Published online Aug 27, 2015. doi: 10.4240/wjgs.v7.i8.170
Peer-review started: March 26, 2015
First decision: April 27, 2015
Revised: May 14, 2015
Accepted: June 4, 2015
Article in press: June 8, 2015
Published online: August 27, 2015
Processing time: 160 Days and 23 Hours
Gangliocytic paragangliomas are rare tumors that almost exclusively occur within the second portion of the duodenum. Although these tumors generally have a benign clinical course, they have the potential to recur or metastasize to regional lymph nodes. The case report presented here describes a 57-year-old female patient with melena, progressive asthenia, anemia, and a mass in the second-third portion of the duodenum that was treated by local excision. The patient was diagnosed with a friable bleeding tumor. The histologic analysis showed that the tumor was a 4 cm gangliocytic paraganglioma without a malignant cell pattern. In the absence of local invasion or distant metastasis, endoscopic resection represents a feasible, curative therapy. Although endoscopic polypectomy is currently considered the treatment of choice, it is not recommended if the size of the tumor is > 3 cm and/or there is active or recent bleeding. Patients diagnosed with a gangliocytic paraganglioma should be closely followed-up for possible local recurrence.
Core tip: We present the case of a patient with a rare duodenal gangliocytic paraganglioma that was treated by tumorectomy. Although there is currently no consensus for treatment, this report demonstrates that local conservative tumorectomy is a feasible, curative therapy. Patients diagnosed with a gangliocytic paraganglioma should be closely followed-up for possible local recurrence.
- Citation: Hernández AG, Lanuza EDA, Matias AC, Huertas RP, Rodriguez KMG, Perez PG, Mompean FO. Large gangliocytic paraganglioma of the duodenum: A rare entity. World J Gastrointest Surg 2015; 7(8): 170-173
- URL: https://www.wjgnet.com/1948-9366/full/v7/i8/170.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i8.170
Gangliocytic paragangliomas (GPs) are rare neuroendocrine tumors that predominantly arise within the second part of the duodenum. GPs seldom recur or metastasize to regional lymph nodes[1], and are considered epithelial tumors according to the classification of tumors of the digestive tract by the World Health Organization[2]. Diagnosis of GP can be achieved based on histopathology showing epithelioid, spindle and ganglion cells, which are similarly observed for paragangliomas[3]. This report describes the case of a 57-year-old woman with melena, progressive asthenia, anemia, and a mass in the second–third portion of the duodenum that was finally diagnosed as a GP.
A 57-year-old female presented with upper abdominal pain associated with melena, asthenia, and anemia. She had a history of gluten intolerance but no fever or weight loss. A physical examination revealed pale conjunctiva and no cervical lymphadenopathy. An abdominal examination revealed tenderness in the upper abdomen with no rebound tenderness, hepatosplenomegaly, or palpable masses. Laboratory analyses showed anemia as the only pathologic finding (hemoglobin level of 9 g/dL), with normal renal and liver function. Ultrasound examination was also normal. A polypoid tumor on the third portion of the duodenum was revealed upon endoscopic examination (Figure 1). The tumor was not amenable to endoscopic resection, however, multiple biopsies were performed showing a cellular pattern of intraepithelial lymphocytes (CD8+) with Marsh grade I. The presence of the polypoid formation in the proximal duodenum was confirmed by a capsule endoscopy.
Resection of the neoplasm using a laparoscopic transduodenal approach and a concomitant intraoperative duodenoscopy were planned. However, technical difficulties prevented clear identification of the lesion, and the procedure was converted to an open surgery. The tumor was then completely resected through a longitudinal duodenotomy.
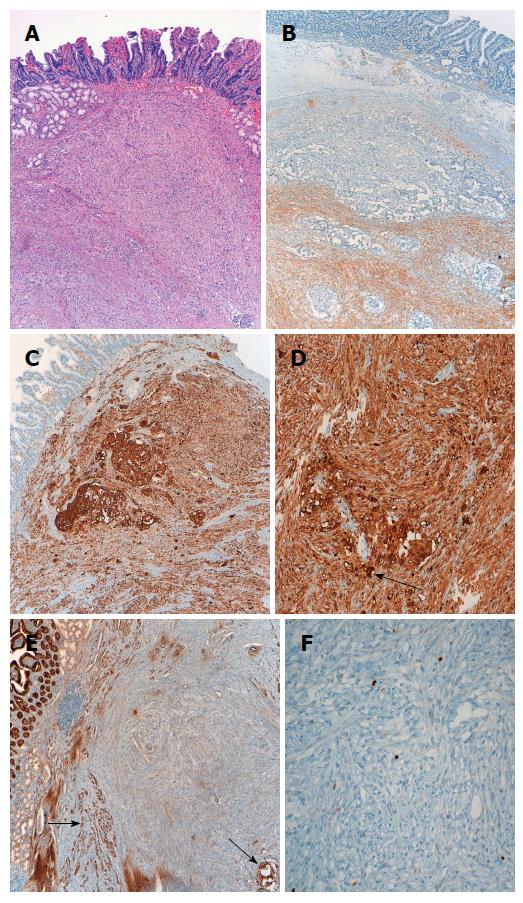
Histopathologic examination of the tumor indicated a 4 cm GP without a malignant cell pattern. The surgical margin was free of neoplastic infiltration and there were no histologic findings indicative of aggressive behavior, such as mitosis and/or pleomorphism. Immunohistochemical analysis showed that the tumor was positive for synaptophysin and enolase. Additionally, epithelioid cells were immunopositive for chromogranin and cytokeratin, and fusocellular cells were S-100-positive[4] (Figure 2).
The patient had an uneventful postoperative period and was discharged after 4 d. At the 3 mo follow-up, the patient was free of symptoms and the endoscopy was normal.
GPs are rare tumors that tend to occur in the 5th decade, and more often affect men (1.8:1)[5]. These tumors typically present with gastrointestinal bleeding, whereas obstructive jaundice is very uncommon. Endoscopic ultrasonography is useful for preoperative differential diagnosis from gastrointestinal stromal tumors, carcinoids, and periampullary adenomas. GPs generally follow a benign course, rarely showing invasive growth patterns or lymph node metastasis.
GPs can be curatively treated by endoscopic resection in the absence of local invasion or distant metastasis. Sathyamurthy et al[6] described a case successfully treated with endoscopic retrograde cholangiography with biliary sphincterotomy to relieve jaundice. In their patient, a periampullary nodule was detected that partially obstructed the orifice of the major papilla, which was treated with en bloc endoscopic mucosal resection with an electrocautery snare. Several recent reports indicate that endoscopic polypectomy is the treatment of choice, except in cases where the tumor is > 3 cm and/or there is active or recent bleeding[7-9]. A polypectomy was not performed in the current case due to recent bleeding and the diameter of the neoplasm (4-5 cm).
Evans et al[10] reported a case of duodenal GP mimicking an ampullary tumor. In their case, marked secondary obstructive chronic pancreatitis was intraoperatively observed in the remaining pancreas necessitating a pylorus-preserving total pancreatectomy. Two years after surgery, the patient remained alive and well on medical treatment with no evidence of tumor recurrence. Although the recurrence index is quite low after local resection[11], Witkiewicz et al[12] concluded that the possibility of recurrence, lymph node involvement, and distant metastasis indicates that more extensive surgical therapy may be warranted. Indeed, surgical treatment is indicated for all GPs that are unresectable by upper gastrointestinal endoscopy and for all malignant forms. However, laparoscopic resection may be adequate for benign forms, due to the advantages of the minimally invasive approach, as demonstrated by Parini et al[13].
Patients who have undergone successful excision of a large polyp should receive a follow-up endoscopy after 3-6 mo, depending on the histologic findings, to verify that the resection was complete. This process should then be repeated if a residual polyp is detected. If complete resection is not possible after two or three examinations, the patient should then be referred for another surgical therapy.
A 57-year-old woman presented with upper abdominal pain associated with melena, asthenia, and anemia.
A polypoid tumor was observed in the duodenum.
Gastrointestinal stromal tumor; carcinoid; periampullary adenoma.
Hemoglobin at 9 g/dL, with normal liver and renal function.
Computed tomography scans were normal.
Gangliocytic paraganglioma was diagnosed by microscopic examination and immunohistochemical study.
Simple excision of the tumor was performed.
Gangliocytic paragangliomas are rare tumors, with very few reports published in the literature.
Gangliocytic paraganglioma is a rare neuroendocrine tumor predominantly arising in the second part of the duodenum, with rare local recurrence or metastasis to regional lymph nodes.
Complete surgical resection remains the only curative treatment, and long-term careful follow-up is necessary for these patients.
This manuscript is well designed with visual materials and will contribute to the literature. It is a nice case report with good description of symptoms and treatment of this tumor entity.
P- Reviewer: Petronella P, Scheidbach H S- Editor: Tian YL L- Editor: A E- Editor: Jiao XK
| 1. | Kwon J, Lee SE, Kang MJ, Jang JY, Kim SW. A case of gangliocytic paraganglioma in the ampulla of Vater. World J Surg Oncol. 2010;8:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, Cavenee WK. The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol. 2002;61:215-225; discussion 226-229. [PubMed] |
| 3. | Perrone T, Sibley RK, Rosai J. Duodenal gangliocytic paraganglioma. An immunohistochemical and ultrastructural study and a hypothesis concerning its origin. Am J Surg Pathol. 1985;9:31-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 125] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Hoffmann KM, Furukawa M, Jensen RT. Duodenal neuroendocrine tumors: Classification, functional syndromes, diagnosis and medical treatment. Best Pract Res Clin Gastroenterol. 2005;19:675-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 124] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | Narang V, Behl N, Sood N, Puri H. Gangliocytic paraganglioma of duodenum. Case Rep Pathol. 2013;2013:378582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Sathyamurthy A, Choudhary A, Ng D, Okponobi S, Diaz-Arias A, Grewal A, Hammoud GM. Obstructive jaundice due to a rare periampullary tumor. World J Gastrointest Oncol. 2013;5:195-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Sánchez-Pobre P, Sáenz-López S, Rodríguez S, Sánchez F, Alemany I, López G, Colina F, Martínez-Montiel P, Marín JC, Castellano G. Safe endoscopic resection of gangliocytic paraganglioma of the major duodenal papilla. Rev Esp Enferm Dig. 2004;96:660-662; 663-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Nagai T, Torishima R, Nakashima H, Tanahashi J, Iwata M, Ookawara H, Yokoyama S, Yada K, Sato R, Murakami K. Duodenal gangliocytic paraganglioma treated with endoscopic hemostasis and resection. J Gastroenterol. 2004;39:277-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Yang JI, Choi JS, Lee GH, Kim BW, Moon SJ, Kang MS, Ahn HJ. A case of ampullary gangliocytic paraganglioma. Korean J Intern Med. 2014;29:375-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Evans JD, Wilson PG, Barber PC, Neoptolemos JP. Duodenal gangliocytic paraganglioma presenting as an ampullary tumor. Int J Pancreatol. 1996;20:131-134. [PubMed] |
| 11. | Scheithauer BW, Nora FE, LeChago J, Wick MR, Crawford BG, Weiland LH, Carney JA. Duodenal gangliocytic paraganglioma. Clinicopathologic and immunocytochemical study of 11 cases. Am J Clin Pathol. 1986;86:559-565. [PubMed] |
| 12. | Witkiewicz A, Galler A, Yeo CJ, Gross SD. Gangliocytic paraganglioma: case report and review of the literature. J Gastrointest Surg. 2007;11:1351-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |