Published online May 27, 2016. doi: 10.4240/wjgs.v8.i5.371
Peer-review started: November 13, 2015
First decision: November 27, 2015
Revised: February 1, 2016
Accepted: February 23, 2016
Article in press: February 24, 2016
Published online: May 27, 2016
Processing time: 187 Days and 20.6 Hours
Laparoscopic lavage and drainage is a novel approach for managing patients with Hinchey III diverticulitis. However, this less invasive technique has important limitations, which are highlighted in this systematic review. We performed a PubMed search and identified 6 individual series reporting the results of this procedure. An analysis was performed regarding treatment-related morbidity, success rates, and subsequent elective sigmoid resection. Data was available for 287 patients only, of which 213 (74%) were actually presenting with Hinchey III diverticulitis. Reported success rate in this group was 94%, with 3% mortality. Causes of failure were: (1) ongoing sepsis; (2) fecal fistula formation; and (3) perforated sigmoid cancer. Although few patients developed recurrent diverticulitis in follow-up, 106 patients (37%) eventually underwent elective sigmoid resection. Our data indicate that laparoscopic lavage and drainage may benefit a highly selected group of Hinchey III patients. It is unclear whether laparoscopic lavage and drainage should be considered a curative procedure or just a damage control operation. Failure to identify patients with either: (1) feculent peritonitis (Hinchey IV); (2) persistent perforation; or (3) perforated sigmoid cancer, are causes of concern, and will limit the application of this technique.
Core tip: Laparoscopic lavage and drainage for purulent peritonitis due to perforated diverticulitis has many limitations, which have been overlooked in the previously published case series of the literature. The available data from the unique RCT indicates that these results will not be reproduced in a trial where patients’ selection is avoided. There are three main limitations to the technique: (1) the risk of missing a persistent (incompletely sealed) perforation - 30% of cases; (2) the risk of missing fecal peritonitis enclosed within the sigmoid loop - 10% of cases; and (3) the risk of missing sigmoid carcinoma - 10% of cases).
- Citation: Gervaz P, Ambrosetti P. Critical appraisal of laparoscopic lavage for Hinchey III diverticulitis. World J Gastrointest Surg 2016; 8(5): 371-375
- URL: https://www.wjgnet.com/1948-9366/full/v8/i5/371.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i5.371
Severe septic complications of sigmoid diverticulitis, such as abscesses and peritonitis, are common emergencies in Western countries. While patients presenting with Hinchey stages I/II (pericolic and extra-mesocolic abscesses) are conservatively managed, those presenting with purulent (Hinchey III) or feculent (Hinchey IV) peritonitis undergo emergency surgery[1]. Most surgeons agree that a Hartmann procedure remains the best approach for Hinchey IV patients[2]. This operation, however, is associated with significant morbidity and mortality, as well as the need for a second operation, 3 mo later, to restore intestinal continuity. Patients with Hinchey III diverticulitis may benefit from less invasive approaches, and since the 1990s, laparoscopic lavage and drainage (LLD) was proposed as an alternative to resection procedures (either with or without primary anastomosis) for Hinchey III patients presenting with generalized purulent peritonitis[3] (Table 1). According to its proponents, this novel approach represents a definitive treatment for most patients presenting with diffuse purulent peritonitis of diverticular origin[4].
| Stage | Definition | Mortality (%) | Treatment |
| I | Small abscess (> 4 cm) | 0 | iv antibiotics |
| II | Large (> 4 cm) abscess | 5 | iv antibiotics + drainage |
| III | Purulent peritonitis | 25 | LLD, PA or Hartmann |
| IV | Fecal peritonitis | 50 | Hartmann |
Unfortunately, 20 years after its first description[5], it appears that LLD has failed to gain popularity: There are less than 15 series published so far, and many are limited to less than 10 patients, which is surprising in the view of the large number of emergency procedures performed for complicated sigmoid diverticulitis. As an example, between 1996 and 2006, there were 500000 admissions in English NHS hospitals for a primary diagnosis of diverticular disease and 22000 patients underwent emergency surgery[6]. The aim of this systematic review is to critically assess the existing data regarding the use of LLD for Hinchey III diverticulitis.
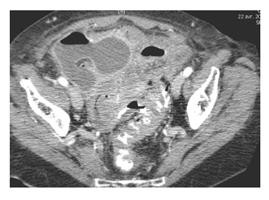
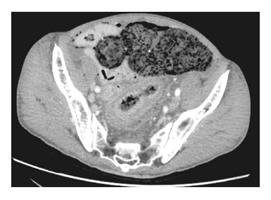
Hinchey III stage is defined by the presence of pus in the four quadrants of the abdomen. It’s a generalized peritonitis of diverticular origin but there is absence of feces in the abdominal cavity. Hinchey III is a life-threatening condition with a high morbidity and mortality. Many patients present often with renal failure, dehydration, and require immediate surgical attention. Of note, the distinction between stages III and IV is not possible by clinical examination, and the definitive diagnosis is made in the operating room during surgical exploration: In some cases, computed tomography scan imaging provides useful preoperative information, and may demonstrate the presence extra-intestinal feces (Figures 1 and 2).
Either the presence of a small amount of fluid in the Douglas pouch, or the presence of free air in the peritoneal cavity are not sufficient criteria for classifying the patient’s condition as Hinchey III. Both findings are common in Hinchey I/II patients, but these latter two categories have a much better prognostic due to the absence of diffuse peritonitis.
Laparoscopic lavage is a technique, which aims at treating the consequences of the perforation, and not the cause itself. Since many patients have, at the time of surgery, a perforation, which is sealed by the omentum or the small bowel, no attempt should be made to mobilize the sigmoid loop. A 4-trocars technique is recommended in order to gain access to the Douglas pouch and thoroughly wash the abdominal cavity with 5-10 L of warm saline, until the fluid in the suction catheter comes back clear. Two drains are left in the Douglas pouch and the left iliac fossa usually, and intravenous (iv) antibiotics prescribed for 5-10 d postoperatively[7].
Laparoscopic lavage is primarily a damage control approach, which aims at minimizing the consequences, and not treating the cause of peritonitis itself. In the case of Hinchey III diverticulitis, the assumption made by the proponents of the technique is that the sigmoid perforation is sealed at the time of the operation, so that LLD and iv antibiotics are sufficient to cure the patient. This may be true for some Hinchey III patients, but recent evidence suggest that 37% of patients who underwent emergency sigmoid resection showed persistent bowel perforation on review of histology[8].
The critical point is to determine whether: (1) LLD is a definitive technique - meaning that the patients’ problems of diverticulitis are for ever taken care of; or (2) LLD is merely a damage control procedure, which aims to delaying definitive treatment (elective sigmoid resection) a couple of months later[9]? It is interesting to note that the authors of the various series do not always agree on that issue. To simplify and summarizes the current debate, authors from the United Kingdom generally consider that laparoscopic lavage is a definitive treatment and that diverticulitis recurrence rarely occurs afterwards, thus precluding the need for subsequent sigmoid resection[10]. By contrast, authors from France believe that most patients successfully managed with LLD in the emergency setting will eventually need a sigmoid resection - they consider in fact that this approach is not a definitive treatment for diverticulitis[3]. These differences in the philosophy of this approach are important to emphasize, since its results are to be evaluated in a different manner.
We performed a PubMed search with the terms “perforated diverticulitis” and “laparoscopic lavage” and retrieved 6 series for a total of 279 patients who underwent LLD, but 200 patients only were classified as Hinchey III[7,11-15]. No indication was given upon the selection process, therefore it is impossible to know how many patients were not considered candidates for LLD; the small number of procedures raises the question that those 200 patients were selected in some way, most probably because they presented with less severe condition. Interestingly, the literature search revealed that LLD is often performed in patients with Hinchey II diverticulitis, a condition that usually does not require operative management: Thus, 25% of patients underwent unnecessary surgery, and represent a subgroup in which a so-called “minimally invasive” approach was actually overtreatment.
Reported success rates in these 6 series were extremely good: 94% of patients were successfully managed with LLD, with minimal (2%) mortality. Causes of failure were: (1) persistent sepsis; (2) fecal fistula formation; and (3) perforated sigmoid cancer. Although few patients developed recurrent diverticulitis in follow-up, 98 (49%) eventually underwent elective sigmoid resection (Table 2). There were wide variations (2%-50%) in the rate of recurrent diverticulitis after LLD. Not surprisingly, these differences translated into wide variations in the rate of subsequent sigmoid resections (0%-100%).
So far, there is only one published RCT on this topic (LADIES[16]), but laparoscopic lavage is currently assessed in 3 other trials, conducted in Ireland (LAPLAND) and Scandinavia (SCANDIV AND DILALA[17,18]). The Dutch LADIEs trial, however, was prematurely interrupted because of an exceedingly high rate of complications in the LLD group. The causes of failure in the lavage group were: Death (4%); surgical re-intervention (20%); recurrent abscess (20%); even worse, 5 (11%) patients were eventually diagnosed with sigmoid carcinoma. The authors of the study reported that, since the surgeons made no attempt to free the sigmoid colon from adjacent structures, large persistent perforations were missed. In the small group (46 patients) of LLD, there were a total of 28 surgical re-interventions, and it is therefore not surprising that the Safety Monitoring Board of the study decided to interrupt patients’ inclusion in the LLD arm of the trial.
The first lesson from the RCT is therefore that LLD is definitively not indicated for Hinchey IV patients. LLD is also not a good operation for patients with a persistent perforation. These individuals present with severe co-morbidities and have a high operative mortality due to sepsis. Resection surgery still remains the best option in this situation. We believe that the main problem of LLD is the absence of a surgical diagnosis: If the surgeon deliberately abandons the prospect of removing adhesions surrounding the source of infection, then he may overlook: (1) the cause of perforation (cancer vs diverticulitis); (2) the severity of perforation (sealed vs persistent); and (3) the presence of extra-digestive feculent discharge.
LLD is not a panacea, and so far did no meet expectations, as proven by the low number of patients who benefitted from this approach in the surgical literature (less than 200, compared to the huge number of emergency laparotomies performed every year for peritonitis of diverticular origin)[19]. LLD has no benefit in patients with Hinchey II, and no efficacy in patients with Hinchey IV diverticulitis. Thus, its indications remain strictly limited to Hinchey III, as initially proposed. A percentage of patients with perforated sigmoid carcinomas will be misdiagnosed as Hinchey III, thus these individuals also will not benefit from LLD - and this important limitation should be explained to the patient and his family before the operation. Recent evidence suggests that the rate of occult neoplasia is 10% in patients presenting with sigmoid perforation[20,21].
Finally, a high number of patients will recur after laparoscopic lavage, and present again with similar symptoms 2-6 mo after LLD. In our experience, this approach should therefore not be considered as a definitive treatment, but preferably as an attempt to avoid sigmoidectomy in the emergency setting. In summary, this approach has important limitations: It is not needed for Hinchey I-II patients; it is not efficient for Hinchey IV patients; most patients with Hinchey III diverticulitis will not be cured, and will require a definitive resection, meaning a second operation three months later, or will be exposed to a high risk of recurrence. Finally, a small but significant percentage of patients with perforated cancers will be misdiagnosed and re-operated with a worst prognosis and probably a very difficult operation 2-4 wk later. In conclusion, this approach has important limitations, and is not a safe alternative to sigmoid resection surgery for patients with Hinchey III diverticulitis.
Laparoscopic lavage and drainage for purulent peritonitis due to perforated diverticulitis has many limitations, which have been overlooked in the previously published case series of the literature; actually, it seems likely that the excellent results of these series are a result of a strong selection bias, as well as the inclusion of many patients with Hinchey II diverticulitis. The available data from the unique RCT indicates that these results will not be reproduced in a trial where patients’ selection is avoided. There are three main limitations to the technique: (1) the risk of missing a persistent (incompletely sealed) perforation - 30% of cases; (2) the risk of missing fecal peritonitis enclosed within the sigmoid loop - 10% of cases); and (3) the risk of missing sigmoid carcinoma - 10% of cases). LLD is deemed to fail in this group of patients. We conclude that LLD is not a safe approach for a majority of patients presenting with diffuse purulent peritonitis of diverticular origin.
P- Reviewer: Lohsiriwat V, Mocellin S S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85-109. [PubMed] |
| 2. | Regenbogen SE, Hardiman KM, Hendren S, Morris AM. Surgery for diverticulitis in the 21st century: a systematic review. JAMA Surg. 2014;149:292-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 3. | Faranda C, Barrat C, Catheline JM, Champault GG. Two-stage laparoscopic management of generalized peritonitis due to perforated sigmoid diverticula: eighteen cases. Surg Laparosc Endosc Percutan Tech. 2000;10:135-138; discussion 139-141. [PubMed] |
| 4. | Myers E, Winter DC. Adieu to Henri Hartmann? Colorectal Dis. 2010;12:849-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | O’Sullivan GC, Murphy D, O’Brien MG, Ireland A. Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg. 1996;171:432-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 153] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Jeyarajah S, Faiz O, Bottle A, Aylin P, Bjarnason I, Tekkis PP, Papagrigoriadis S. Diverticular disease hospital admissions are increasing, with poor outcomes in the elderly and emergency admissions. Aliment Pharmacol Ther. 2009;30:1171-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97-101. [PubMed] |
| 8. | O’Leary DP, Myers E, O’Brien O, Andrews E, McCourt M, Redmond HP. Persistent perforation in non-faeculant diverticular peritonitis--incidence and clinical significance. J Gastrointest Surg. 2013;17:369-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Weber DG, Bendinelli C, Balogh ZJ. Damage control surgery for abdominal emergencies. Br J Surg. 2014;101:e109-e118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 145] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 10. | McDermott FD, Collins D, Heeney A, Winter DC. Minimally invasive and surgical management strategies tailored to the severity of acute diverticulitis. Br J Surg. 2014;101:e90-e99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Radé F, Bretagnol F, Auguste M, Di Guisto C, Huten N, de Calan L. Determinants of outcome following laparoscopic peritoneal lavage for perforated diverticulitis. Br J Surg. 2014;101:1602-1606; discussion 1606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Karoui M, Champault A, Pautrat K, Valleur P, Cherqui D, Champault G. Laparoscopic peritoneal lavage or primary anastomosis with defunctioning stoma for Hinchey 3 complicated diverticulitis: results of a comparative study. Dis Colon Rectum. 2009;52:609-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | White SI, Frenkiel B, Martin PJ. A ten-year audit of perforated sigmoid diverticulitis: highlighting the outcomes of laparoscopic lavage. Dis Colon Rectum. 2010;53:1537-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Liang S, Russek K, Franklin ME. Damage control strategy for the management of perforated diverticulitis with generalized peritonitis: laparoscopic lavage and drainage vs. laparoscopic Hartmann’s procedure. Surg Endosc. 2012;26:2835-2842. [PubMed] |
| 15. | Swank HA, Mulder IM, Hoofwijk AG, Nienhuijs SW, Lange JF, Bemelman WA. Early experience with laparoscopic lavage for perforated diverticulitis. Br J Surg. 2013;100:704-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, Belgers EH, van Geloven AA, Gerhards MF, Govaert MJ, van Grevenstein WM. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet. 2015;386:1269-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Thornell A, Angenete E, Gonzales E, Heath J, Jess P, Läckberg Z, Ovesen H, Rosenberg J, Skullman S, Haglind E. Treatment of acute diverticulitis laparoscopic lavage vs resection (DILALA): study protocol for a randomised controlled trial. Trials. 2011;12:186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Oresland T, Schultz JK, Yaqub S, Rashidi M, Nilsen FR. Scandinavian diverticulitis Trial -SCANDIV. A randomized prospective multicenter trial. Available from: http://www.scandiv.com/Scandiv/SCANDIV_files/Scandiv protokoll110110.pdf. |
| 19. | Mutch MG. Complicated diverticulitis: are there indications for laparoscopic lavage and drainage? Dis Colon Rectum. 2010;53:1465-1466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Lau KC, Spilsbury K, Farooque Y, Kariyawasam SB, Owen RG, Wallace MH, Makin GB. Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: can colorectal cancer be confidently excluded? Dis Colon Rectum. 2011;54:1265-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Brar MS, Roxin G, Yaffe PB, Stanger J, MacLean AR, Buie WD. Colonoscopy following nonoperative management of uncomplicated diverticulitis may not be warranted. Dis Colon Rectum. 2013;56:1259-1264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |