Published online Jul 27, 2016. doi: 10.4240/wjgs.v8.i7.533
Peer-review started: October 21, 2015
First decision: December 28, 2015
Revised: April 2, 2016
Accepted: April 14, 2016
Article in press: April 18, 2016
Published online: July 27, 2016
Processing time: 265 Days and 18.2 Hours
AIM: To perform a systematic review focusing on short-term outcomes after colorectal surgery in patients with previous abdominal open surgery (PAOS).
METHODS: A broad literature search was performed with the terms “colorectal”, “colectomy”, “PAOS”, “previous surgery” and “PAOS”. Studies were included if their topic was laparoscopic colorectal surgery in patients with PAOS, whether descriptive or comparative. Endpoints of interest were conversion rates, inadvertent enterotomy and morbidity. Analysis of articles was made according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
RESULTS: From a total of 394 citations, 13 full-texts achieved selection criteria to be included in the study. Twelve of them compared patients with and without PAOS. All studies were retrospective and comparative and two were case-matched. The selected studies comprised a total of 5005 patients, 1865 with PAOS. Among the later, only 294 (16%) had history of a midline incision for previous gastrointestinal surgery. Conversion rates were significantly higher in 3 of 12 studies and inadvertent enterotomy during laparoscopy was more prevalent in 3 of 5 studies that disclosed this event. Morbidity was similar in the majority of studies. A quantitative analysis (meta-analysis) could not be performed due to heterogeneity of the studies.
CONCLUSION: Conversion rates were slightly higher in PAOS groups, although not statistical significant in most studies. History of PAOS did not implicate in higher morbidity rates.
Core tip: So far, there is no substantial evidence in the literature to recommend laparoscopic surgery instead of laparotomy for patients previously submitted to abdominal surgery, concerning short-term benefits, such as conversion rates and morbidity. This review, although without a meta-analysis, brings new light into this matter.
- Citation: Figueiredo MN, Campos FG, D’Albuquerque LA, Nahas SC, Cecconello I, Panis Y. Short-term outcomes after laparoscopic colorectal surgery in patients with previous abdominal surgery: A systematic review. World J Gastrointest Surg 2016; 8(7): 533-540
- URL: https://www.wjgnet.com/1948-9366/full/v8/i7/533.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i7.533
In colorectal surgery, laparoscopy has been progressively accepted as a good alternative to open surgery since its first reports during the 90’s[1,2]. The main benefit attributed to laparoscopy is the associated better short-term outcomes observed in both benign and malignant colorectal diseases[3-6]. Moreover, randomized clinical trials and meta-analysis have suggested that there is no prejudice of oncological outcomes as well[3,7,8].
It is well recognized that the laparoscopic access to treat colorectal diseases is associated with an extended learning curve and has its own limitations. Many patient’s, disease’s and surgeon’s factors may affect operative results, such as previous abdominal open surgery (PAOS), obesity, inflammatory conditions, pregnancy, surgical expertise and others. At the beginning of laparoscopic experience, some of these conditions were even considered contraindications for this approach[9], due to the potential higher risk of intraoperative lesions, during trocar placement or because of visceral adhesions. In practice, these drawbacks were translated into a longer operative time and greater conversion rates. With growing expertise in laparoscopic techniques, surgeons gained confidence to perform more difficult cases and reports of laparoscopic procedures after PAOS have been increasingly published[10-12]. However, there is still a debate concerning the indication of laparoscopic colorectal surgery in patients with PAOS[13,14]. Furthermore, there is no randomized study evaluating the possible benefit of laparoscopic colorectal surgery in the context of PAOS.
Thus, the aim of this study was to perform a systematic review concerning short-term outcomes after laparoscopic colorectal surgery in patients with or without PAOS.
Incidence of conversion, inadvertent intraoperative intestinal lesions and overall morbidity were our main outcome measures.
Studies were included if they reported results on laparoscopic colorectal surgery in patients with PAOS, whether previously open or laparoscopic, with a special interest if they were comparative. Abstracts only were not included in the systematic review, although they were taken into consideration for discussion.
All authors agreed regarding terms that should be used for online search. The literature search comprised the terms “colorectal”, “colectomy”, “PAOS”, “previous surgery” and “PAOS” in different combinations. Articles were searched if published before August 2014 in the following databases: MEDLINE, EMBASE, Cochrane, Scopus, Scielo and LILACS. Initially the search was not limited by language, but only full texts in English were finally included. References in the selected articles were also searched for additional citations.
Titles and abstracts were scanned to identify suitable articles; afterwards abstracts were reviewed to identify studies fulfilling inclusion criteria. Finally, full texts of the interested studies were selected. Two authors performed the study selection and one author was responsible for revision of this selection. There were no conflicts regarding suitability of studies selected or excluded.
Two investigators were responsible to extract data from the studies to a previously designed datasheet, interesting outcomes of this study. Another investigator was responsible to review the information and to solve any conflicts. Information collected from the studies was: Overall conversion, inadvertent intraoperative lesions and morbidity. Definition of conversion was not always mentioned in the articles or differed between them. Mostly, conversion referred to unplanned incisions or size of incision in order to complete surgery. We have considered conversion as described in each study, as shown in Table 1.
| Ref. | Definition of conversion |
| Hamel et al[19] | “any incision unplanned, made sooner than planned or longer than 5 cm” |
| Kwok et al[26] | “abdominal incision exceeded 8 cm; or the incision was extended for any reasons other than division of the bowel and extraction of specimens” |
| Law et al[22] | N/A |
| Arteaga González et al[21] | N/A |
| Franko et al[23] | “change in operative strategy requiring exsufflation of capnoperitoneum and elongation of the surgical incision to allow direct visualization for continued dissection” |
| Vignali et al[14] | “abdominal incision longer than 7 cm or an abdominal incision made earlier or different from that planned at the start of the procedure” |
| Nozaki et al[17] | N/A |
| Offodile et al[25] | “final incision length longer than 7 cm (after skin closure)” |
| Barleben et al[16] | N/A |
| Fukunaga et al[24] | “performance of an unplanned incision” |
| Maggiori et al[18] | “any unplanned incision or a planned incision longer than 6 cm” |
| Naguib et al[20] | N/A |
| Yamamoto et al[13] | “any incision more than 8 cm in length needed to complete or facilitate the procedure that could not be completed” laparoscopically |
Analysis of articles was done according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses[15]. Forest plots were done using Review Manager (RevMan, Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012).
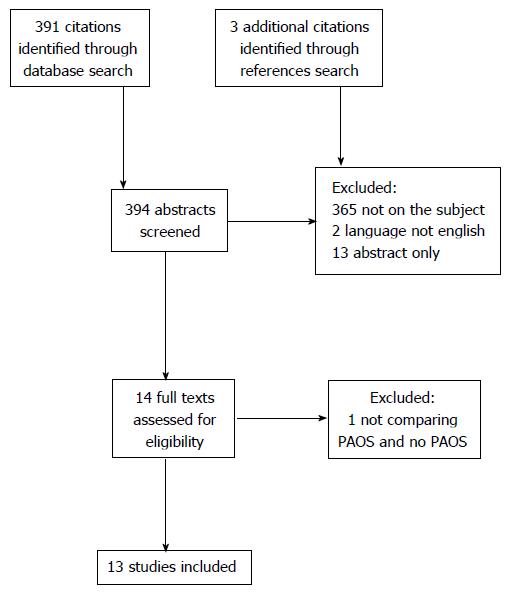
The literature search initially identified 391 articles. Search within references led us to include other 3 articles. Subject of citation did not meet the interest criteria of this study in 365 citations. Two studies were excluded because of language (Chinese and Italian) and 13 had only presented abstracts. Fourteen full-text articles were analysed and 13 studies were included in the present manuscript. One article was excluded because it did not describe nor compared laparoscopy with and without PAOS[13,14,16-26] (Figure 1).
Regarding their characteristics, with one exception, all studies were retrospective and comparative, but only two were case-matched[14,18]. One study was not comparative and only described a group of patients with PAOS[16] (Table 2).
| Ref. | Type of study | No. of patients | Conversion rate (%) | Inadvertent enterotomy (%) | ||||||
| Total | PAOS | non PAOS | PAOS | non PAOS | P-value | PAOS | non PAOS | P-value | ||
| Hamel et al[19] | Comparative | 85 | 36 | 49 | 17 | 12 | 0.754 | N/A | N/A | N/A |
| Kwok et al[26] | Comparative | 91 | 26 | 65 | 15.4 | 7.7 | 0.55 | N/A | N/A | N/A |
| Law et al[22] | Comparative | 295 | 84 | 211 | 17 | 11 | 0.181 | N/A | N/A | N/A |
| Arteaga González et al[21] | Comparative | 86 | 27 | 59 | 26.1 | 5.1 | 0.02 | 0 | 1.7 | NS |
| Franko et al[23] | Comparative | 820 | 347 | 473 | 19 | 11 | < 0.001 | 1.4 | 0.2 | 0.04 |
| Vignali et al[14] | Case-matched | 182 | 91 | 91 | 16.5 | 8.8 | 0.18 | N/A | N/A | N/A |
| Nozaki et al[17] | Comparative | 121 | 21 | 100 | 0 | 0 | N/A | N/A | N/A | N/A |
| Offodile et al[25] | Comparative | 414 | 171 | 243 | 17 | 15 | 0.42 | N/A | N/A | N/A |
| Barleben et al[16] | Observational; not comparative | 55 | 55 | 0 | 14.5 | N/A | N/A | N/A | N/A | N/A |
| Fukunaga et al[24] | Comparative | 607 | 192 | 415 | 5.2 | 2.6 | 0.108 | 2.6 | 0 | 0.001 |
| Maggiori et al[18] | Case-matched | 367 | 167 | 200 | 22 | 13 | 0.017 | N/A | N/A | N/A |
| Naguib et al[20] | Comparative | 181 | 68 | 113 | 13.2 | 10.6 | 0.6 | 2.9 | 0 | 0.14 |
| Yamamoto et al[13] | Comparative | 1701 | 580 | 1121 | 12.4 | 10.2 | 0.16 | 0.9 | 0.1 | 0.037 |
| Total | 5005 | 1865 | 3140 | |||||||
The selected studies comprised a total of 5005 patients, 1865 with PAOS. Four papers included not only open but also laparoscopic previous surgeries, and in most of them some kind of resection was done (i.e., excluding diagnostic laparoscopy and bypasses), excluding one study that included a few patients submitted to a diverting stoma[16]. In two studies[17,23], colorectal surgery included totally laparoscopic and also hand-assisted techniques. Regarding the type of surgical procedures performed, two studies[19,25] described only right colectomies, one included only anterior resections for upper rectum cancer[26], while others included all types of colorectal resections. Three articles included only patients diagnosed with colorectal cancer[17,24,26].
All but three studies[14,18,21] included previous appendectomy. Most previous surgeries described in the studies were appendectomies, gynaecological procedures or cholecystectomies. Of 1865 patients, only 294 (16%) were cited as having had a midline incision for previous gastrointestinal surgeries, while 702 (38%) had a previous appendectomy. Although we cannot separate results of only previous gastrointestinal procedures from gynaecological procedures and cholecystectomies, these 294 cases are the object of our interest in this paper.
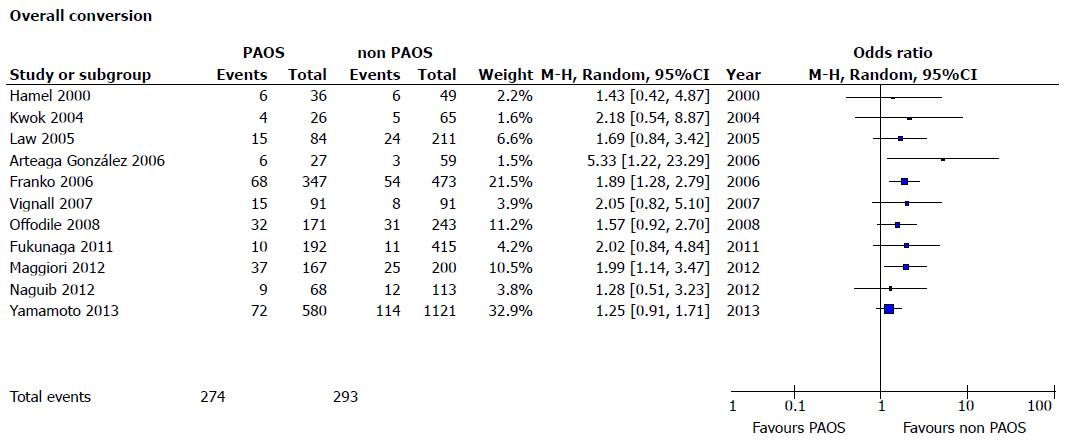
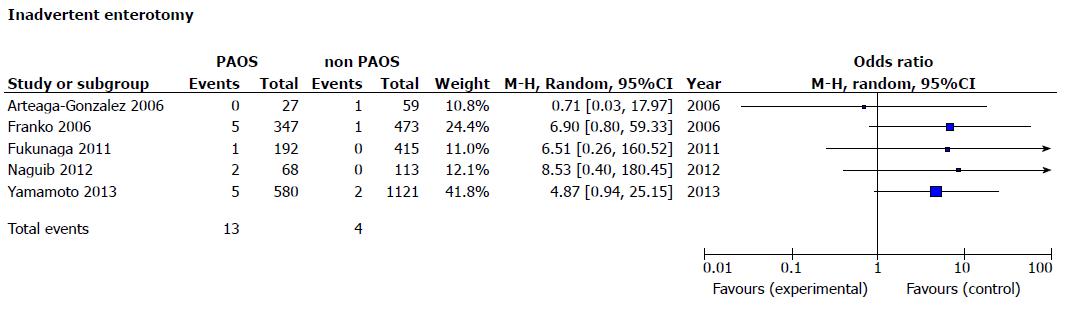
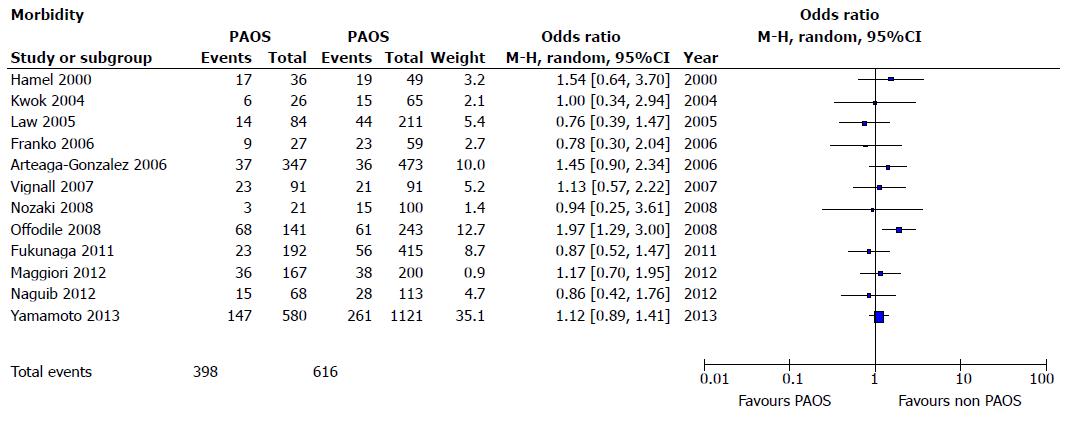
All studies were retrospective and with great heterogeneity, so a quantitative analysis (mata-analysis) was not carried out because it would not be of value. Nonetheless, a forest plot was made in order to provide an idea of trend in the results of this review, in case data could be adequately extracted.
Overall conversion rates were described in all 12 studies (Table 2). These rates were higher in all of the studies but only 3 of studies showed statistical significance[18,21,23] (Figure 2). There were no conversions in one of the studies[17].
In 3 of 5 studies, rates of intraoperative intestinal lesions (Figure 3) were higher in the PAOS groups (not necessarily leading to conversion)[13,23,24], while in two studies they were similar[20,21]. The other 8 papers did not describe such data (Table 2).
In the 9 studies that reported postoperative complication rates, similar rates were reported between patients with and without PAOS (Table 3). In 3 other studies the P value comparing overall morbidity rates was not available, but numbers for independent complications were summed in order to perform odds ratio analysis (Figure 4).
| Ref. | No. of patients | Morbidity (%) | ||||
| Total | PAOS | non PAOS | PAOS | non PAOS | P-value | |
| Hamel et al[19] | 85 | 36 | 49 | 47 | 37 | 0.18 |
| Kwok et al[26] | 91 | 26 | 65 | 23 | 23 | 0.79 |
| Law et al[22] | 295 | 84 | 211 | 16 | 20 | 0.516 |
| Arteaga González et al[21] | 86 | 27 | 59 | 39 | 38 | NS |
| Franko et al[23] | 820 | 347 | 473 | N/A | N/A | N/A |
| Vignali et al[14] | 182 | 91 | 91 | 25.3 | 23.1 | 0.86 |
| Nozaki et al[17] | 121 | 21 | 100 | 14 | 15 | 0.94 |
| Offodile et al[25] | 414 | 171 | 243 | N/A | N/A | N/A |
| Barleben et al[16] | 55 | 55 | 0 | N/A | N/A | N/A |
| Fukunaga et al[24] | 607 | 192 | 415 | 15.6 | 14.5 | 0.767 |
| Maggiori et al[18] | 367 | 167 | 200 | 22 | 19 | 0.543 |
| Naguib et al[20] | 181 | 68 | 113 | N/A | N/A | N/A |
| Yamamoto et al[13] | 1701 | 580 | 1121 | 25.3 | 23.3 | 0.345 |
To date, very few studies have been devoted to evaluate the impact of PAOS on the short-term results after laparoscopic colorectal surgery. The present literature review with more than 5000 patients (including 1800 that had PAOS and 264 with previous gastrointestinal resection by midline incision) suggests that PAOS has probably little impact on postoperative morbidity after laparoscopic colorectal surgery.
It is important to state that previous surgery away from the site of the current surgery might not interfere in short-term outcomes, for ex. previous gynaecological surgery in a patient that is going to be submitted to a transverse colon resection should not present a problem regarding technical aspects and subsequent results.
Although conversion rates were higher in few studies (mainly because of adhesion), and the risk of inadvertent enterotomy was also slightly increased, overall postoperative morbidity was similar with or without PAOS. According to the literature, conversion from laparoscopic to open surgery does not seem to influence directly in post-operative morbidity[27]. In our study, although 3 studies reported higher conversion rates in the PAOS groups, morbidity was similar in both groups.
Due to the heterogeneity of the studies, it was not possible to perform a meta-analysis with qualitative results. This heterogeneity refers not only to statistical methods or study design, but also to different types of surgery (previous and actual) and diseases, as well as experience of the surgeon, which makes it hard to compare as equal.
In a pragmatic approach, laparoscopy should not be contraindicated in patients with PAOS and this is common sense for most surgeons, though it is not well established by current medical literature so far. Although surgeon and patient must be aware of the higher risk of conversion and possible accidental enterotomy, because of all the possible benefits previously demonstrated after laparoscopic colorectal surgery, laparoscopy might be attempted in most of the patients.
Short-term benefits of laparoscopic colorectal resection are clearly demonstrated by several randomized studies, including faster recovery, lower pain, earlier feeding and shorter return of normal intestinal function and shorter hospital stay[6,28-30]. However, it remains controversial if patients still profit from laparoscopic advantages in cases of PAOS. There is no doubt that intra-abdominal adherences may substantially impair intra and postoperative outcomes, mainly due to difficulties when performing adhesiolysis and the risks of visceral perforations. In fact, abdominal adhesions following laparotomy have been described in up to 70% to 90% of patients[31,32], and this may reflect in a longer operative time, mainly due to adhesiolysis, even in open surgery[33], and may lead, also in open surgery, to a higher risk of small bowel lesion in up to 20%[34].
Conversion rates in laparoscopic colorectal surgery range between 5% and 23%[4,35-40]. Although some studies did not find PAOS as a risk factor for higher conversion rates[36,39,41,42], it is believed that PAOS has the potential to increase these rates. In our opinion and practice, we believe that a systematic laparoscopic approach in colorectal surgery for patients with PAOS should be done, except for those with wound dehiscence for which repair is indicated.
Our literature review about laparoscopic surgery in patients with PAOS is in accordance with our strategy: Overall postoperative morbidity was similar whether there was PAOS or not. However, it must be noticed that conversion rates are probably slightly higher in cases of PAOS (demonstrated in only 3/12 studies) mainly because of adhesions, as suggested in 5/6 studies.
We are aware that inflammatory cases (Inflammatory Bowel Disease and diverticulitis) may sometimes present as an even bigger challenge than colorectal cancer and that a learning curve is fundamental for a surgeon to achieve advanced laparoscopic skills and overcome technical difficulties. Therefore, surgeons without significant experience in laparoscopy should carefully select PAOS cases. However, with growing experience in laparoscopic surgery, we consider that adhesion is no more a contraindication to laparoscopic surgery. Even if several minutes might be necessary in the beginning of the procedure to perform adhesiolysis, we consider that avoiding an unnecessary laparotomy may bring several advantages. First, it avoids a traumatic aggression on a previous healed abdominal incision, with the risk of long-term hernia; second, it allows keeping all the short-term advantages of laparoscopy.
In our systematic review, risk of inadvertent enterotomy seems higher with than without PAOS, but this aspect was in fact evaluated in only 5 of 12 studies, and demonstrated in only 3 of those 5 studies.
The main limitation of our review is the heterogeneity of the studies and the absence of prospective studies. For these reasons, it does not allow us to perform quantitative analysis, pooling the results together. Among the studies excluded from our review for being abstracts only, we could also perceive a trend suggesting that conversion rates in patients with PAOS is not higher than that in non PAOS groups[43-47]. In one abstract referring to risk factors for conversion during laparoscopy in colorectal surgery, PAOS was not identified as one[48]. Furthermore, in the context of Crohn’s disease, where redo surgery is frequent, two teams have demonstrated that performing a redosurgery by laparoscopy is feasible without increased morbidity rate[43,49], even though short-term benefits might not be the same as in first-time laparoscopies for IBD.
In conclusion, this review suggests that laparoscopic surgery in patients with PAOS is feasible and it is not associated with higher morbidity rates. Although the potential risks of conversion (due to adherences) and inadvertent enterotomies must not be forgotten, we consider that they are not enough to contraindicate laparoscopy in these patients.
Laparoscopy became the standard technique in many gastrointestinal procedures. But still there is controversy when it comes to perform colorectal surgery in patients that were operated on by a previous laparotomy, since there are no definite studies in this matter. Adhesions and consequent conversion might pose a problem as well as possible higher morbidity rates derived from those. Several articles have compared patients with and without previous abdominal open surgery, but most have a small number of patients, making it harder to make definite assumptions.
If the authors could consider only patients with previous gastrointestinal resections through midline incision they might bring an even better light in this subject of laparoscopy in case of previous abdominal surgery.
A systematic review concerning a theme that has not been so far elucidated by the current literature, to try to stimulate the debate and since a controlled study with such design is not probable, they might have to take the best evidence from uncontrolled studies.
Surgeons might use a systematic revision as an extra support to the belief that previous surgery is no longer a contraindication for laparoscopy in colorectal surgery.
This manuscript is a satisfactorily written systemic review on this problematic subject.
P- Reviewer: Agresta F, Aly EH, Aytac E, Oncel M, Pedziwiatr M, Yamamoto M S- Editor: Qiu S L- Editor: A E- Editor: Jiao XK
| 1. | Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1:144-150. [PubMed] |
| 2. | Redwine DB, Sharpe DR. Laparoscopic segmental resection of the sigmoid colon for endometriosis. J Laparoendosc Surg. 1991;1:217-220. [PubMed] |
| 3. | Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1901] [Cited by in RCA: 1816] [Article Influence: 79.0] [Reference Citation Analysis (0)] |
| 4. | Campos FG, Valarini R. Evolution of laparoscopic colorectal surgery in Brazil: results of 4744 patients from the national registry. Surg Laparosc Endosc Percutan Tech. 2009;19:249-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Alves A, Panis Y, Slim K, Heyd B, Kwiatkowski F, Mantion G. French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg. 2005;92:1520-1525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;CD003145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 431] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 7. | Fleshman JW, Nelson H, Peters WR, Kim HC, Larach S, Boorse RR, Ambroze W, Leggett P, Bleday R, Stryker S. Early results of laparoscopic surgery for colorectal cancer. Retrospective analysis of 372 patients treated by Clinical Outcomes of Surgical Therapy (COST) Study Group. Dis Colon Rectum. 1996;39:S53-S58. [PubMed] |
| 8. | Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010;97:1638-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 830] [Cited by in RCA: 737] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 9. | Curet MJ. Special problems in laparoscopic surgery. Previous abdominal surgery, obesity, and pregnancy. Surg Clin North Am. 2000;80:1093-1110. [PubMed] |
| 10. | Schirmer BD, Dix J, Schmieg RE, Aguilar M, Urch S. The impact of previous abdominal surgery on outcome following laparoscopic cholecystectomy. Surg Endosc. 1995;9:1085-1089. [PubMed] |
| 11. | Yu SC, Chen SC, Wang SM, Wei TC. Is previous abdominal surgery a contraindication to laparoscopic cholecystectomy? J Laparoendosc Surg. 1994;4:31-35. [PubMed] |
| 12. | Miller K, Hölbling N, Hutter J, Junger W, Moritz E, Speil T. Laparoscopic cholecystectomy for patients who have had previous abdominal surgery. Surg Endosc. 1993;7:400-403. [PubMed] |
| 13. | Yamamoto M, Okuda J, Tanaka K, Kondo K, Asai K, Kayano H, Masubuchi S, Uchiyama K. Effect of previous abdominal surgery on outcomes following laparoscopic colorectal surgery. Dis Colon Rectum. 2013;56:336-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Vignali A, Di Palo S, De Nardi P, Radaelli G, Orsenigo E, Staudacher C. Impact of previous abdominal surgery on the outcome of laparoscopic colectomy: a case-matched control study. Tech Coloproctol. 2007;11:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [PubMed] |
| 16. | Barleben A, Gandhi D, Nguyen XM, Che F, Nguyen NT, Mills S, Stamos MJ. Is laparoscopic colon surgery appropriate in patients who have had previous abdominal surgery? Am Surg. 2009;75:1015-1019. [PubMed] |
| 17. | Nozaki I, Kubo Y, Kurita A, Ohta K, Aogi K, Tanada M, Takashima S. Laparoscopic colectomy for colorectal cancer patients with previous abdominal surgery. Hepatogastroenterology. 2008;55:943-946. [PubMed] |
| 18. | Maggiori L, Cook MC, Bretagnol F, Ferron M, Alves A, Panis Y. Prior abdominal open surgery does not impair outcomes of laparoscopic colorectal surgery: a case-control study in 367 patients. Colorectal Dis. 2013;15:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Hamel CT, Pikarsky AJ, Weiss E, Nogueras J, Wexner SD. Do prior abdominal operations alter the outcome of laparoscopically assisted right hemicolectomy? Surg Endosc. 2000;14:853-857. [PubMed] |
| 20. | Naguib N, Saklani A, Shah P, Mekhail P, Alsheikh M, AbdelDayem M, Masoud AG. Short-term outcomes of laparoscopic colorectal resection in patients with previous abdominal operations. J Laparoendosc Adv Surg Tech A. 2012;22:468-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Arteaga González I, Martín Malagón A, López-Tomassetti Fernández EM, Arranz Durán J, Díaz Luis H, Carrillo Pallares A. Impact of previous abdominal surgery on colorectal laparoscopy results: a comparative clinical study. Surg Laparosc Endosc Percutan Tech. 2006;16:8-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Law WL, Lee YM, Chu KW. Previous abdominal operations do not affect the outcomes of laparoscopic colorectal surgery. Surg Endosc. 2005;19:326-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Franko J, O’Connell BG, Mehall JR, Harper SG, Nejman JH, Zebley DM, Fassler SA. The influence of prior abdominal operations on conversion and complication rates in laparoscopic colorectal surgery. JSLS. 2006;10:169-175. [PubMed] |
| 24. | Fukunaga Y, Kameyama M, Kawasaki M, Takemura M, Fujiwara Y. Laparoscopic colorectal surgery in patients with prior abdominal surgery. Dig Surg. 2011;28:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Offodile AC, Lee SW, Yoo J, Whelan RL, Moradi D, Baxter R, Arnell TD, Nasar A, Sonoda T, Milsom JW. Does prior abdominal surgery influence conversion rates and outcomes of laparoscopic right colectomy in patients with neoplasia? Dis Colon Rectum. 2008;51:1669-1674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Kwok SY, Chung CCC, Tsang WWC, Li MKW. Laparoscopic resection for rectal cancer in patients with previous abdominal surgery: A comparative study. Annals Of The College Of Surgeons (Hong Kong). 2004;8:115-119. |
| 27. | Aytac E, Stocchi L, Ozdemir Y, Kiran RP. Factors affecting morbidity after conversion of laparoscopic colorectal resections. Br J Surg. 2013;100:1641-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006;CD006231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 252] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 29. | Reza MM, Blasco JA, Andradas E, Cantero R, Mayol J. Systematic review of laparoscopic versus open surgery for colorectal cancer. Br J Surg. 2006;93:921-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 257] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 30. | Noel JK, Fahrbach K, Estok R, Cella C, Frame D, Linz H, Cima RR, Dozois EJ, Senagore AJ. Minimally invasive colorectal resection outcomes: short-term comparison with open procedures. J Am Coll Surg. 2007;204:291-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Ellis H. The causes and prevention of intestinal adhesions. Br J Surg. 1982;69:241-243. [PubMed] |
| 32. | Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18:260-273. [PubMed] |
| 33. | Coleman MG, McLain AD, Moran BJ. Impact of previous surgery on time taken for incision and division of adhesions during laparotomy. Dis Colon Rectum. 2000;43:1297-1299. [PubMed] |
| 34. | Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, Reijnen MM, Schaapveld M, Van Goor H. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000;87:467-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 277] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 35. | Pandya S, Murray JJ, Coller JA, Rusin LC. Laparoscopic colectomy: indications for conversion to laparotomy. Arch Surg. 1999;134:471-475. [PubMed] |
| 36. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1681] [Article Influence: 84.1] [Reference Citation Analysis (0)] |
| 37. | Croce E, Olmi S, Azzola M, Russo R, Di Bonifacio M. Laparoscopic colectomy: indications, standardized technique and results after 6 years experience. Hepatogastroenterology. 2000;47:683-691. [PubMed] |
| 38. | Casillas S, Delaney CP, Senagore AJ, Brady K, Fazio VW. Does conversion of a laparoscopic colectomy adversely affect patient outcome? Dis Colon Rectum. 2004;47:1680-1685. [PubMed] |
| 39. | Tekkis PP, Senagore AJ, Delaney CP. Conversion rates in laparoscopic colorectal surgery: a predictive model with, 1253 patients. Surg Endosc. 2005;19:47-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 168] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 40. | Kelly M, Bhangu A, Singh P, Fitzgerald JE, Tekkis PP. Systematic review and meta-analysis of trainee- versus expert surgeon-performed colorectal resection. Br J Surg. 2014;101:750-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 41. | Thorpe H, Jayne DG, Guillou PJ, Quirke P, Copeland J, Brown JM. Patient factors influencing conversion from laparoscopically assisted to open surgery for colorectal cancer. Br J Surg. 2008;95:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 42. | Vaccaro CA, Rossi GL, Quintana GO, Soriano ER, Vaccarezza H, Rubinstein F. Laparoscopic colorectal resections: a simple predictor model and a stratification risk for conversion to open surgery. Dis Colon Rectum. 2014;57:869-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 43. | Aytac E, Stocchi L, Remzi FH, Kiran RP. Is laparoscopic surgery for recurrent Crohn’s disease beneficial in patients with previous primary resection through midline laparotomy? A case-matched study. Surg Endosc. 2012;26:3552-3556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 44. | Naguib N, Saklani A, Shah P, Mekhail P, AbdelDayem M, Alsheikh M. Short term outcomes of laparoscopic colorectal surgery in patients with perious abdominal operations, 10 years experience. Surgical Endoscopy and Other Interventional Techniques. 2013;27:S97. |
| 45. | Huang CC, Su CH, Ghen YC, Fan WC, Ma CJ, Huang CJ. The impact of previous surgery on clinical outcomes of laparoscopic colectomy for colorectal cancer. Surgical Endoscopy and Other Interventional Techniques. 2013;27:S113. |
| 46. | Patel K, Siddiqi N, Flashman KG, O’Leary DP, Khan JS. Laparoscopic colorectal surgery outcomes for patients with previous abdominal surgery. Colorectal Disease. 2011;13:30. |
| 47. | King A, Bracey E, Flashman D, Senapati A, Skull A, O’Leary D. Does higher BMI and previous abdominal surgery affect the clinical outcome or the conversion rate in laparoscopic colorectal surgery? Prospective data from 255 consecutive cases. Colorectal Disease. 2009;11:23. |
| 48. | Gellona J, Inostroza G, Miguieles R, Elena Molina M, Bellolio F, Urrejola G, Espinola D, Larach T, Zuniga JM. Predictive factors for conversion in laparoscopic colorectal surgery and impact on early postoperative period, an 848 patient case control study. Surgical Endoscopy and Other Interventional Techniques. 2013;27:S319. |
| 49. | Brouquet A, Bretagnol F, Soprani A, Valleur P, Bouhnik Y, Panis Y. A laparoscopic approach to iterative ileocolonic resection for the recurrence of Crohn’s disease. Surg Endosc. 2010;24:879-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |