Published online Sep 27, 2015. doi: 10.4240/wjgs.v7.i9.203
Peer-review started: March 28, 2015
First decision: May 13, 2015
Revised: June 6, 2015
Accepted: July 16, 2015
Article in press: July 17, 2015
Published online: September 27, 2015
Processing time: 187 Days and 7.8 Hours
AIM: To implement a quick and simple test - rapid assessment faecal incontinence score (RAFIS) and show its reliability and validity.
METHODS: From March 2008 through March 2010, we evaluated a total of 261 consecutive patients, including 53 patients with faecal incontinence. Demographic and comorbidity information was collected. In a single visit, patients were administered the RAFIS. The results obtained with the new score were compared with those of both Wexner score and faecal incontinence quality of life scale (FIQL) questionnaire. The patient without influence of the surgeon completed the test. The role of surgeon was explaining the meaning of each section and how he had to fill. Reliability of the RAFIS score was measured using intra-observer agreement and Cronbach’s alpha (internal consistency) coefficient. Multivariate analysis of the main components within the different scores was performed in order to determine whether all the scores measured the same factor and to conclude whether the information could be encompassed in a single factor. A sample size of 50 patients with faecal incontinence was estimated to be enough to detect a correlation of 0.55 or better at 5% level of significance with 80% power.
RESULTS: We analysed the results obtained by 53 consecutive patients with faecal incontinence (median age 61.55 ± 12.49 years) in the three scoring systems. A total of 208 healthy volunteers (median age 58.41 ± 18.41 years) without faecal incontinence were included in the study as negative controls. Pearson’s correlation coefficient between “state” and “leaks” was excellent (r = 0.92, P < 0.005). Internal consistency in the comparison of “state” and “leaks” yielded also excellent correlation (Cronbach’s α = 0.93). Results in each score were compared using regression analysis and a correlation value of r = 0.98 was obtained with Wexner score. As regards FIQL questionnaire, the values of “r” for the different subscales of the questionnaire were: “lifestyle”r = -0.87, “coping/behaviour”r = -0.91, “depression”r = -0.36 and “embarrassment”r = -0.90, (P < 0.01). A multivariate analysis showed that all the scoring systems measured the same factor. A single factor may explain 80.84% of the variability of FI, so all the scoring systems measure the same factor. Patient’s continence improves when RAFIS and Jorge-Wexner scores show low values and when the values obtained in the FIQL questionnaire are high.
CONCLUSION: RAFIS is a valid and reliable tool to assess Faecal Incontinence.
Core tip: There are different scales for measuring the severity and impact of faecal incontinence (FI), but no together. The authors recommend the combined use of them to get a complete evaluation of FI. The aim of the present study is to implement a quick and simple test to assess faecal incontinence - the rapid assessment faecal incontinence score - and show its reliability and validity. Its validity and reliability has been proved when compared with other widely used scores.
- Citation: Portilla FL, Calero-Lillo A, Jiménez-Rodríguez RM, Reyes ML, Segovia-González M, Maestre MV, García-Cabrera AM. Validation of a new scoring system: Rapid assessment faecal incontinence score. World Journal of Gastrointestinal Surgery 2015; 7(9): 203-207
- URL: https://www.wjgnet.com/1948-9366/full/v7/i9/203.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i9.203
Faecal incontinence (FI) refers to the inability to control gas, liquid or solid stool passage[1]. FI has a high prevalence in our environment, affecting 10% of primary care patients and having a significant impact on mental health[2]. The cause of FI can be stool characteristics, rectal or sphincter dysfunctions or neurological disorders[3].
The assessment of FI should be performed in a simple way but it must take into account two different factors which may be associated, that is, FI severity and impact of FI on quality of life of patients. As a result, its assessment may be difficult.
Severity refers to the number and characteristics of leaks and it can be measured using nominal scales, which is less frequent or by means of ordinal scales. The latter assign a numeric value to FI and are nowadays the preferred assessment method[4-7]. One of the most widely used scales is the Jorge-Wexner score (the wexner cleveland clinic florida score)[3].
The impact of FI on patient’s quality of life can be measured using generic scales such as the SF36 questionnaire. Visual analogue scales for grading FI have been employed as well[8]. Widely used is the rockwood faecal incontinence quality of life scale (FIQL)[9] which contains a total of 29 different items assessing social, emotional, occupational and functional aspects. This scale has been translated and validated into Spanish[10].
Although severity scales have progressively included items which try to measure “impact”, the impact FI has on patients is more thoroughly assessed using its own specific scales. Some authors even recommend the use of a combination of two different scoring systems for severity and impact on quality of life respectively in order to attain a complete evaluation of FI[11].
The objective of this study is to implement a new score that allows the joint measurement of severity and impact in a simple way. Reliability and validity have been analysed comparing the new score with the Jorge-Wexner score and FIQL questionnaire.
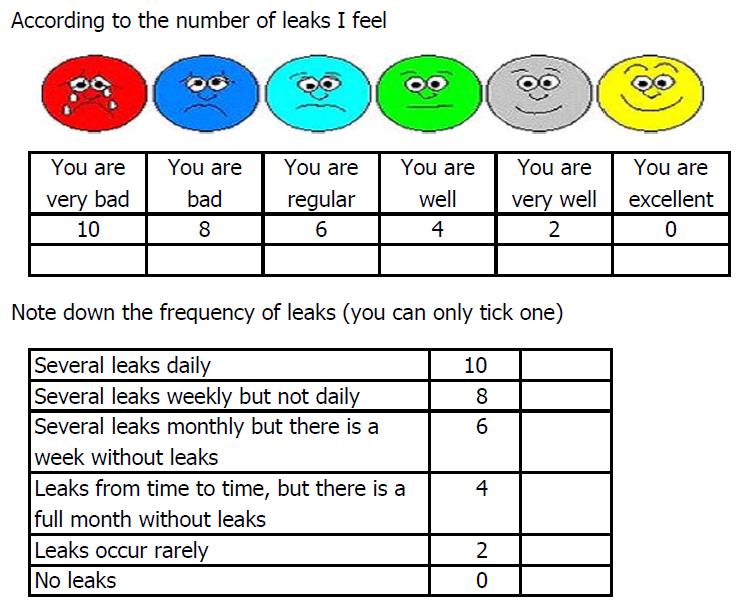
From March 2008 through March 2010, we evaluated a total of 261 consecutive patients (145 females, median age 59.05 ± 17.39 years) from the Proctology clinic. Demographic and comorbidity information was collected. In a single visit, patients were administered the Rapid Assessment Faecal Incontinence Score (RAFIS) (Figure 1), and the Jorge-Wexner score. The patient without influence of the surgeon completed the test. The role of surgeon was explaining the meaning of each section and how he had to fill.
The score is composed of two sections: (1) Visual-descriptive ordinal trying to define in concrete terms how it affects the patient fecal incontinence; and (2) the frequency of episodes, which generally describes many episodes of incontinences have the patient in a month.
RAFIS total score was obtained after each patient made a selection in our score according to the frequency and number of leaks.
A sample size of 50 patients with faecal incontinence was estimated to be enough to detect a correlation of 0.55 or better at 5% level of significance with 80% power.
Reliability of the RAFIS score was measured using intra-observer agreement and Cronbach's alpha (internal consistency) coefficient. In both cases, the items "State" and "Leaks" were compared. A value ≥ 0.7 is acceptable in the case of intra-observer agreement. As for Cronbach's alpha, an internal consistency value of α≥ 0.7 is acceptable and a value of α > 0.9 is excellent.
Validity of RAFIS score was assessed by means of convergent validity. RAFIS was compared with Jorge-Wexner score and with FIQL questionnaire. Also, a multivariate analysis of the main components within the different scores was performed in order to determine whether all the scores measured the same factor and to conclude whether the information could be encompassed in a single factor.
The statistical analysis was performed using SPSS 20.0 software and a value of P < 0.05 was considered significant.
Since no intervention was performed on patients, approval by the Ethics Committee was not necessary.
We analysed the results obtained by 53 consecutive patients with faecal incontinence (median age 61.55 ± 12.49 years) in the three scoring systems. A total of 208 healthy volunteers (median age 58.41 ± 18.41 years) without faecal incontinence were included in the study as negative controls. Age below 18 was an exclusion criteria. Table 1 shows demographic data and the results obtained in the scores.
| Incontinent patients | Control patients | |
| Number of patients | 53 | 208 |
| Age (mean ± SD) | 61.55 ± 12.49 | 58.41 ± 18.41 |
| RAFIS state (mean ± SD) | 6.91 ± 2.37 | 0 |
| RAFIS leaks (mean ± SD) | 7.25 ± 2.48 | 0 |
| RAFIS global (mean ± SD) | 14.15 ± 4.09 | 0 |
| Jorge-wexner score (mean ± SD) | 13.32 ± 4.95 | 0 |
| FIQL test lifestyle (mean ± SD) | 2.99 ± 0.96 | 4.99 ± 0.06 |
| FIQL test coping/behaviour (mean ± SD) | 2.48 ± 0.95 | 4.99 ± 0.06 |
| FIQL test depression (mean ± SD) | 3.23 ± 1.63 | 4.20 ± 0.84 |
| FIQL test embarassment (mean ± SD) | 2.59 ± 0.95 | 5 ± 0 |
RAFIS reliability was measured using intra-observer agreement. Pearson’s correlation coefficient between “state” and “leaks” was excellent (r = 0.92, P < 0.005). Internal consistency in the comparison of “state” and “leaks” yielded also excellent correlation (Cronbach’s α = 0.93).
Validity assessment of the new score yielded a high correlation with both Jorge-Wexner score and with the different subscales of FIQL, as shown in Table 2.
In order to complete the study, a multivariate analysis was also carried out of the global results obtained in the different scoring systems (Jorge-Wexner, FIQL lifestyle, coping/behaviour, depression and embarrassment) and RAFIS. A single factor may explain 80.84% of the variability of FI, so all the scoring systems measure the same factor. Patient’s continence improves when RAFIS and Jorge-Wexner scores show low values and when the values obtained in the FIQL questionnaire are high (Table 3).
| RAFIS global | 0.96 |
| Jorge-Wexner score | 0.96 |
| FIQL test lifestyle | -0.95 |
| FIQL test coping/behaviour | -0.97 |
| FIQL test depression | -0.47 |
| FIQL test embarrassment | -0.97 |
RAFIS comprises two items: State and leaks. The former is measured by means of a visual analogue scale and the latter by means of an ordinary scale.
Visual analogue scales were chosen as measurement tool because they have a high correlation with reality and are easy to understand by patients. Moreover, the advantages of visual analogue scales of faces are wellestablished[12].
In our study, the measurement of leaks introduces a novel simplification as it does not consider the quality of faecal leaks but only their frequency. We do not take into account such variables as pad usage (evaluated in Jorge-Wexner score or Vaizey test[6]), the necessity to change underwear (included in RFIS test[7]), faecal urgency or anti-diarrheal drugs (measured in Vaizey test).
In our country, Devesa et al[8] have used numeric visual analogue scales to assess the severity of FI and its impact on quality of life of patients. They found no correlation between visual analogue scales for FI and Jorge-Wexner score but they observed a significant correlation with the “embarrassment” subscale of FIQL. They also found correlation between visual analogue scales for quality of life and the “coping/behaviour” subscale of FIQL. Our study shows a significant correlation between RAFIS global and Jorge-Wexner score.
The impact of FI on quality of life has long been discussed and several studies have established the importance of such impact. Minguez et al[10] validated the FIQL into Spanish and compared it with the Jorge-Wexner score. These authors observed a strong correlation among all the items. Their study also showed that pad usage is an independent factor which worsened quality of life scores. Similar results have been reported by Bols et al[11] when they compared Jorge-Wexner score and Vaizey score with FIQL. They found a strong correlation between results, particularly in “embarrassment” and “coping/behaviour” subscales.
However, there are some studies which do not agree with these results. For instance, Bordeianou et al[13] in their analysis of the correlation between faecal incontinence severity index and every one of the subscales in FIQL, found moderate correlations with embarrassment and coping/behaviour but no correlation at all with lifestyle and depression.
Another study by Damon et al[14], comparing Jorge-Wexner score with gastrointestinal quality of life index questionnaire, found a poor correlation between FI severity and quality of life.
Our study shows significant correlation between RAFIS and every subscale of FIQL with the exception of “depression” although higher depression scores as well as prior hysterectomy have moderate to severe quality of life impairment. Some authors said when evaluating FI, screening for mood disturbances should be undertaken[15]; however depression is multifactorial, in fact biological and environmental factors may be involved. This explains why scales depression associated with FI only have a lower correlation, without implication to determine the complete evaluation of FI.
In our opinion, the election of aggressive therapy for the treatment of FI should consider not only severity of symptoms but also impact on the quality of life of patients.
Our study has some limitations. In order to assess the reliability of our score, we compared two factors: Leaks and state. We obtained a high correlation. However, the best statistical tool is the Test-Retest, as has been proven by similar studies[16]. The same measurement is performed repeatedly at short intervals, which does not allow patients to change their status. Unfortunately, logistical reasons made it impossible to perform the tes-retest. In spite of it, our score shows high reliability. Also, we could not demonstrate the sensitivity of our score to change after faecal incontinence therapy as our objective was to evaluate our new test to assess FI, so the test was not repeated after faecal incontinence therapy.
In our opinion RAFIS could be improved taking into account the factor of faecal urgency and a third section that refers to the type of incontinence (hard, liquid or gas feces). Urgency item was not taken into account due to the chosen gold standard scale for severity was Jorge-Wexner score, which does not include it, instead of Vaizey[6]. Vaizey score determines faecal urgency asking patients the ability to defer defecation for 15 min. We suggest asking about the need to stop the current activity in order to go to the toilet.
Bols et al[11] compared Jorge-Wexner, Vaizey and FIQL scores, and Vaizey score showed that items “medication use,”“pads,” and “flatus incontinence” had poor external responsiveness, whereas “urgency” had adequate external responsiveness. The item “pad use” of the Wexner score also had poor external responsiveness.
Although RAFIS seems a valid and reliable scoring system in our environment, which could even replace Jorge-Wexner score and FIQL questionnaire, we still believe it is highly advisable to use a diary system as it provides an objective measurement of FI if correctly filled out by patients.
In our opinion RAFIS could be improved taking into account the factor of faecal urgency.
Faecal incontinence severity comprises two factors: objective (severity/leaks) and subjective (impact on quality of life/state). A new quick and simple score to assess FI has been tested showing its validity and reliability when compared with other widely used scores.
CIBERehd was funded by the Instituto de Salud Carlo III.
Several questionnaires have been used in different studies to evaluate fecal incontinence and how patient’s life is disturbed by the symptoms. There are different scales for measuring the severity and impact of faecal incontinence (FI), but no together and a simple and quick score.
Creating a faecal incontinence scoring system which is both reproducible and simple to use is complex due to the variable nature of the condition.
There are different scales for measuring the severity and impact of FI, but no together. The authors recommend the combined use of them to get a complete evaluation of FI. The aim of the present study is to implement a quick and simple test to assess FI - the rapid assessment faecal incontinence score - and show its reliability and validity. Its validity and reliability has been proved when compared with other widely used scores. The research fulfills the criteria of novelty and innovative because it proposes and shows a new and reliable way to mesure faecal incontinence.
Clinical assessment of severity of faecal incontinence varies between clinicians according to their expertise. This causes difficulties when comparing results of published data, often making comparisons of treatment modalities meaningless. Many attempts have been made in the past to develop scoring systems but their clinical applicability has not been validated adequately. This study has established the validity of a quick and simple test to assess FI, and it could also help select patients who could benefit from a affective treatment.
The research is important, because it proposes a method of inquiring that could facilitate the communication between physicians and faecal incontinence patients. This new approach could have a positive impact on these patients treatment. Regarding the significance of the study findings, the authors showed excellent agreement and consistency for both criteria analyzed.
P- Reviewer: Amaro F, Santos-Antunes J, Teo M, Venskutonis D
S- Editor: Tian YL L- Editor: A E- Editor: Li D
| 1. | Baxter NN, Rothenberger DA, Lowry AC. Measuring fecal incontinence. Dis Colon Rectum. 2003;46:1591-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 94] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Parés D, Vial M, Bohle B, Maestre Y, Pera M, Roura M, Comas M, Sala M, Grande L. Prevalence of faecal incontinence and analysis of its impact on quality of life and mental health. Colorectal Dis. 2011;13:899-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2089] [Cited by in RCA: 1968] [Article Influence: 61.5] [Reference Citation Analysis (1)] |
| 4. | Pescatori M, Anastasio G, Bottini C, Mentasti A. New grading and scoring for anal incontinence. Evaluation of 335 patients. Dis Colon Rectum. 1992;35:482-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 223] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum. 1999;42:1525-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 597] [Cited by in RCA: 582] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 6. | Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 963] [Cited by in RCA: 973] [Article Influence: 37.4] [Reference Citation Analysis (1)] |
| 7. | Sansoni J, Hawthorne G, Fleming G, Marosszeky N. The revised faecal incontinence scale: a clinical validation of a new, short measure for assessment and outcomes evaluation. Dis Colon Rectum. 2013;56:652-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Devesa JM, Vicente R, Abraira V. Visual analogue scales for grading faecal incontinence and quality of life: their relationship with the Jorge-Wexner score and Rockwood scale. Tech Coloproctol. 2013;17:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC. Fecal Incontinence Quality of Life Scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum. 2000;43:9-16; discussion 16-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 929] [Cited by in RCA: 842] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 10. | Minguez M, Garrigues V, Soria MJ, Andreu M, Mearin F, Clave P. Adaptation to Spanish language and validation of the fecal incontinence quality of life scale. Dis Colon Rectum. 2006;49:490-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Bols EM, Hendriks HJ, Berghmans LC, Baeten CG, de Bie RA. Responsiveness and interpretability of incontinence severity scores and FIQL in patients with fecal incontinence: a secondary analysis from a randomized controlled trial. Int Urogynecol J. 2013;24:469-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Li L, Liu X, Herr K. Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med. 2007;8:223-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 143] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | Bordeianou L, Rockwood T, Baxter N, Lowry A, Mellgren A, Parker S. Does incontinence severity correlate with quality of life Prospective analysis of 502 consecutive patients. Colorectal Dis. 2008;10:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Damon H, Dumas P, Mion F. Impact of anal incontinence and chronic constipation on quality of life. Gastroenterol Clin Biol. 2004;28:16-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Smith TM, Menees SB, Xu X, Saad RJ, Chey WD, Fenner DE. Factors associated with quality of life among women with fecal incontinence. Int Urogynecol J. 2013;24:493-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Hussain ZI, Lim M, Stojkovic S. The test-retest reliability of fecal incontinence severity and quality-of-life assessment tools. Dis Colon Rectum. 2014;57:638-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |