Published online Aug 27, 2016. doi: 10.4240/wjgs.v8.i8.545
Peer-review started: March 26, 2016
First decision: April 19, 2016
Revised: April 30, 2016
Accepted: May 17, 2016
Article in press: May 27, 2016
Published online: August 27, 2016
Processing time: 153 Days and 8.2 Hours
Gastric outlet obstruction (GOO) is a common problem associated with advanced malignancies of the upper gastrointestinal tract. Palliative treatment of patients’ symptoms who present with GOO is an important aspect of their care. Surgical palliation of malignancy is defined as a procedure performed with the intention of relieving symptoms caused by an advanced malignancy or improving quality of life. Palliative treatment for GOO includes operative (open and laparoscopic gastrojejunostomy) and non-operative (endoscopic stenting) options. The performance status and medical condition of the patient, the extent of the cancer, the patients prognosis, the availability of a curative procedure, the natural history of symptoms of the disease (primary and secondary), the durability of the procedure, and the quality of life and life expectancy of the patient should always be considered when choosing treatment for any patient with advanced malignancy. Gastrojejunostomy appears to be associated with better long term symptom relief while stenting appears to be associated with lower immediate procedure related morbidity.
Core tip: Gastric outlet obstruction (GOO) is a common problem associated with advanced malignancies of the upper gastrointestinal tract. Palliative treatment of patients’ symptoms who present with GOO is an important aspect of their care. Surgical palliation of malignancy is defined as a procedure performed with the intention of relieving symptoms caused by an advanced malignancy or improving quality of life. Palliative treatment for GOO includes operative (open and laparoscopic gastrojejunostomy) and non-operative (endoscopic stenting) options. Regardless of the treatment used for relief of symptoms all physicians having end of life conversations with patients should be adequately trained in end of life care to ensure that patients are getting the optimal treatment for their particular circumstances.
- Citation: Potz BA, Miner TJ. Surgical palliation of gastric outlet obstruction in advanced malignancy. World J Gastrointest Surg 2016; 8(8): 545-555
- URL: https://www.wjgnet.com/1948-9366/full/v8/i8/545.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i8.545
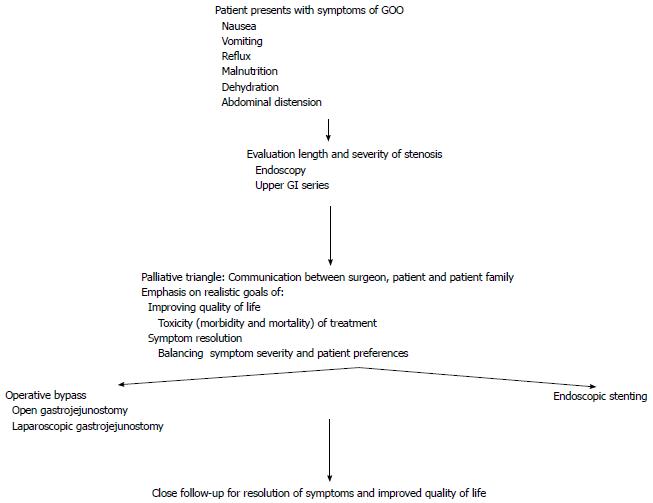
Gastric outlet obstruction (GOO) is a common problem associated with advanced malignancies of the upper gastrointestinal tract. Symptoms can be severe and include nausea, vomiting, malnutrition and decreased quality of life. Due to the advanced stages of the underlying malignancies causing these symptoms many patients are not candidates for curative resection. However, palliative treatment of their symptoms is an important aspect of their care. Research has shown that symptoms of advanced gastric cancer can often be effectively managed with palliative interventions. One of the main symptoms of advanced gastric cancer is GOO. Treatment for GOO includes operative and non-operative options. Traditionally, open gastrojejunostomy was the treatment modality of choice to bypass the obstruction. However, in recent years endoscopic stenting has been used more frequently. While stenting is considered less invasive and associated with a quicker return to oral intake, it is associated with several disadvantages including a high rate of re-obstruction and stent migration[1]. In this review, we discuss the incidence and presentation of GOO, the current data regarding the goals of palliative intervention, the success of palliative treatment of gastric cancer, the techniques used to treat GOO and the outcomes of those treatments (Figure 1).
GOO is a common complication of both benign and malignant disease of the stomach, pancreas and duodenum. It is caused by occlusion of the lumen by intrinsic or extrinsic growth[2]. Because up to 55% of gastric cancers and up to 75% of periampullary cancers are not resectable at the time of diagnosis, they represent the most common causes of malignant gastroduodenal obstruction[1,3]. GOO can also be caused by lymphoma, biliary disease, metastasis to the duodenum or jejunum and extrinsic compression[1,3]. Malignant gastroduodenal obstruction is associated with limited length of patient survival. Patients, on average, live 3-6 mo[3-7]. Malignant obstruction is a serious problem for physicians to treat because it is associated with a marked reduction in quality of life in a group of patients who are already significantly medically compromised[4]. In the setting of patients suffering from GOO, palliative interventions are often necessary to alleviate symptoms and improve quality of life[5].
The stomach has a significant capacity to distend allowing GOO to go unnoticed by the patient until high grade obstruction develops[4]. The symptoms of GOO are often incorrectly ascribed to the patient’s cancer or the therapies they are undergoing (including chemotherapy, radiation therapy or both). However, the diagnosis of GOO can be made by obtaining a good history of present illness from the patient. Patients present with symptoms of nausea, vomiting, malnutrition, reflux, abdominal distension and dehydration[3]. Patients often present with vomiting undigested food hours after eating and the vomit is often described as bilious[4]. As a result, these patients can develop “food fear” secondary to their debilitating emesis[3]. Patients also describe a reduced quality of life, poor condition and poor performance status[6]. Evaluation of patients who present with symptoms of GOO may require endoscopy and upper gastrointestinal series to evaluate severity and length of the stenosis. Because of the potential of an associated biliary obstruction, it is also important that the biliary system is evaluated prior to any surgical procedure. This workup can include a liver function panel, a right upper quadrant ultrasound, or a computed tomography scan with a “pancreas protocol”.
Substantial variation in the definition of palliative care has complicated the understanding of the role of palliative operations[7]. The concept of “palliation” is often used by physicians to describe: (1) a patient with limited survival; (2) procedures performed in the presence of unresectable disease; or (3) as acknowledgment that a curative procedure is not an option[7]. This suboptimal characterization of “palliation” has perpetuated imprecise interpretations of both palliative surgical indications and outcomes[7]. In an attempt to standardize the role of palliative care, the World Health Organization has defined palliative care as “the total active care of patients whose disease is not responsive to curative treatment. Control of pain, of other symptoms, and of psychological, social, and spiritual problems is paramount. The goal of palliative care is the achievement of the best quality of life for patients and their families”[7,8]. While these broad definitions of palliative care do provide a global understanding, they do not definitively explain the diverse goals of surgical palliation. For example, compare and contrast the patient who presents to the emergency room for an emergent laparotomy for a hemorrhagic tumor and the patient who presents to for an elective surgical biopsy to confirm advanced disease. The intent of these procedures is so dissimilar that it makes any meaningful evaluation of critical outcome measures imprecise[7]. Even if one considers only those patients with known metastatic disease, they still present with such different clinical scenarios requiring surgery that it makes valid comparisons of outcomes difficult[7]. In every case, ideal palliative care must emphasize the individual’s specific values and needs and therefore, different indications and outcomes can be observed for essentially identical procedures[7].
The best way to define surgical palliation of malignancy is as a procedure used with the primary intention of relieving symptoms caused by advanced malignancy or improving quality of life[7,9-12]. It is important to note that a palliative procedure is not the opposite of curative procedure. Instead, each procedure has its own distinct goals and indications and need to be considered separately and independently. The performance status and medical condition of the patient, the extent of the cancer, the patients prognosis, the availability of a curative procedure, the natural history of symptoms of the disease (primary and secondary), the durability of the procedure, and the quality of life and life expectancy of the patient should always be considered when choosing treatment for any patient with advanced malignancy[7,13]. The emphasis of palliative decision making should be placed on outcomes that can be realistically delivered with the goal of providing the patient with a good quality of life and symptom resolution[10].
In order to successfully provide symptom relief at the end of life while also minimizing operative morbidity and mortality, careful patient selection is of critical importance[14]. Appropriate decision making is enabled through effective interactions among the surgeon, the patient, and their family members via a dynamic relationship described by the palliative triangle[9,10,15]. This relationship allows the patients values, complaints, and social support to be considered against known surgical and medical alternatives[16]. Through this triangle emphasis should be placed on outcomes that can realistically be delivered to the patient with the goal of providing: (1) symptom resolution; (2) a good quality of life; (3) technically superior palliative operations; (4) dignity; and (5) compassion. The dynamics of the palliative triangle help to moderate the different beliefs of each of its members and to guide the decision making to the best treatment for individual patient[9,10,15]. Brown University studied the outcomes of patients with advanced malignancy that was managed by surgeons with the palliative triangle method. Patient reported symptom resolution or improvement after palliative intervention was noted in 117 of 129 procedures (90.7%) and this symptom relief occurred within 30 d after the operation. Palliative procedures were associated with 30 d postoperative mortality (3.9%) and morbidity (20.1%). Median survival was 212 d. The study suggests that palliative operations performed on patients selected using the palliative triangle approach have high rates of symptom improvement and low morbidity and mortality[10]. It is important to note that in this study, either one or two meetings between the surgeon, the patient and family lasting 60-90 min occurred before consensus was achieved on the appropriate palliative intervention. This fact highlights the complexity of the decision making involved when performing palliative procedures and the importance of understanding the core concepts of the palliative triangle[10].
Excellent communication between patients, family and providers is essential to successful palliation whether surgery is performed or is not even offered[10]. Effective communication between the patient and their doctor allows clinical problems to be identified more accurately, increases patient satisfaction with their care, improves patient compliance with treatment plans, alleviates feelings of distress and vulnerability by the patient and improves the patients overall well-being[10]. At the end of life, patients and families are particularly vulnerable and they seek well developed interpersonal silks and communication from their physicians to guide them[10].
Patients with gastric cancer often present with an advanced stage and have a low cure rate, therefore palliative strategies are an essential and necessary component of gastric cancer management. Surgical palliation may include resection or bypass with or without endoscopic or percutaneous interventions. These interventions serve to eliminate potential complications (pain, obstruction, bleeding, debilitating ascites, perforation) and improve symptom control caused by the primary tumor[7,17].
Research suggests that there may be a surgical benefit after palliative resection for patients with advanced gastric cancer[18-20]. Keränen et al[21] compared the safety, efficacy, and outcome of palliative stenting, palliative resection and gastrojejunostomy in patients with primary gastric cancer complicated by GOO. They concluded that palliative resection provides a surgical benefit and should be considered in patients suitable for surgery[21]. A study from Memorial Sloan Kettering Cancer Center evaluated the outcomes of patients who underwent noncurative gastric resection with either palliative or nonpalliative intent[7]. Three hundred and seven patients received a noncurative gastric resection between 1985 and 2001. Palliative operations were performed in 48% (147/307) and nonpalliative operations were performed in 52% (160/307) of patients[7]. There was no difference in mean length of hospital stay [palliative (16.9 d) vs nonpalliative (18.9 d)], morbidity (54%) or mortality (6%) between the two groups[7]. However, high-grade complications were less common in palliative [22% (32 of 147)] cases than in nonpalliative cases [29% (47 of 160), P = 0.049][7]. Additional palliative procedures were required in 24% (72 of 307) of patients, but their distribution was equal between the two groups[7]. Interestingly, many of the indications for repeat surgery were for treatment of distant disease and not for symptoms caused by the primary tumor. In both the palliative and nonpalliative groups, carcinomatisis caused gastrointestinal obstruction which required an intervention (either internal bypass, small bowel resection or colostomy) at similar rates[7]. This study suggests that complication rates associated with noncurative procedures performed with palliative intent are lower than those performed with nonpalliative intent. Similarly, Saidi et al[22] examined the role of palliative gastrectomy for patients with metastatic gastric cancer and evaluated its impact on survival. The study concludes that palliative gastrectomy with systemic therapy may improve survival in patients with stage IV gastric cancer[22]. However, further research would need to be done to compare palliative gastrectomy plus systemic therapy to systemic therapy alone. Finally, Zhang et al[23] attempted to summarize the outcome of patients undergoing palliative total gastrectomy for stage IV proximal gastric cancer. Between 1991 and 2005, clinical data of 197 patients undergoing palliative gastrectomy, 642 patients undergoing curative total gastrectomy, 102 patients undergoing explorative laparotomy, 78 patients undergoing jejunostomy and 152 nonsurgical patients, were enrolled. One-, three-, and five-year survival rates were significantly lower in the palliative gastrectomy group compared to the curative gastrectomy group[23]. Interestingly, the median survival time in the palliative gastrectomy group was significantly longer than that in the laparotomy, jejunostomy and the no surgery. The postoperative mortality and complication rate were significantly higher in the palliative gastrectomy group compared to the curative gastrectomy group[23]. The study concluded that palliative total gastrectomy for stage IV proximal gastric cancer is associated with prolonged survival time and decreased post-operative complications when compared to no surgery, laparotomy and jejunostomy procedures[23]. The improvement in survival seen in the above studies may be due to the reduction in overall tumor burden[24]. Together, this suggests that there may be a surgical benefit after palliative resection for patients with advanced gastric cancer.
Research regarding surgical treatment for advanced gastric cancer highlights the importance of appropriate patient selection. Samarasam et al[25] retrospectively reviewed patients from 1999 to 2003 who underwent palliative surgery for gastric adenocarcinoma. One hundred and seven/one hundred and fifty-one (70.9%) underwent either subtotal gastrectomy (SG) or total gastrectomy (TG) to macroscopic free margins; the remaining 44/151 underwent laparotomy with or without gastrojejunostomy. All patients received adjuvant chemotherapy[25]. Median survival was improved in resected patients (24 mo vs 12 mo, P = 0.0003); however the survival benefit decreased when a patient had more than one criteria for unresectability (T+, H+, P+, N+)[25]. Median survival was similar between SG and TG groups (24 mo and 20 mo, respectively)[25]. This study suggests that patients with more than one criteria for unresectability may do better with less invasive procedures. Zhang et al[23] compared the clinicopathological factors and outcomes of palliative gastrectomy to exploratory laparotomy with or without bypass for noncurative gastric cancer[26]. From 1988 to 2008, 365 patients underwent palliative gastrectomy and 151 patients underwent exploratory laparotomy or gastrojejunostomy for noncurative gastric cancer. One hundred and eighty-two of the patients were aged 70 years old and younger (group A) and 183 of the patients were older than 70 years old (group B). The overall survival of patients who underwent resection was 10.2 mo which was significantly longer than those patients who did not undergo resection (4.48 mo). Patients in the younger group (group A) were more likely to be female and had more aggressive tumors. Interestingly, the surgical morbidity was higher in both groups if the patients had comorbidities and the surgical morbidity and mortality was significantly higher in patients in the older age group (group B)[26]. This data once again highlights the critical importance of appropriate patient selection and the terms of the palliative triangle.
While postoperative morbidity and mortality are important outcomes to consider for any surgical intervention the goals of palliative care emphasize quality of life and symptom relief. To better evaluate these important outcomes, one group performed a partitioned survival analysis, which assessed the state of health in relation to the patient’s treatment, the treatment toxicity, and any patient relapse over time[24,27]. Patient health state was defined in terms of “time without symptoms or toxicity” or (TWiST). Three hundred and seven non-curative resections were included in the analysis and 147 (48%) of them were performed with palliative intent. In the palliative group patients experienced an average of 8.5 mo in the TWiST state. Complications that reduced the time spent in TWiST included high-grade complications such as ICU admission, unplanned re-intervention, or permanent disability (2.1 mo, P = 0.04). Patients who presented with multiple sites of metastasis trended towards less time in the TWiST state (4.9 mo, P = 0.08). This data demonstrates the importance of appropriate patient selection. Pre-operative counseling between the surgeon, the patient and the family is critical in determining treatment goals and appropriate follow-up is necessary to ensure appropriate outcomes.
Understanding the anatomy of the stomach and small bowel in patients who have symptoms of GOO is an important aspect of choosing the right intervention.
Gastrojejunostomies can be performed in an antecolic or retrocolic fashion. The antecolic technique connects the distal stomach to the jejunum. The retrocolic technique involves placement of the jejunal loop through the transverse colon mesentery[28].
An incision is made in the upper midline of the abdomen. In an antecolic gastrojejunostomy the surgeon must identify a section of the distal stomach and a loop of jejunum distal to the ligament of Treitz that can be easily brought in close proximity to the stomach. Usually a location 15-20 cm distal to the ligament of Treitz is chosen. Care must be taken to identify the proximal jejunum when making a gastrojejunostomy, because anastomosing the ilium to the stomach is a rare complication associated with high morbidity. A posterior row of silk sutures is placed to connect the stomach and jejunum. Electro cautery is then used to open the jejunum and the stomach creating jejunal and gastric stomas respectively. The inner layer of the anastomosis is performed using a running full thickness absorbable suture which is carried anteriorly. Interrupted silk sutures are then placed to complete the anterior portion of the two layer gastrojejunostomy[28].
A stapled anastomosis can also be performed in which case the enterotomy and gastrotomy are performed as described above to facilitate placement of the stapler. The opening should be large enough to allow entry of the staple device. The gastrointestinal anastomosis (GIA) stapling device is placed through the holes created in the stomach and the jejunal and the anastomosis is performed by firing the stapler. The enterotomy and gastroenterotomy are then closed together using a transanastomotic (TA) stapling device[28].
If a retrocolic gastrojejunostomy is performed, the first step is again to identify the sites for the anastomosis of the stomach and jejunum. The transverse colon is lifted cephalad to visualize the mesentery and identify an avascular area through which the jejunal loop can pass through. A hand sewn anastomosis is performed in the same fashion described above for the antecolic approach using a two layer anastomosis with a posterior row of silk interrupted sutures. The jejunal and gastric stomas are created using electro cautery. The inner layer of the anastomosis is accomplished with a running full thickness absorbable suture. The retrocolic gastrojejunostomy is then completed using interrupted silk seromuscular sutures placed anteriorly[28].
Similar techniques are used to perform the stapled anastomosis for a retrocolic gastrojejunostomy. The jejunal and gastric stomas are created using electro cautery. The retrocolic gastrojejunostomy is then completed using the GIA stapler and the openings created in the stomach and jejunum are closed together using a TA stapler. If a retrocolic approach is used most surgeons will loosely suture the edges of the mesentery to the jejunum to minimize the risk of herniation of the bowel loop[28].
The midline incision is closed in the usual fashion regardless of whether an antecolic or retrocolic approach was used. A nasogastric tube is usually maintained postoperatively on suction until bowel function returns and a diet can be initiated[28].
Understanding the anatomy of the stomach, liver, ligament of Treitz and esophagus are important details for the surgeon to understand before performing a laparoscopic gastrojejunostomy[29]. It is necessary to identify the presence of hepatomegaly because a large left lateral segment may mean that the falciform ligament will need to be divided for optimal hepatic retraction and visualization[29]. Again, accurate identification of the ligament of Treitz is imperative to ensure localization of the jejunum[29].
Prior to surgery the patient is usually asked to undergo bowel preparation. After induction of anesthesia, a nasogastric tube (18 gauge) is placed to decompress the stomach. This will also be used during the creation of the gastrojejunostomy anastomosis and as an intraluminal stent to ensure patency of the newly created gastro-jejunal lumen. A urinary catheter is also placed to decompress the bladder.
The patient is placed in the supine position on the operating table. The arms are extended on arm boards and foot plates and safety straps are placed to secure positioning. The surgeon stands on the patient’s right side while the assistant surgeon and camera operator are on the left side[29]. The authors recommend an open Hassan technique to access the abdomen. A long 45 degree, 10 mm endoscope allows for optical visualization of the operative anatomy[29]. Five ports are placed as follows: (1) one to the left of midline below the sternum to be used for liver retraction (an expandable liver paddle is used to bluntly retract the left lobe of the liver); (2) one to the right of midline to be used for the instrument in the surgeons left hand; (3) one to the right of the umbilicus for the instrument to be used in the surgeon’s right hand; (4) one to the left of the umbilicus to be used for the camera; and (5) one in the left lower quadrant to be used for the instrument in the assistant’s right hand[30]. Laparoscopic gastrojejunostomy can be performed with a stapler or with a hand sewn technique.
For the hand sewn technique a needle driver for suturing and a left handed instrument, either blunt grasper or curved tip grasper, will be needed. To begin the construction of the gastrojejunostomy the left lobe of the liver must be fully retracted. To facilitate this, a nathanson retractor is placed in the epigastrium to elevate the liver and expose the gastro esophageal fat pat which is used to identify the gastro esophageal junction[29,30]. The proximal end of the jejunal limb is carefully identified and brought into the upper abdomen (usually in an antecolic, antegastric manner). A running back wall suture line is created using a 2-0 Vicryl suture (approximately 20 cm in length). Two enterotomies are made, one in the stomach and one in the jejunal limb, about 1.5 cm in length and a few millimeters away from the running back wall suture line[30]. The suture is run from the patients left side corner to the right corner and the remaining suture and needle are saved. A second, inner running suture line is created using a 2-0 Vicryl which is started at the patients left side corner of the open enterotomy. Another 2-0 Vicryl suture is used to close the inner layer anteriorly. Prior to completion of the inner layer closure, a 34 French nasogastric (NG) or orogastric (OG) tube is passed across the anastomosis under direct visualization. The inner layer closure is completed by bringing the two sutures onto the anterior aspect of the anastomosis and tying them together. Needles are cut and removed. The previous outer layer Vicryl suture is then used to continue anteriorly to reinforce the inner layer. This can also be completed by starting a separate second suture beginning from the corner and tying in the middle of the anterior aspect gastrojejunostomy[30].
A leak test is then performed. The patient is placed in the Trendelenburg position and the left upper quadrant is filled with normal saline to immerse the anastomosis[30]. Air is introduced into NG tube until adequate inflation of the stomach and jejunal anastomosis is observed. A leak test can also be performed with methylene blue through the NG tube. If leakage is noticed the area is repaired with additional non absorbable sutures until no further lair leak is seen[30].
There are several of important techniques that should be used when performing a gastrojejunostomy to minimize postoperative complications. To minimize anastomotic ulcer and stricture formation, the inner layer is closed using absorbable sutures[30]. The aperture of the anastomosis is regulated by closing the enterotomy defect over an NG or OG tube. Care must be taken to avoid suturing to the tube which can result in disruption of the closure[30]. Back-hand suturing in the corners may allow more precise suturing if forehand stitching appears awkward in orientation[30]. The tension on the running suture is maintained by the assistant throughout the closure process to avoid loosening of the closure and allowing potential leakage. Prior to tying the knots the entire suture must be cinched down to further eliminate potential gaps[30].
A laparoscopic gastrojejunostomy can also be performed with stapling devices. First, the posterior wall of the stomach is cleared of adhesions and any vascular tissue with a Ligasure device. In preparation for a retrogastric anastomosis a gastrostomy is created and marked with a silk suture. An enterotomy is created in a carefully selected potion of the jejunum. A 30-mm long endoscopic gastrointestinal stapler is used to create a gastrojejunostomy by firing it across the common walls of the stomach and the jejunum for approximately 2 cm in length. Following stapling, anesthesia advances the NG tube under direct vision across the gastrojejunostomy[29]. The gastrojejunostomy is closed over the NG tube with a running 2.0 silk suture. This layer is carefully inspected to look for any gaps in the suture line. A second layer of 2-0 silk is paced circumferentially around the entire anastomosis. The gastrojejunostomy is tested for a leak and reinforced as appropriate. The NG tube must be advanced forward and pulled back to ensure that is has not been caught by on the sutures. The trocars are removed under direct visualization and the pneumoperitonium is released.
For both the hand sewn and stapling technique a suction drain may be left in the vicinity of the anastomosis for postoperative management. 3-0 absorbable suture is used for the subcuticular port site closure[29]. Post operatively a nasogastric tube is usually maintained on suction until bowel function returns and a diet can be initiated[29].
It is important that the gastrointestinal stent morphology adapt to the anatomic curvature of the intestine to achieve appropriate function[1]. There are currently two FDA approved duodenal stents and they include the Wallstent Enteral and the Wallflex Enteral duodenal Stent. The Wallstent Enteral from Boston Scientific is made from Cobalt-based alloy. It is uncovered and has a deployment diameter of 20-22 mm and a 40%-50% degree of shortening. The Wallstent Enteral features through the scope delivery and reconstrainability. The Wallflex Enteralduodenal Stent from Boston Scientific is made of Nitinol. It is uncovered and had a deployment diameter of 22 mm and a 30%-40% degree of shortening. The Wallflex Enteralduodenal Stent features proximal flaring, through the scope delivery and reconstrainability. These stents are self-expandable metal stents (SEMS)[31]. They are both uncovered meaning that they embed into the stricture and surrounding tissue and can be placed through the working channel of a therapeutic endoscope. Uncovered SEMS are non-removable and migrate less often but tumor ingrowth frequently occurs causing a high rate of reobstruction[31]. New stents are being developed with higher flexibility, less foreshortening and covers with the goal of reducing stent migration and tumor ingrowth. So far these stents have been found to be comparable to existing stents and may have a lower frequency of complications including decreased migration and tumor ingrowth[4,32-36]. Other drug eluting or radioactive stents to help slow tumor growth are being developed but are currently not yet available.
Associated with GOO is sometimes so tight that it is difficult, if not impossible, to traverse the stricture with the therapeutic endoscope (the working channel of the scope needs to be greater than 3.8 mm)[31]. In order to minimize risk of perforation, physicians should avoid attempting to aggressively dilate the stricture[31]. However, patients with malignant duodenal obstruction are at a high risk for biliary obstruction. Therefore placing a biliary SEMS prophylactically before placing the duodenal SEMS should be considered. Duodenal strictures are dilated (18-22 mm) only if biliary drainage is to be performed, because access to the papilla requires the use of a large diameter therapeutic duodenoscope[31]. If, after assessing the status of the biliary tree, there is known or impending biliary obstruction an expandable metal biliary stent should be placed before the duodenal stent. To treat biliary obstruction after placement of a duodenal stent, a percutaneous transhepatic approach is usually required. Stenting of both the duodenum and the bile duct is the non-surgical equivalent of traditional double surgical bypass (gastrojejunosmy and choledochojejunostomy)[31]. Due to these potential complications, duodenal stents generally are not used for benign disease only malignant disease.
Patients with GOO have high gastric residuals and suction of gastric contents should be performed prior to beginning the procedure to minimize aspiration risk and optimize visualization[31]. If a patient is determined to be at high risk for aspiration then endotracheal intubation should be initiated prior to stent placement. The procedure should be performed under fluoroscopic or endoscopic guidance. Research suggests that the use of both modalities is important provide adequate visualization and get an idea of any distal obstruction[3,37]. Patients should be in the supine or prone position to optimize fluoroscopic visualization. As mentioned above, the status of the biliary tree should always be assessed before gastro duodenal stent placement. Placement of the SEMS across the papilla will make endoscopic biliary access difficult. If the tumor is located in the proximal duodenum without involvement of the papilla a stent that is long enough to cross the lesion should be chosen but not excessively long which will prevent access to the papilla[31]. Therefore, accurate assessment of the length and location of the malignant stricture is important[31]. The stricture may be accessed with a standard biliary balloon catheter over a guide wire under fluoroscopic guidance. Injecting dye through the stricture may help delineate the length, geometry and extension of the structure. The selected stent should be about 4 cm longer than the stricture. Prior to patient discharge patients should be advanced to liquids and then to solids as tolerated. They should be told to avoid leafy vegetables which may result in stent occlusion.
Operative treatment options for GOO include NG placement, percutaneous gastrojejunostomy and gastrojejunostomy (open and laparoscopic).
While nasogastric and jejunostomy tubes are minimally invasive they have several disadvantages. Nasogastric tubes and gastrostomy tubes are used for decompression however they cannot be used for feeding. In contrast, jejunostomy tubes can be placed distal to the obstruction so they can be used for hydration, enteral nutrition, and to provide medications[4]. However these patients remain obstructed in their stomach and they often still have symptoms of nausea and vomiting. Percutaneous gastrojejunostomy tubes provide decompression of the stomach and distal enteral feeding. However these tubes can result in peritoneal leakage especially in the setting of ascites[3]. The main disadvantage, however, of percutaneous tubes is the fact that patients are unable to resume oral feeding.
Surgical palliation is the standard treatment method for patients who present with symptoms of GOO[38]. Gastrojejunostomy has been shown to be highly successful at relieving obstructive symptoms and allowing patients to return to oral eating[4]. Research suggests that operative gastrojejunostomy may be preferable to endoscopic stent procedures due to its durability for providing symptom relief[6,39,40]. However, due to the poor general condition and advanced malnutrition of these patients, surgical palliation with gastrojejunostomy can be associated with a high complication rate[3,41]. The mortality rate associated with surgical bypass has been reported to be between 2%-36% and the complication rate to be between 13%-55%[3,7,42,43]. The mean hospital stay is 11 to 15 d with a range of 5-80 d[3,43,44]. Delayed gastric emptying is a common complication which has been reported to vary from 5 to 37 d[3,38,43,45,46]. Patients who undergo palliative surgical gastrojejunostomy have been reported to have survival times between 35-293 d[1,40,43-48]. The large range is likely due to the difference in the underlying extent of disease. There is no evidence to suggest a difference in mortality or survival between patients who undergo open surgical or endoscopic procedures[45,46].
Laparoscopic gastrojejunostomy is another option for the relief of the obstructive symptoms associated with GOO[49]. Laparoscopy is a less invasive procedure than open surgery. The hospital length of stay can be as low as 3 d and as high as 14 d[41,42,44,50,51]. Laparoscopic procedures are associated with decreased blood loss compared to open procedures[41,51]. However there is no research to suggest a difference in the amount of blood transfusion received[42]. It is unclear as to whether laparoscopic gastrojejunostomy is associated with a delay in gastric emptying[3,41]. Research shows no difference in mortality, operating time, or nonsteroidal and anti-inflammatory drug consumption between patients undergoing open vs laparoscopic bypass for GOO[41,42]. There is inconclusive evidence regarding the difference in opiate analgesia and operative morbidity between laparoscopic and open procedures[41,42]. The conversion to open surgery has been reported to range from 0% to 20%[42]. The presence of malignant ascites is a relative contraindication for laparoscopic surgery.
Nonoperative treatment options for the treatment of GOO include gastroduodenal stent placement. In the recent years there has been a decline in the number of patients undergoing surgical treatment of GOO because of the development of self-expanding metal stents[4]. Stents have been found to be safe and effective in terms of palliation of symptoms especially in those patients who are too high risk to undergo surgery. Patients who have previously undergone a surgical procedure who later develop GOO are also good candidates for stent placement. However, it should be noted that because of the low durability and high re-obstruction rates of duodenal stents they are often not used for benign disease. A large systemic review found that in 6076 patients with malignant GOO, 97% underwent successful stent placement and 89% had relieve of symptoms and improvement in oral intake[52]. Interestingly, patients who did not have relief of symptoms also suffered from side effects such as narcotic pain medication, anorexia or subsequent distal obstructive which may have been contributing to their symptoms[52]. Advantages of stent placement include the following: Less invasive, outpatient procedure, fewer complications, cost effective, rapid return to gastric emptying, shorter procedure time and improved quality of life[3,4,45,53-55]. Patients may resume oral intake as quickly as post-operative day 1-5 of the procedure[2-4,6,43,45,46]. It has been reported that 73%-87% of patients who have gastroduodenal stents placed resume oral food intake[1,47]. The mean hospital discharge rate is short and has been reported to be 2.5-7.5 d. Survival has been reported to range from 63-189 d[2,40,43,45-48]. Again, survival time is likely attributed to the advanced stages of the underlying disease.
Contraindications to stent placement include distal gastrointestinal obstruction, gastrointestinal perforation, and patients with multilevel bowel disease[3]. The immediate complication rate of the procedure is low and has been reported to be 4%[43]. However the rate of late adverse events has been found to be higher in patients who undergo stent placement compared to those who undergo gastrojejunostomy[40]. The major disadvantages of stent placement include a high rate of stent migration and re-obstruction[1,6,38,40]. Reobstruction rates have been found to occur more quickly than patients who undergo gastrojejunostomy[40]. Another devastating complication is the concomitant or subsequent development of biliary obstruction which has been reported in up to 44% of cases[4,56]. Other complications include bleeding and perforation[4]. Interestingly, one study looked at the effect of endoscopic vs surgical palliative procedures for symptom relief in patients with metastatic or advanced loco regional cancer. They found that patients who underwent endoscopic procedures had fewer perioperative complications {endoscopic [18% (37/209)] vs patients who underwent operative procedures [39% (205/522)], P < 0.001}. The patients in the endoscopic group experienced a higher 30-d mortality {endoscopic [15% (38/247)]} when compared to the operative group [9% (54/576), P = 0.017][11]. Therefore, stenting is likely more beneficial for patients with a short anticipated survival, while gastrojejunostomy may provide more durable symptom improvement.
Interestingly, one study compared the cost of stent placement and gastrojejunostomy for the treatment of malignant GOO. They found that food intake improved more rapidly after stent placement as opposed to after gastrojejunostomy. However, long term relief of obstructive symptoms was better after gastrojejunostomy. In addition they found that more major complications and more repeat interventions occurred after stent placement as opposed to after gastrojejunostomy. While the initial costs were higher for patients undergoing gastrojejunostomy there was no difference between the two procedures in follow-up costs. Total costs per patient were higher for gastrojejunostomy compared to stent placement. The incremental cost effectiveness ratio of the gastrojejunostomy compared to stent placement was 164 euros per extra day with gastric outlet obstruction scoring system adjusted for survival. They concluded that the medical effects were better after gastrojejunostomy despite the higher costs and that because the cost difference between the two groups was small that it should not play a role when deciding on the type of treatment to offer patients[39].
Palliative treatments are offered to patients with the intent of relieving the symptoms of GOO and ultimately improving patient quality of life. Decisions regarding the use of surgical verses endoscopic procedures for GOO require the highest level of surgical judgment. Physicians must consider the individual patients quality and expectancy of life, the prognosis of the disease, the availability and the success of each treatment option[9,14,15].
GOO can be effectively treated by both gastrojejunostomy and stenting. Gastrojejunostomy appears to be associated with better long term outcomes while stenting appears to be associated with better short term outcomes. New laparoscopic procedures and new technologies in endoscopic stents will likely continue to change the treatment recommendations for GOO. When it comes to palliative care, it is imperative that all physicians involved are adequately trained in end of life management to ensure that each patient gets the appropriate treatment for their particular circumstances.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Cleveland EM, Kassir R, Kopljar M S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Pinto Pabón IT, Díaz LP, Ruiz De Adana JC, López Herrero J. Gastric and duodenal stents: follow-up and complications. Cardiovasc Intervent Radiol. 2001;24:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Espinel J, Vivas S, Muñoz F, Jorquera F, Olcoz JL. Palliative treatment of malignant obstruction of gastric outlet using an endoscopically placed enteral Wallstent. Dig Dis Sci. 2001;46:2322-2324. [PubMed] |
| 3. | Lopera JE, Brazzini A, Gonzales A, Castaneda-Zuniga WR. Gastroduodenal stent placement: current status. Radiographics. 2004;24:1561-1573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 115] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Brimhall B, Adler DG. Enteral stents for malignant gastric outlet obstruction. Gastrointest Endosc Clin N Am. 2011;21:389-403, vii-viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Schmidt C, Gerdes H, Hawkins W, Zucker E, Zhou Q, Riedel E, Jaques D, Markowitz A, Coit D, Schattner M. A prospective observational study examining quality of life in patients with malignant gastric outlet obstruction. Am J Surg. 2009;198:92-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (38)] |
| 6. | Miyazaki Y, Takiguchi S, Takahashi T, Kurokawa Y, Makino T, Yamasaki M, Nakajima K, Mori M, Doki Y. Treatment of gastric outlet obstruction that results from unresectable gastric cancer: Current evidence. World J Gastrointest Endosc. 2016;8:165-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Miner TJ, Jaques DP, Karpeh MS, Brennan MF. Defining palliative surgery in patients receiving noncurative resections for gastric cancer. J Am Coll Surg. 2004;198:1013-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Cancer pain relief and palliative care. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1990;804:1-75. [PubMed] |
| 9. | Miner TJ. Communication skills in palliative surgery: skill and effort are key. Surg Clin North Am. 2011;91:355-366, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Miner TJ. Communication as a core skill of palliative surgical care. Anesthesiol Clin. 2012;30:47-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Miner TJ, Brennan MF, Jaques DP. A prospective, symptom related, outcomes analysis of 1022 palliative procedures for advanced cancer. Ann Surg. 2004;240:719-726; discussion 726-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 110] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Miner TJ, Jaques DP, Tavaf-Motamen H, Shriver CD. Decision making on surgical palliation based on patient outcome data. Am J Surg. 1999;177:150-154. [PubMed] |
| 13. | Forbes JF. Principles and potential of palliative surgery in patients with advanced cancer. Recent Results Cancer Res. 1988;108:134-142. [PubMed] |
| 14. | Miner TJ. Palliative surgery for advanced cancer: lessons learned in patient selection and outcome assessment. Am J Clin Oncol. 2005;28:411-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Miner TJ, Cohen J, Charpentier K, McPhillips J, Marvell L, Cioffi WG. The palliative triangle: improved patient selection and outcomes associated with palliative operations. Arch Surg. 2011;146:517-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Thomay AA, Jaques DP, Miner TJ. Surgical palliation: getting back to our roots. Surg Clin North Am. 2009;89:27-41, vii-viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Sugarbaker PH, Yonemura Y. Clinical pathway for the management of resectable gastric cancer with peritoneal seeding: best palliation with a ray of hope for cure. Oncology. 2000;58:96-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 118] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Chang YR, Han DS, Kong SH, Lee HJ, Kim SH, Kim WH, Yang HK. The value of palliative gastrectomy in gastric cancer with distant metastasis. Ann Surg Oncol. 2012;19:1231-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Hartgrink HH, Putter H, Klein Kranenbarg E, Bonenkamp JJ, van de Velde CJ. Value of palliative resection in gastric cancer. Br J Surg. 2002;89:1438-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 187] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 20. | Blakely AM, McPhillips J, Miner TJ. Surgical palliation for malignant disease requiring locoregional control. Ann Palliat Med. 2015;4:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Keränen I, Kylänpää L, Udd M, Louhimo J, Lepistö A, Halttunen J, Kokkola A. Gastric outlet obstruction in gastric cancer: a comparison of three palliative methods. J Surg Oncol. 2013;108:537-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Saidi RF, ReMine SG, Dudrick PS, Hanna NN. Is there a role for palliative gastrectomy in patients with stage IV gastric cancer? World J Surg. 2006;30:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Zhang JZ, Lu HS, Huang CM, Wu XY, Wang C, Guan GX, Zhen JW, Huang HG, Zhang XF. Outcome of palliative total gastrectomy for stage IV proximal gastric cancer. Am J Surg. 2011;202:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Blakely AM, Miner TJ. Surgical considerations in the treatment of gastric cancer. Gastroenterol Clin North Am. 2013;42:337-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 25. | Samarasam I, Chandran BS, Sitaram V, Perakath B, Nair A, Mathew G. Palliative gastrectomy in advanced gastric cancer: is it worthwhile? Anz J Surg. 2006;76:60-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Huang KH, Wu CW, Fang WL, Chen JH, Lo SS, Wang RF, Li AF. Palliative resection in noncurative gastric cancer patients. World J Surg. 2010;34:1015-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Miner TJ, Karpeh MS. Gastrectomy for gastric cancer: defining critical elements of patient selection and outcome assessment. Surg Oncol Clin N Am. 2004;13:455-466, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Lautz GGW, Lautz DB. Roux-en-Y gastric bypass (linear stapler). Atlas of Minimally Invasive Surgical Techniques. New York: Saunders an imprint of Elsevier Inc 2012; 251-263. |
| 29. | Mun E. Handsewn Gastrojejunal Anastomosis. Atlas of Minimally Invasive Surgical Techniques. New York: Saunders an imprint of Elsevier Inc 2012; 264-269. |
| 30. | Canard JM, Létard JC, Palazzo L, Penman I, Anne Marie Lennon AM. Interventional endoscopy. Gastrointestinal Endoscopy In Practice. New York: Elsevier Limited 2011; 155-263. |
| 31. | Maetani I, Isayama H, Mizumoto Y. Palliation in patients with malignant gastric outlet obstruction with a newly designed enteral stent: a multicenter study. Gastrointest Endosc. 2007;66:355-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Vakil N, Morris AI, Marcon N, Segalin A, Peracchia A, Bethge N, Zuccaro G, Bosco JJ, Jones WF. A prospective, randomized, controlled trial of covered expandable metal stents in the palliation of malignant esophageal obstruction at the gastroesophageal junction. Am J Gastroenterol. 2001;96:1791-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Vakil N, Morris AI, Marcon N, Segalin A, Peracchia A, Bethge N, Zuccaro G, Bosco JJ, Jones WF. A prospective, randomized, controlled trial of covered expandable metal stents in the palliation of malignant esophageal obstruction at the gastroesophageal junction. Am J Gastroenterol. 2001;96:1791-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Lee KM, Shin SJ, Hwang JC, Cheong JY, Yoo BM, Lee KJ, Hahm KB, Kim JH, Cho SW. Comparison of uncovered stent with covered stent for treatment of malignant colorectal obstruction. Gastrointest Endosc. 2007;66:931-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 35. | Kim CG, Choi IJ, Lee JY, Cho SJ, Park SR, Lee JH, Ryu KW, Kim YW, Park YI. Covered versus uncovered self-expandable metallic stents for palliation of malignant pyloric obstruction in gastric cancer patients: a randomized, prospective study. Gastrointest Endosc. 2010;72:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 36. | Maetani I, Mizumoto Y, Shigoka H, Omuta S, Saito M, Tokuhisa J, Morizane T. Placement of a triple-layered covered versus uncovered metallic stent for palliation of malignant gastric outlet obstruction: a multicenter randomized trial. Dig Endosc. 2014;26:192-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 37. | Topazian M, Ring E, Grendell J. Palliation of obstructing gastric cancer with steel mesh, self-expanding endoprostheses. Gastrointest Endosc. 1992;38:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 38. | Jeurnink SM, van Eijck CH, Steyerberg EW, Kuipers EJ, Siersema PD. Stent versus gastrojejunostomy for the palliation of gastric outlet obstruction: a systematic review. BMC Gastroenterol. 2007;7:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 250] [Cited by in RCA: 232] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 39. | Jeurnink SM, Polinder S, Steyerberg EW, Kuipers EJ, Siersema PD. Cost comparison of gastrojejunostomy versus duodenal stent placement for malignant gastric outlet obstruction. J Gastroenterol. 2010;45:537-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 40. | No JH, Kim SW, Lim CH, Kim JS, Cho YK, Park JM, Lee IS, Choi MG, Choi KY. Long-term outcome of palliative therapy for gastric outlet obstruction caused by unresectable gastric cancer in patients with good performance status: endoscopic stenting versus surgery. Gastrointest Endosc. 2013;78:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 90] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 41. | Navarra G, Musolino C, Venneri A, De Marco ML, Bartolotta M. Palliative antecolic isoperistaltic gastrojejunostomy: a randomized controlled trial comparing open and laparoscopic approaches. Surg Endosc. 2006;20:1831-1834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 42. | Al-Rashedy M, Dadibhai M, Shareif A, Khandelwal MI, Ballester P, Abid G, McCloy RF, Ammori BJ. Laparoscopic gastric bypass for gastric outlet obstruction is associated with smoother, faster recovery and shorter hospital stay compared with open surgery. J Hepatobiliary Pancreat Surg. 2005;12:474-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Espinel J, Sanz O, Vivas S, Jorquera F, Muñoz F, Olcoz JL, Pinedo E. Malignant gastrointestinal obstruction: endoscopic stenting versus surgical palliation. Surg Endosc. 2006;20:1083-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 44. | Wong YT, Brams DM, Munson L, Sanders L, Heiss F, Chase M, Birkett DH. Gastric outlet obstruction secondary to pancreatic cancer: surgical vs endoscopic palliation. Surg Endosc. 2002;16:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 123] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 45. | Maetani I, Akatsuka S, Ikeda M, Tada T, Ukita T, Nakamura Y, Nagao J, Sakai Y. Self-expandable metallic stent placement for palliation in gastric outlet obstructions caused by gastric cancer: a comparison with surgical gastrojejunostomy. J Gastroenterol. 2005;40:932-937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 46. | Jeurnink SM, Steyerberg EW, van Hooft JE, van Eijck CH, Schwartz MP, Vleggaar FP, Kuipers EJ, Siersema PD. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010;71:490-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 361] [Article Influence: 24.1] [Reference Citation Analysis (2)] |
| 47. | Johnsson E, Thune A, Liedman B. Palliation of malignant gastroduodenal obstruction with open surgical bypass or endoscopic stenting: clinical outcome and health economic evaluation. World J Surg. 2004;28:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 48. | Guo JJ, Liang WX, Zhang T. A prospective comparative study of three treatment options in patients with malignant gastric outlet obstruction. Zhonghua Weichang Waike Zazhi. 2010;13:598-600. [PubMed] |
| 49. | Nagy A, Brosseuk D, Hemming A, Scudamore C, Mamazza J. Laparoscopic gastroenterostomy for duodenal obstruction. Am J Surg. 1995;169:539-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7651] [Cited by in RCA: 3105] [Article Influence: 103.5] [Reference Citation Analysis (0)] |
| 50. | Mehta S, Hindmarsh A, Cheong E, Cockburn J, Saada J, Tighe R, Lewis MP, Rhodes M. Prospective randomized trial of laparoscopic gastrojejunostomy versus duodenal stenting for malignant gastric outflow obstruction. Surg Endosc. 2006;20:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 155] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 51. | Bergamaschi R, Mårvik R, Thoresen JE, Ystgaard B, Johnsen G, Myrvold HE. Open versus laparoscopic gastrojejunostomy for palliation in advanced pancreatic cancer. Surg Laparosc Endosc. 1998;8:92-96. [PubMed] |
| 52. | Dormann A, Meisner S, Verin N, Wenk Lang A. Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness. Endoscopy. 2004;36:543-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 290] [Article Influence: 13.8] [Reference Citation Analysis (1)] |
| 53. | Ly J, O’Grady G, Mittal A, Plank L, Windsor JA. A systematic review of methods to palliate malignant gastric outlet obstruction. Surg Endosc. 2010;24:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 122] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 54. | Yim HB, Jacobson BC, Saltzman JR, Johannes RS, Bounds BC, Lee JH, Shields SJ, Ruymann FW, Van Dam J, Carr-Locke DL. Clinical outcome of the use of enteral stents for palliation of patients with malignant upper GI obstruction. Gastrointest Endosc. 2001;53:329-332. [PubMed] |
| 55. | Zheng B, Wang X, Ma B, Tian J, Jiang L, Yang K. Endoscopic stenting versus gastrojejunostomy for palliation of malignant gastric outlet obstruction. Dig Endosc. 2012;24:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (3)] |
| 56. | Adler DG, Baron TH. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol. 2002;97:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |