reduced analgesic consumption, shorter hospital stay vs LAC (with EA) group (Figure 1). These better results may be explained by the less intestinal manipulation in the IA group thanks to the lesser dissection (lesser p.o. adhesions) and mobilization of transverse colon at the cost of longer operative time and higher laparoscopic experience[32-34].
On the contrary, some authors (Table 2) reported different results: shorter operative time and hospital stay in LAC vs TLC group, remarking the necessity of further controlled studies[9,32,33,35-38] .
| Ref. | Patient number TLC/LAC | Length of skin incision (mm) TLC/LAC | Mean operative time (min) TLC/LAC | Blood loss (mL) TLC/LAC | Harvested nodes TLC/LAC | First flatus/defecation (d) TLC/LAC | P.O. Complications (patients) TLC/LAC | Hospital stay TLC/LAC | Mortality TLC/LAC |
| Roscio et al[33] | 42/30 | 48.2/711 | 176.5/186.3 | 31.2/43.3 | 25.9/22 | 2.9/3.41 | 1/2 | 6.2/7.21 | 0/1 |
| Fabozzi et al[32] | 50/50 | 60/1201 | 78/921 | NR | 16/17 | 1.3/2.61 | 0/141 | 5.3/7.61 | 0/0 |
| Scatizzi et al[35] | 40/40 | 50/40 | 150/150 | NR | 30/26 | 0/1 | 3/3 | 5/5 | 0/0 |
| Hellan et al[36] | 23/57 | 40/501 | 190/180 | 50/100 | 18/17 | NS | 6/14 | 4/4 | 0/1 |
| Magistro et al[9] | 40/40 | 55/721 | 230/2031 | NR | 22/20 | 2.2/2.61 | 7/8 | 6.3/6 | 0/1 |
| Chaves et al[37] | 35/25 | NR | 226/2081 | NR | 20.6/14.2 | 3/41 | 7/5 | 6/81 | 1/1 |
| Grams et al[38] | 54/51 | NR | 190/1561 | NS | NR | 2/2.4 | 6/15 | 3.2/3.81 | 1/1 |
All authors, fortunately, agree about the absolute indication to TLC with IA in obese patients, who present some factors interfering with EA: Greater wall thickness, shorter and thick mesentery causing the necessity of enlarging minilaparotomy to perform the colonic resection and EA.
The goal of treatment in colon cancer outcomes should be the number of lymph nodes harvested: This is similar in TLC (IA) and LAC (EA) groups because the vessel legation was conducted in the same intracorporeal way (Table 2). The lymph nodes removal, in fact, is influenced by the level of vessel ligation which must be performed at the origin from Superior Mesenteric Artery. This technical point explains why it is more difficult to obtain a sufficient number (at least 12) of lymph nodes through a right sided abdominal small incision of the LFC and HAC.
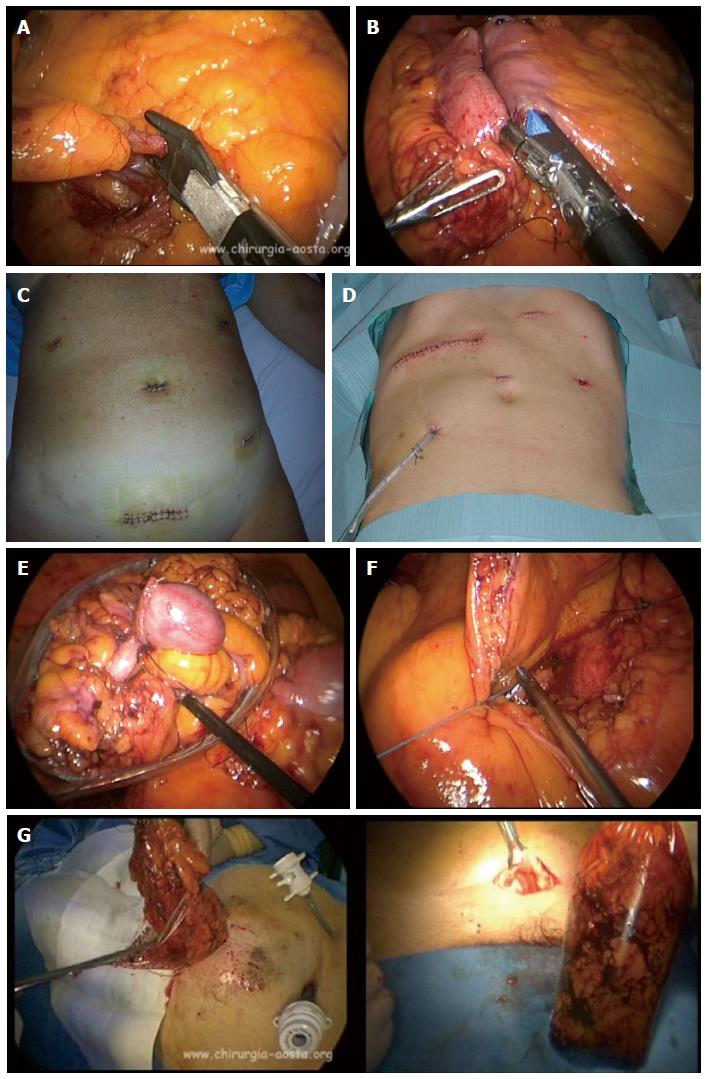
The right colon dissection with the median to lateral approach in TLC in fact, consents to achieve a good exposure of all colonic vessels: The ileo-colic trunk, the right colic artery, the right branch of the median colic artery (Figure 2A). The most difficult step is the nodal dissection at the origin of the median colic vein and of the Henle’s trunk that could increase a risk of bleeding, so a great expertise and laparoscopic skill are requested[39].
TLC provides a mechanical (stapled side to side anastomosis) IA (Figure 2B) while EA procedures can have a stapled or hand-sewn anastomosis. A recent Cochrane systematic review reported a lower rate of anastomotic leakage in stapled ileo-colic anastomosis compared to hand-sewn anastomosis[40]. The safety of both types of side to side anastomosis (hand-sewn running suture anastomosis vs stapled EA) is well known but the advantages of mechanical anastomosis could be due to the standardization of anastomosis (60 mm blue cartridge) and the faster performance that do not depend from the ability of surgeon[31].
In Fabozzi et al[32] TLC has better postoperative recovery outcomes such as shorter hospital stay, faster bowel movements and also better aesthetic results thanks to the minor size and site of minilaparotomy (in suprapubic region) (Figure 2C) which also determines less post-operative pain and p.o. analgesia and less risk of incisional hernias. The suprapubic incision (in IA procedures) in fact, is subjected to less abdominal pressure (compared to right sided abdominal incision in EA procedures) and it is not influenced by diaphragmatic movements that can increase the p.o. pain. Moreover, the pain of the right side incision (Figure 2D) can also reduce diaphragmatic and respiratory movements determining a higher risk of pulmonary infections (Table 3)[31,32].
| Laparotomy | Suprapubic | Right hypocondrium |
| Dimension | ↓ | ↑ |
| Wound infection | ↓ | ↑ |
| Incisional hernia | ↓ | ↑ |
| P.O. pain | ↓ | ↑ |
| Respiratory function | ↓ | ↑ |
Other studies compare transverse vs midline incision showing better outcomes in term of p.o. morbidity, hospital stay and incisional hernia in the first one[33,41,42].
The cost of procedures is lower in case of EA (Open, LAC, LFA) compared to IA of TLC and RRC due to longer operative time and use of instruments but the cost of drugs is significantly higher in EA than IA group related to duration of p.o. use of analgesics[31]. The only one study published on the long term results is by Lee et al[43], reporting no difference in survival and disease free survival at 3 years follow-up between the two groups (IA vs EA).
The limits of literature data depend on the large amount of non-randomized studies which leads to a bias giving preferential choice to the more difficult technique (TLC with IA).
Open questions remain the operating time that is related to the learning curve to reach the laparoscopic suture skill, and the oncological long term results connected to a correct nodal clearance for which there is lacking of high grade evidences.
Single incision laparoscopic surgery is a recently introduced mini-invasive procedure performed through single skin access of 3-4 cm using a larger multichannel port. It was first used for laparoscopic colecistectomy and appendectomy and later it has been tested for other procedures[16]. Colorectal SILS was first performed in 2008[44]. The umbilicus is the most common access for the SILS procedures (in particular for right colon) but some surgeons prefer to use other sites (such as the right side of abdomen) for example when a diverting stoma is planned[7,16]. The SILC port is generally composed by 3 or 4 channel (depending on type): 1 of 10 mm for the 30º camera, 1 of 12 mm for stapler or other instruments and other 1 or 2 channels of 5 mm for specific curved instruments to allow the inverse triangulation and to facilitate the movements in operative field[15,16]. The specimen was generally removed through a suprapubic incision or enlarging (if necessary) the umbilical incision[7,15,16]. Despite the experience in SILS is recently improved and many papers are appeared in literature, the technical difficulties of procedure, the prolonged learning curve and the oncological results are still object of discussion[16,45].
Recent study of Yun et al[46] reported same oncologic results in SILS compared to conventional laparoscopy for colon cancer.
A systematic review on 881 patients (389 SILC vs 492 Multiport) of Vettoretto et al[47] reported no statistical difference between the two techniques in morbidity and mortality, number of lymphnodes harvested and disease free survival at 24 mo. Other outcomes such as operative time, post-operative analgesic use, blood loss, anastomotic leaks rate, first flatus and hospital stay were not analyzed due to the lack of data.
A randomized clinical trial of Poon et al[48] on 25 patients reported a reduced p.o. pain and hospital stay in SILS procedure even if further randomized clinical trials are necessary.
In the SILS specimen extraction can be performed through the umbilicus, also used to make the anastomosis extracorporeally. The extracorporeal anastomosis allows shorter operative time, so some surgeons prefer it especially in their early experience. Instead, the minilaparotomy can be performed in suprapubic region to extract the specimen when intracorporeal anastomosis is made[47].
A certain benefit of SILS is the better cosmetic result comparing to the other mini-invasive and open procedures even if some authors think that cosmetic evaluation must be made after the complete wound healing[49].
Another metanalysis of Yang et al[50] reported smaller incisions, less blood lost and more lymphnodes removed with same results in p.o. morbidity and operative time.
With the progressive diffusion of the SILS and the improvement of surgeons experience, its cost became almost the same of conventional laparoscopy[49].
The major spreading of EA techniques depends on their major feasibility compared to IA of TLC. The use of Robot (Da Vinci System™) has simplified the laparoscopic procedure allowing the surgeons who do not make laparoscopy to overcome the learning curve of minimally invasive surgery. The robotic technique plays the same steps of open surgery with the advantages of the minimally invasiveness (including the better vision) but it is easier than laparoscopy.
According to Trastulli et al[13] the use of Robot facilitates an extended lymphadenectomy through a complete mesocolon excision if compared to laparoscopy.
Robotic surgery is safe and could be an effective alternative to conventional LS. Like laparoscopy, it avoids the big incision, reduces pain, allows early mobilization, and diminishes general (respiratory and circulatory) and local complications (wound infection and incisional hernia). Global morbidity and mortality rate is generally lower than all types of corresponding open interventions.
Moreover, the Da Vinci Intuitive Xi™ Robotic System could allow interventions to be more effective and reliable than traditional laparoscopic techniques and faster in terms of operative but not total time because it includes the time for system setup too. Robotic surgery, restoring the hand-eye coordination and three-dimensional view lost in laparoscopic surgery, filtrating hand tremors, giving more freedom degrees to instruments and amplifying different motion scale, could allow to perform complex procedures with greater precision and better results[51,52]. Thus, difficult laparoscopic interventions may become easier to perform, and the indications for robotic and minimal invasive surgery could be generally extended despite the long setup time.
A recent meta-analysis of Xu et al[53] reports the advantages of robotic approach compared to laparoscopy in treatment of right colon cancer. In particular, RRC seems to be associated with lower blood losses, reduced p.o. complications and a faster restore of bowel functions despite a long operative time. In literature the benefits of laparoscopy vs open surgery in the treatment of colorectal surgery are well known: Smaller incision, less blood loss, less p.o. pain, early resume to normal diet and intestinal function, short hospital stay and quickly return of the patients to daily life activities. On the other side, the laparoscopic approach for the right colon shows some technical difficulties connected to the lack of fixed anatomical landmarks (as we mentioned before) and to the laparoscopy itself such as the lack of three dimensional vision, the complex dissection and suturing, so it is performed only by expert surgeons with good results. The Da Vinci Xi Robot SystemTM allows to overcome all laparoscopic technical difficulties (three dimensional vision, easy suturing, filtering tremor movements with surgeon comfortable sitting) combining the advantages of minimally invasive surgery and open surgery[53].
Actually, the higher costs of the robotic surgical instruments, as compared with the cost of the laparoscopic instruments, represent the real disadvantage of this new technique.
However, the absence of a sufficient number of patient follow-up in the literature does not allow having data on long term results.
A schematic representation of the advantages or disadvantages of each technique is reported in Table 4[13,14,16,29,32,33,41,47,51,52].
| Parameters | Open right colectomy | LAC | TLC | SILC | RRC |
| Laparotomy site and dimension | Transverse (on right side ) Median (10-12 cm) | Transverse (on right side) (7-13.5 cm) | Suprapubic (48-13 cm) | Suprapubic Umbilical (median) (3-4.5 cm) | Suprapubic (4-6 cm) |
| Type of anastomosis | EA | EA | IA | IA/EA | IA |
| 3D vision | Yes | No | No | No | Yes |
| Surgeon hand tremor filtering | No | No | No | No | Yes |
| High-precision movements and suturing | No | No | No | No | Yes |
| Technical difficulty | ↓ | ↑ | ↑↑ | ↑↑↑ | ↓ |
| Surgeon’s comfort (dock station) | ↓ | ↓ | ↓ | ↓↓↓ | ↑ |
| Patient’s comfort | ↓ | ↓ | ↑↑ | ↑↑ | ↑↑ |
| Costs | ↓ | ↑ | ↑ | ↑ | ↑↑↑ |
The different laparoscopic techniques meet the same oncological criteria of radicalism as the open surgery for the right colon: Absence of tumor manipulation (“no touch techniques”), section at the origin of the right vascular peduncles and the “distal and radial clearance” of the neoplasm margins[54]. The TLC and even more the SILC with IA remain a technical challenge due to the complexity of procedures (especially for the SILC) and the particular right colon vascular anatomy but they seem to have some theoretical advantages than the other mini-invasive and open procedures[26,32,33,46]:
The extraction of the operative specimen by 15 cm endobag through a suprapubic incision prevents the tumor squeezing and neoplastic cells spreading (Figure 2E and G).
The closure of mesentery by non-absorbable running suture (Figure 2G) especially in obese patients is easier in laparoscopic procedures with IA thanks to its better vision and exposure. The laparoscopic suturing of mesentery reduces the risks of internal hernia and avoids traction on vascular and nervous peduncles (as it could happen in case of EA) which is one of the cause of the delayed canalization.
The suprapubic incision (a little Pfannestiel) for the specimen removal is smaller (about 5 cm) than other laparoscopic techniques (about 8 cm) and open technique (about 10 cm) (Figure 2C and D). The smaller dimension and the site of incision reduce the postoperative pain with less assumption of analgesic drugs, promoting early mobilization of patients and recovery of intestinal function, better respiratory exchanges, better tissue (and anastomotic) oxygenation, faster healing and coming back to ordinary life. In fact, the major dimensions and right sided abdomen (or median) incision of non totally laparoscopic and open techniques with muscles section cause greater pain, reducing the respiratory excursions especially in the elder and favouring pulmonary complications with prolonged hospitalization and higher risk of incisional hernias as reported by some authors[32,33,36,41,42] (Table 3).
The smaller dimension and the suprapubic (TLC, SILC) or umbilical (SILC) site incision determine better aesthetic results than other mini-invasive and open right colon techniques (larger incision on the right side of the abdomen).
Although some good short term outcomes, TLC and SILS with IA have the limitation of a minor tactile feedback and a steep learning curve (longer in SILS)[16,45]. Despite advances in technologies and devices, the laparoscopic procedures require dexterity and technical skill. In a study of Tekkis et al[27] the evidences demonstrated that colorectal surgeons with an experience of 0-25 procedures have a significant higher risk of conversion to open surgery respect to surgeons with over 175 procedures. Surgeons with a 25 laparoscopic colectomies experience employed a median of 180 min for procedure, while at the 175th procedure the median operating time is 115 min. To reach good results with TLC, it is mandatory to overcome specific technical steps (laparoscopic intracorporeal running suture, mechanical stapler use, correct bowel orientation) supported by expert staff assistance and advanced technology.
After these assumptions, TLC may be considered feasible and safe techniques, even if it requires a great experience not only in laparoscopy but also in open surgery to ensure better p.o. results, better comfort for the patients and similar oncological outcomes to the open surgery[27,32,55].
The SILC may be considered a valid alternative to TLC thanks to similar p.o. outcomes but a longer learning curve than TLC is required in addition to a great experience in laparoscopic and open surgery. It seems to report better cosmetic results, even if in TLC, the suprapubic scare would be also covered by the brief. It not clear instead, if it has an higher incisional hernia rate or p.o pain due to the median site of incision compared to suprapubic incision (of TLC) and right sided incision of other procedures[32,36,41,42,47].
Recently, an early experience of Robotic SILC reported a longer operative time, higher conversion rate and 27% of p.o. complications rate (in particular: Wound hematomas, infections and incisional hernias of the umbilicus)[56].
The LAC instead, could be considered an alternative to both TLC and SILC for the surgeons with early experience in laparoscopic advanced procedures or to avoid a primary open surgery of the right colon or a conversion to open surgery due to technical problems related to difficult anatomy, surgical experience or intraoperative complications untreatable in laparoscopy[57].
Some authors report that HAC procedure has not advantages respect to LAC in term of clinical and oncological results but it could have some advantages in case of bulky tumors treatment[11].
Data reported in literature while confirming the advantages of laparoscopic approach, do not allow to solve controversies about which is the best laparoscopic technique (IA vs EA) to treat the right colon cancer: some authors consider a mini-invasive right colectomy with IA as “a triumph of technique over the common sense” while for others is “an illogical waste of time”. For these reasons, all the studies reported in literature conclude that further prospective randomized trials are necessary.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Hsu CW, Kim YW S- Editor: Qi Y L- Editor: A E- Editor: Wu HL
| 1. | Künzli BM, Friess H, Shrikhande SV. Is laparoscopic colorectal cancer surgery equal to open surgery? An evidence based perspective. World J Gastrointest Surg. 2010;2:101-108. [PubMed] |
| 2. | Bailey MB, Davenport DL, Vargas HD, Evers BM, McKenzie SP. Longer operative time: deterioration of clinical outcomes of laparoscopic colectomy versus open colectomy. Dis Colon Rectum. 2014;57:616-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Kornmann VN, Hagendoorn J, van Koeverden S, van Ramshorst B, Smits AB. Totally laparoscopic right hemicolectomy with intracorporeal anastomosis is a technically and oncologically safe procedure. Acta Chir Belg. 2013;113:439-443. [PubMed] |
| 4. | Kanemitsu Y, Komori K, Kimura K, Kato T. D3 Lymph Node Dissection in Right Hemicolectomy with a No-touch Isolation Technique in Patients With Colon Cancer. Dis Colon Rectum. 2013;56:815-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | Facy O, De Magistris L, Poulain V, Goergen M, Orlando G, Azagra JS. Right colectomy: value of the totally laparoscopic approach. J Visc Surg. 2013;150:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Kim SJ, Choi BJ, Lee SC. Overview of single-port laparoscopic surgery for colorectal cancers: past, present, and the future. World J Gastroenterol. 2014;20:997-1004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Lim SW, Kim HR, Kim YJ. Single incision laparoscopic colectomy for colorectal cancer: comparison with conventional laparoscopic colectomy. Ann Surg Treat Res. 2014;87:131-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Marchesi F, Pinna F, Percalli L, Cecchini S, Riccó M, Costi R, Pattonieri V, Roncoroni L. Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assisted approach. J Laparoendosc Adv Surg Tech A. 2013;23:418-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Magistro C, Lernia SD, Ferrari G, Zullino A, Mazzola M, De Martini P, De Carli S, Forgione A, Bertoglio CL, Pugliese R. Totally laparoscopic versus laparoscopic-assisted right colectomy for colon cancer: is there any advantage in short-term outcomes? A prospective comparative assessment in our center. Surg Endosc. 2013;27:2613-2618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Cirocchi R, Trastulli S, Farinella E, Guarino S, Desiderio J, Boselli C, Parisi A, Noya G, Slim K. Intracorporeal versus extracorporeal anastomosis during laparoscopic right hemicolectomy - systematic review and meta-analysis. Surg Oncol. 2013;22:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Kim H. Hand-assisted laparoscopic right colectomy: is it useful? Ann Coloproctol. 2014;30:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Meng WJ, Wang ZQ, Zhou ZG. Hand-assisted laparoscopic right colectomy: a consideration of hand-device placement and trocar arrangement. Colorectal Dis. 2013;15:910-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Trastulli S, Coratti A, Guarino S, Piagnerelli R, Annecchiarico M, Coratti F, Di Marino M, Ricci F, Desiderio J, Cirocchi R. Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc. 2015;29:1512-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 14. | Stein SA, Bergamaschi R. Extracorporeal versus intracorporeal ileocolic anastomosis. Tech Coloproctol. 2013;17 Suppl 1:S35-S39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Dapri G, Carandina S, Mathonet P, Himpens J, Cadière GB. Suprapubic single-incision laparoscopic right hemicolectomy with intracorporeal anastomosis. Surg Innov. 2013;20:484-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Velthuis S, van den Boezem PB, Lips DJ, Prins HA, Cuesta MA, Sietses C. Comparison of short-term surgical outcomes after single-incision laparoscopic versus multiport laparoscopic right colectomy: a two-center, prospective case-controlled study of 100 patients. Dig Surg. 2012;29:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Ding J, Liao GQ, Xia Y, Zhang ZM, Liu S, Yan ZS. Laparoscopic versus open right hemicolectomy for colon cancer: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2013;23:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Hitchins CR, Trickett JP, Scott HJ. Clinical outcome of laparoscopic and open colectomy for right colonic carcinoma. Ann R Coll Surg Engl. 2012;94:288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Rondelli F, Trastulli S, Avenia N, Schillaci G, Cirocchi R, Gullà N, Mariani E, Bistoni G, Noya G. Is laparoscopic right colectomy more effective than open resection? A meta-analysis of randomized and nonrandomized studies. Colorectal Dis. 2012;14:e447-e469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 20. | Ramacciato G, D’Angelo F, Aurello P, Nigri G, Valabrega S, Pezzoli F, Ravaioli M, Cescon M, Cucchetti A, Lauro A. Right hemicolectomy for colon cancer: a prospective randomised study comparing laparoscopic vs. open technique. Chir Ital. 2008;60:1-7. [PubMed] |
| 21. | Khan JS, Hemandas AK, Flashman KG, Senapati A, O’Leary D, Parvaiz A. Clinical outcome of laparoscopic and open colectomy for right colonic carcinoma. Ann R Coll Surg Engl. 2011;93:603-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM; COlon cancer Laparoscopic or Open Resection Study Group (COLOR). Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. |
| 23. | Lohsiriwat V, Lohsiriwat D, Chinswangwatanakul V, Akaraviputh T, Lert-Akyamanee N. Comparison of short-term outcomes between laparoscopically-assisted vs. transverse-incision open right hemicolectomy for right-sided colon cancer: a retrospective study. World J Surg Oncol. 2007;5:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [PubMed] |
| 25. | Abdel-Halim MR, Moore HM, Cohen P, Dawson P, Buchanan GN. Impact of laparoscopic right hemicolectomy for colon cancer. Ann R Coll Surg Engl. 2010;92:211-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Zhao LY, Liu H, Wang YN, Deng HJ, Xue Q, Li GX. Techniques and feasibility of laparoscopic extended right hemicolectomy with D3 lymphadenectomy. World J Gastroenterol. 2014;20:10531-10536. [PubMed] |
| 27. | Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the Learning Curve in Laparoscopic Colorectal surgery. Ann Surg. 2005;222:83-91. [RCA] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 601] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 28. | Guerrieri M, Campagnacci R, De Sanctis A, Lezoche G, Massucco P, Summa M, Gesuita R, Capussotti L, Spinoglio G, Lezoche E. Laparoscopic versus open colectomy for TNM stage III colon cancer: results of a prospective multicenter study in Italy. Surg Today. 2012;42:1071-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Reza MM, Blasco JA, Andradas E, Cantero R, Mayol J. Systematic review of laparoscopic versus open surgery for colorectal cancer. Br J Surg. 2006;93:921-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 257] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 30. | Han DP, Lu AG, Feng H, Wang PX, Cao QF, Zong YP, Feng B, Zheng MH. Long-term results of laparoscopy-assisted radical right hemicolectomy with D3 lymphadenectomy: clinical analysis with 177 cases. Int J Colorectal Dis. 2013;28:623-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 31. | Feroci F, Lenzi E, Garzi A, Vannucchi A, Cantafio S, Scatizzi M. Intracorporeal versus extracorporeal anastomosis after laparoscopic right hemicolectomy for cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2013;28:1177-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 32. | Fabozzi M, Allieta R, Brachet Contul R, Grivon M, Millo P, Lale-Murix E, Nardi M. Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc. 2010;24:2085-2091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 33. | Roscio F, Bertoglio C, De Luca A, Frattini P, Scandroglio I. Totally laparoscopic versus laparoscopic assisted right colectomy for cancer. Int J Surg. 2012;10:290-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 34. | Iorio T, Blumberg D. Totally intracorporeal laparoscopic colectomy (TILC) is associated with similar surgical outcomes in high and low operative risk patients. Surg Laparosc Endosc Percutan Tech. 2013;23:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Scatizzi M, Kröning KC, Borrelli A, Andan G, Lenzi E, Feroci F. Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg. 2010;34:2902-2908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 36. | Hellan M, Anderson C, Pigazzi A. Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS. 2009;13:312-317. [PubMed] |
| 37. | Chaves JA, Idoate CP, Fons JB, Oliver MB, Rodríguez NP, Delgado AB, Lizoain JL. [A case-control study of extracorporeal versus intracorporeal anastomosis in patients subjected to right laparoscopic hemicolectomy]. Cir Esp. 2011;89:24-30. [PubMed] |
| 38. | Grams J, Tong W, Greenstein AJ, Salky B. Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc. 2010;24:1886-1891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 105] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 39. | Tarta C, Bishawi M, Bergamaschi R. Intracorporeal ileocolic anastomosis: a review. Tech Coloproctol. 2013;17:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 40. | Choy PY, Bissett IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. 2011;7:CD004320. |
| 41. | Tanis E, van Geloven AA, Bemelman WA, Wind J. A comparison of short-term outcome after laparoscopic, transverse, and midline right-sided colectomy. Int J Colorectal Dis. 2012;27:797-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Santoro A, Boselli C, Renzi C, Gubbiotti F, Grassi V, Di Rocco G, Cirocchi R, Redler A. Transverse skin crease versus vertical midline incision versus laparoscopy for right hemicolectomy: a systematic review--current status of right hemicolectomy. Biomed Res Int. 2014;2014:643685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 43. | Lee KH, Ho J, Akmal Y, Nelson R, Pigazzi A. Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc. 2013;27:1986-1990. |
| 44. | Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008;10:823-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 405] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 45. | Park Y, Yong YG, Yun SH, Jung KU, Huh JW, Cho YB, Kim HC, Lee WY, Chun HK. Learning curves for single incision and conventional laparoscopic right hemicolectomy: a multidimensional analysis. Ann Surg Treat Res. 2015;88:269-275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 46. | Yun JA, Yun SH, Park YA, Huh JW, Cho YB, Kim HC, Lee WY. Oncologic Outcomes of Single-incision Laparoscopic Surgery Compared With Conventional Laparoscopy for Colon Cancer. Ann Surg. 2016;263:973-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 47. | Vettoretto N, Cirocchi R, Randolph J, Parisi A, Farinella E, Romano G. Single incision laparoscopic right colectomy: a systematic review and meta-analysis. Colorectal Dis. 2014;16:O123-O132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 48. | Poon JT, Cheung CW, Fan JK, Lo OS, Law WL. Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc. 2012;26:2729-2734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 153] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 49. | Pascual M, Salvans S, Pera M. Laparoscopic colorectal surgery: Current status and implementation of the latest technological innovations. World J Gastroenterol. 2016;22:704-717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 76] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 50. | Yang TX, Chua TC. Single-incision laparoscopic colectomy versus conventional multiport laparoscopic colectomy: a meta-analysis of comparative studies. Int J Colorectal Dis. 2013;28:89-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 51. | Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99:1219-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 270] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 52. | Morpurgo E, Contardo T, Molaro R, Zerbinati A, Orsini C, D’Annibale A. Robotic-assisted intracorporeal anastomosis versus extracorporeal anastomosis in laparoscopic right hemicolectomy for cancer: a case control study. J Laparoendosc Adv Surg Tech A. 2013;23:414-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 53. | Xu H, Li J, Sun Y, Li Z, Zhen Y, Wang B, Xu Z. Robotic versus laparoscopic right colectomy: a meta-analysis. World J Surg Oncol. 2014;12:274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 54. | Guerrieri M, Organetti L, Baldarelli M, Romiti C, Campagnacci R. Laparoscopic colectomy is a reliable option for colon cancer treatment. Ann Ital Chir. 2012;83:239-244. [PubMed] |
| 55. | Erguner I, Aytac E, Baca B, Hamzaoglu I, Karahasanoglu T. Total laparoscopic approach for the treatment of right colon cancer: a technical critique. Asian J Surg. 2013;36:58-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 56. | Juo YY, Agarwal S, Luka S, Satey S, Obias V. Single-Incision Robotic Colectomy (SIRC) case series: initial experience at a single center. Surg Endosc. 2015;29:1976-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 57. | Li JC, Leung KL, Ng SS, Liu SY, Lee JF, Hon SS. Laparoscopic-assisted versus open resection of right-sided colonic cancer--a prospective randomized controlled trial. Int J Colorectal Dis. 2012;27:95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |