Published online Aug 27, 2015. doi: 10.4240/wjgs.v7.i8.160
Peer-review started: February 6, 2015
First decision: April 13, 2015
Revised: April 15, 2015
Accepted: July 7, 2015
Article in press: July 8, 2015
Published online: August 27, 2015
Processing time: 209 Days and 17.7 Hours
AIM: To investigate the role of laparoscopy in diagnosis and treatment of intra abdominal infections.
METHODS: A systematic review of the literature was performed including studies where intra abdominal infections were treated laparoscopically.
RESULTS: Early laparoscopic approaches have become the standard surgical technique for treating acute cholecystitis. The laparoscopic appendectomy has been demonstrated to be superior to open surgery in acute appendicitis. In the event of diverticulitis, laparoscopic resections have proven to be safe and effective procedures for experienced laparoscopic surgeons and may be performed without adversely affecting morbidity and mortality rates. However laparoscopic resection has not been accepted by the medical community as the primary treatment of choice. In high-risk patients, laparoscopic approach may be used for exploration or peritoneal lavage and drainage. The successful laparoscopic repair of perforated peptic ulcers for experienced surgeons, is demonstrated to be safe and effective. Regarding small bowel perforations, comparative studies contrasting open and laparoscopic surgeries have not yet been conducted. Successful laparoscopic resections addressing iatrogenic colonic perforation have been reported despite a lack of literature-based evidence supporting such procedures. In post-operative infections, laparoscopic approaches may be useful in preventing diagnostic delay and controlling the source.
CONCLUSION: Laparoscopy has a good diagnostic accuracy and enables to better identify the causative pathology; laparoscopy may be recommended for the treatment of many intra-abdominal infections.
Core tip: Laparoscopic procedures have become widely accepted as a primary means of diagnosing and treating intra-abdominal infections (IAIs). The diagnostic accuracy of laparoscopy enables surgeons to better identify the causative pathology of acute abdominal pain, and related procedures can be employed to effectively treat a variety of IAIs. Depending on the patient’s symptoms, pathological severity, and the attending surgeon’s personal experience, laparoscopy may be recommended for the treatment of many IAIs.
- Citation: Coccolini F, Tranà C, Sartelli M, Catena F, Saverio SD, Manfredi R, Montori G, Ceresoli M, Falcone C, Ansaloni L. Laparoscopic management of intra-abdominal infections: Systematic review of the literature. World J Gastrointest Surg 2015; 7(8): 160-169
- URL: https://www.wjgnet.com/1948-9366/full/v7/i8/160.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i8.160
Intra-abdominal infections (IAIs) include a variety of pathological conditions, ranging from uncomplicated appendicitis to fecal peritonitis. IAIs are subcategorized in 2 groups: uncomplicated and complicated IAIs[1]. In the event of an uncomplicated case of IAI, the infection involves a single organ and does not spread to the peritoneum. Patients with such infections can be treated with either surgical intervention or antibiotics.
When the infection is effectively resolved by means of surgery, a 24-h regimen of perioperative antibiotics is typically sufficient. In the event of complicated IAI, the infectious process proceeds beyond a single organ, causing either localized or diffuse peritonitis. The treatment of patients with complicated IAIs involves both surgical and antibiotic therapy[1]. Source control action encompasses all measures taken to eliminate the abdominal source of infection and to control ongoing intra-abdominal contamination. Control of the source of infection can be achieved by either operative or non-operative means. The percutaneous drainage of abscesses is an important non-operative interventional procedure. However, surgery remains the undisputed cornerstone of treatment for IAIs. Surgery may be required depending on the underlying pathology and the type and severity of the intra-abdominal infection. Surgical source control may entail resection or suture of diseased or perforated viscera (e.g., diverticular perforation, gastro-duodenal perforation), removal of the infected organ (e.g., appendix, gall bladder), or drainage of abscesses inaccessible by means of percutaneous drainage. Source control typically involves debridement, which is essential for the removal of infected or necrotic tissue.
Laparoscopic procedures have become widely accepted by the medical community as a primary means of diagnosing and treating IAIs.
For patients with complicated IAIs, the laparoscopic approach is an extremely useful technique, particularly for diagnosing uncertain cases[2].
Depending on the anatomical source of infection and the attending surgeon’s experience, laparoscopy may be recommended for the treatment of many IAIs. The aim of the present systematic review is to evaluate the role of laparoscopy in the management of the different causes of complicated IAIs.
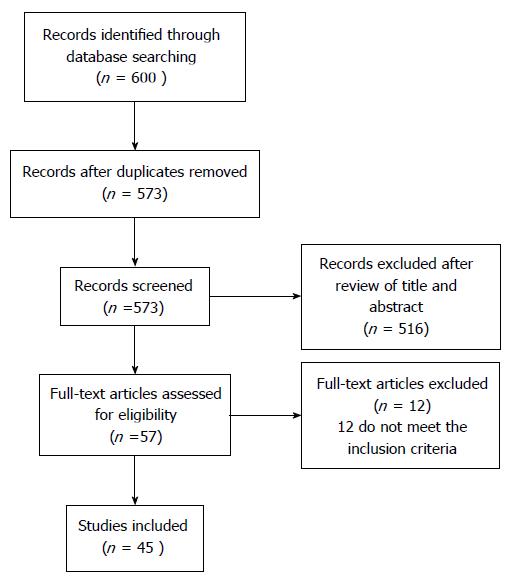
Electronic searches were performed using MEDLINE, EMBASE (1988-2014), PubMed (January 1980-December 2014), Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews and CINAHL from (1966-2014). The search terms were: “appendicitis”, “diverticulitis”, “perforation”, “laparoscopy”, “intra-abdominal”, “infection”, “management” combined with AND/OR. Research included also all the MeSH Terms. No search restrictions were imposed. Progressive filters have been introduced in the research strategy in order to focalize on the highest level of evidence existing articles (i.e., from meta-analysis to case series and case reports). The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. Narrative review articles were also obtained to determine other possible studies. Duplicate published trials with accumulating numbers of patients or increased lengths of follow-up, were considered only in the last or at least in the more complete version (Figure 1).
Studies which have been judged eligible for this systematic review are those in which patients with IAIs from different causes have been treated with laparoscopic approach. Eligibility for study inclusion into the systematic review and study quality assessment were performed independently by two authors (FeCo, FC). Discrepancies between the two investigators were resolved by discussion.
Level of evidence definition was provided according to Oxford Classification (2011).
From the research a total of 600 studies were found. Among these papers 45 were selected for the inclusion in the systematic review.
Laparoscopic cholecystectomy have been widely accepted by the medical community as a safe and effective means of treating acute cholecystitis (AC). About the topic several randomized trials and meta-analysis exist.
The “laparoscopic vs open cholecystectomy” debate has been extensively investigated in the past two decades by researchers and clinicians worldwide. In the early 1990s, laparoscopic management techniques for AC were considered highly controversial; however, by today’s standards, the laparoscopic cholecystectomy is widely accepted as a safe and effective treatment for AC.
Several randomized trials have demonstrated the safety and efficacy of laparoscopic cholecystectomies in treating AC[3-8].
In 1998, Kiviluoto et al[3] published the first randomized trial investigating laparoscopic vs open cholecystectomies in the treatment of both acute and gangrenous cholecystitis.
In the Kiviluoto randomized clinical trial, no deaths or bile-duct lesions were reported in both groups, but the post-operative complication rate was significantly higher (P = 0.0048) for the open cholecystectomy (OC) group than it was for the laparoscopic cholecystectomy (LC) group. Seven patients (23%) experienced major complications and six patients (19%) experienced minor complications following OC; by contrast, no patients experienced major complications and only one patient (3%) experienced minor complications following LC. The post-operative hospital stay was significantly shorter for the LC group than it was for the OC group [median 4 (IQR 2-5) d vs 6 (IQR 5-8) d; P = 0.0063].
An additional randomized controlled trial was published in 2005 by Johansson et al[4]. This study did not report any statistically significant differences between the laparoscopic and open groups in terms of rate of post-operative complications, pain score at time of discharge, or overall sick leave. For eight patients, laparoscopic interventions were converted mid-procedure to OC. The median operating time was 90 min (range 30-155 min) and 80 min (range 50-170 min) for the laparoscopic and open groups, respectively (P = 0.040). The direct medical costs were equivalent for the two groups. Although the median post-operative hospital stay was 2 d in each group, it was significantly shorter for the laparoscopic group (P = 0.011).
Common bile injuries occurring during laparoscopic cholecystectomy for AC remain the most serious complication associated with this procedure. At the beginning of the so-called “laparoscopic era”, several studies reported alarmingly high rates of common bile duct injuries, but this rate decreased dramatically as the modern surgeon began to hone and fine-tune laparoscopic techniques[6,9-15].
In 2008, Borzellino et al[16] published a detailed meta-analysis compiling the results of laparoscopic cholecystectomy in the treatment of severe AC.
Seven studies with a total of 1408 patients who had undergone laparoscopic cholecystectomy were assessed in the meta-analysis. The risks of conversion (RR = 3.2, 95%CI: 2.5-4.2) and overall post-operative complications (RR = 1.6, 95%CI: 1.2-2.2) were significantly higher for cases of severe AC than they were for the non-severe acute forms. However, no differences were reported in terms of local post-operative complications. The authors concluded that laparoscopic cholecystectomies are less effective in treating severe AC (gangrenous or empyematous cholecystitis) than they are in treating less severe forms. A lower threshold of conversion was recommended in order to reduce the likelihood and intensity of local post-operative complications.
In 2014, Catena et al[17] published the results from the ACTIVE trial. 144 consecutive patients were randomly assigned to receive either OC or LC for AC. The two groups were homogeneous. Seven patients (9.7%) required conversion to OC. There were no deaths or bile duct lesions in either group, and the postoperative complication rate was similar (P = NS). The mean postoperative hospital stay was also comparable. Authors concluded that even though LC for acute and gangrenous cholecystitis is technically demanding, in experienced hands it is safe and effective. It does not increase the mortality and the morbidity rate with a low conversion rate and no difference in hospital stay.
The other question widely debated regarding the surgical treatment of AC concerns the timing.
There is strong evidence to support[18-21] that, compared to delayed laparoscopic cholecystectomies, early laparoscopic cholecystectomies for AC reduce both the duration of hospitalization and the risk of readmission due to recurrent AC.
Gurusamy et al[18] recently published a meta-analysis of randomized clinical trials contrasting early laparoscopic cholecystectomies (performed within 1 wk of onset of symptoms) with delayed laparoscopic cholecystectomies (performed at least 6 wk after the first onset of symptoms) in the treatment of AC. Five trials involving 451 patients were included in the study. In the resulting meta-analysis, no statistically significant differences were reported between the two groups regarding either bile duct injury or conversion to OC. The early laparoscopic cholecystectomy group featured a shorter overall hospital stay by 4 d.
The last published randomized controlled trial by Gutt et al[22] compared the immediate laparoscopic cholecystectomy (within 24 h from the admission) (ILC) and the initial antibiotic treatment, followed by delayed laparoscopic cholecystectomy at days 7 to 45 (DLC) in 618 patients. All patients were treated with moxifloxacin for at least 48 h. The primary endpoint was the occurrence of relevant morbidity within 75 d. Secondary endpoints were: 75-d morbidity, conversion rate, change of antibiotic therapy, mortality, costs and length of hospital stay. The trial showed as morbidity rate was significantly lower in group ILC (304 patients) than in group DLC (314 patients): 11.8% vs 34.4%. The conversion rate to open surgery and mortality did not differ significantly between the two groups. The mean length of hospital stay (5.4 d vs 10.0 d; P < 0.001) and total hospital costs (€2919 vs€4262; P < 0.001) were significantly lower in group ILC. Authors concluded that laparoscopic cholecystectomy within 24 h since hospital admission has shown to be superior to the conservative approach concerning morbidity and costs. Moreover authors believe that ILC cholecystectomy should become therapy of choice for AC in operable patients.
A recently published meta-analysis demonstrated that The post-operative morbidity rate was half with LC (OR = 0.46). The post-operative wound infection and pneumonia rates were reduced by LC (OR = 0.54 and 0.51 respectively). The post-operative mortality rate was reduced by LC (OR = 0.2). The mean postoperative hospital stay was significantly shortened in the LC group (MD - 4.74 d). There were no significant differences in the bile leakage rate, intraoperative blood loss and operative times [23].
In order to determine if the treatment delay following the initial onset of symptoms was truly correlated with increased conversion rates in patients with AC, a retrospective case study review of patients undergoing emergency cholecystectomies in a single treatment centre in the 4-year period between January 2002 and December 2005 was conducted[24]. Early intervention for AC (preferably within 2 d of initial onset of symptoms) was the most important criterion for a successful laparoscopic cholecystectomy; treatment delays were associated with a higher likelihood of mid-procedure conversion from laparoscopic to open surgery.
In conclusion, in AC cholecystectomy should be attempted laparoscopically at first (Level of Evidence 1).
Acute appendicitis (AA) is the most common intra-abdominal condition requiring emergency surgery. Although antibiotic treatment has proven to be effective in treating select patients with AA[25-27], appendectomies remain the standard treatment of choice[28].
In recent years, the question of which surgical procedure, laparoscopic or open, is the best way of treating AA has been fiercely debated. Randomized trials and meta-analysis investigating the different surgical means of performing appendectomies have been published in the past 20 years.
In 2010, Li et al[29] published an extensive meta-analysis of randomized controlled trials (1990-2009) comparing laparoscopic (LA) and open appendectomies (OA) in both adults and children in the 19-year period from. Forty-four randomized controlled trials involving 5292 patients were included in the meta-analysis. Authors found that operating time was 12.35 min longer for LA (95%CI: 7.99-16.72). Hospital stay after LA was 0.6 d shorter (95%CI: -0.85 to 0.36). Patients returned to their normal activity 4.52 d earlier after LA (95%CI: -5.95 to 3.10), and resumed their diet 0.34 d earlier (95%CI: -0.46 to 0.21). Pain after LA on the first postoperative day was significantly less. The overall conversion rate from LA to OA was 9.51%. With regard to the rate of complications, wound infection after LA was definitely reduced (OR = 0.45, 95%CI: 0.34-0.59), while postoperative ileus was not significantly reduced (OR = 0.91, 95%CI: 0.57-1.47). However, intra-abdominal abscess, intraoperative bleeding and urinary tract infection after LA, occurred slightly more frequently (OR = 1.56, 95%CI: 1.01-2.43; OR = 1.56, 95%CI: 0.54-4.48 and OR = 1.76, 95%CI: 0.58-5.29 respectively). Authors concluded that LA provides considerable benefits over OA.
Wei et al[30] in 2011 published another meta-analysis analysing 25 RCTs involving 4694 patients (2220 LA and 2474 OA cases). LA showed fewer postoperative complications (OR = 0.74; 95%CI: 0.55-0.98), less pain [length of analgesia: weighted mean difference (WMD), -0.53; 95%CI: -0.91 to -0.15, earlier start of liquid diet (WMD, -0.51; 95%CI: -0.75 to -0.28)], shorter hospital stay (WMD, -0.68; 95%CI: -1.02 to -0.35), and earlier return to work (WMD, -3.09; 95%CI: -5.22 to -0.97) and normal activity (WMD, -4.73; 95%CI: -6.54-12.92). In term of hospital costs the two techniques seemed comparable. LA demonstrated to need longer operative time (WMD, 10.71; 95%CI: 6.76-14.66). Authors concluded that LA is an effective and safe procedure for AA.
Ohtani et al[31] in 2012 published the last meta-analysis reporting results from 39 randomized controlled trials (1990-2012) that compared LA with OA for AA. This meta-analysis included 5896 patients with AA: 2847 had undergone LA, and 3049 had undergone OA. LA was associated with longer operative time (by 13.12 min, 95%CI: 9.72-16.61). As a counterpart, it was associated with earlier resumption of liquid and solid intake, shorter duration of postoperative hospital stay, a reduction in dose numbers of parenteral and oral analgesics, an earlier return to normal activity, work, and normal life, a decreased occurrence of wound infection (OR = 0.44; 95%CI: 0.32-0.60), a better cosmesis and similar hospital charges. Authors concluded that laparoscopic surgery may now be the standard treatment for AA.
From the literature analysis appears that LA has proven to be superior to OA. LA was, however, associated with a slightly increased rate of incidence of intra-abdominal abscesses, intra-operative bleeding, and urinary tract infections. Moreover the use of laparoscopic appendectomy should be used carefully in pregnant women. A systematic review of twenty eight articles (2008) documenting 637 cases of LA in pregnancy were included. The authors concluded that laparoscopic appendectomy in pregnancy is associated with a low rate of intra operative complications in all trimesters. However, LA in pregnancy is associated with a significantly higher rate of fetal loss compared to OA. Rates of preterm delivery appear similar or slightly better following a laparoscopic approach. According to the revised data authors suggested that OA would appear to be the safer option for pregnant women for whom surgical intervention is indicated[32].
A more recent systematic review (2012) with meta-analysis analysing laparoscopic vs open appendectomy during pregnancy in eleven studies with a total of 3415 women (599 in laparoscopic and 2816 in open group) showed that fetal loss rate was statistically significantly higher in those women who underwent laparoscopy. The pooled relative risk (RR) was 1.91 (95%CI: 1.31-2.77) with no heterogeneity. The pooled RR for preterm labour was not statistically significant. The mean difference in length of hospital stay was -0.49 (-1.76 to -0.78) d. No significant difference was found for wound infection, birth weight, duration of operation or Apgar score[33]. Authors concluded that laparoscopic appendectomy in pregnant women might be associated with a greater risk of fetal loss.
In conclusion, literature evidences demonstrated that the laparoscopic appendectomy is the treatment of choice in the vast majority of patients (Level of evidence 1).
Emergency surgery for colonic diverticular perforations is recommended for patients with large and/or multi-loculated diverticular abscesses inaccessible by means of percutaneous drainage, patients with persistent clinical symptoms following CT-guided percutaneous drainage, and patients presenting with diverticulitis associated with free perforation and purulent or fecal diffuse peritonitis.
When a colectomy is performed to address diverticular disease, a laparoscopic procedure appears to be the most viable approach. Even in the event of complicated diverticular disease, laparoscopic resections have proven to be safe and effective; when performed by experienced surgeons, such procedures do not appear to adversely affect the morbidity and mortality rates. However, in most cases the mainstream medical community does not consider laparoscopic procedures to be the optimal treatment of choice, despite the support of the aforementioned clinical evidence.
Although the intra-operative course for perforated diverticulitis patients undergoing laparoscopic resection may appear challenging, many retrospective studies performed by expert laparoscopic surgery groups have demonstrated at least no significant increase in the duration of surgery or the conversion rate among patients with Hinchey stage I, II, or III disease[34-38].
Furthermore, in situations requiring the use of a Hartmann’s procedure, laparoscopic resection with subsequent laparoscopic colostomy reversal has often been implemented successfully[39].
In 2009, the results of the only existing randomized multicentre controlled trial, the Sigma trial, were published[40]. One hundred and four patients were randomized: 52 to receive laparoscopic sigmoid resection (LSR) and 52 to open sigmoid resection (OSR). The two groups were homogeneous for gender, age, Body Mass Index, ASA grade, comorbid conditions, previous abdominal surgery, and indication for surgery. LSR took significantly longer but caused significantly less blood loss The conversion rate was 19.2%. The mortality rate was 1%. There were significantly more major complications in OSR patients (9.6% vs 25.0%). Minor complication rates were similar (LSR 36.5% vs OSR 38.5%). LSR patients had less pain (Visual Analog Scale 1.6), systemic analgesia requirement, and returned home earlier. The short form-36 questionnaire showed significantly better quality of life for LSR.
In 2013, Mbadiwe et al[41] published a vast retrospective trial including a total of 11981 patients. Patients undergoing laparoscopy experienced significantly lower rates of complications with both primary anastomosis (14% vs 26%) and colostomy (30% vs 37%). The laparoscopic approach was associated with decreased mortality rates for patients undergoing primary anastomosis (0.24% vs 0.79%). At the multivariate analysis the laparoscopic approach was associated with lower postoperative morbidity for patients undergoing primary anastomosis. The reduced risk of death for patients undergoing laparoscopic primary anastomosis (vs open approach) didn’t achieve a statistical significance. A small number of patients underwent laparoscopic colostomy (n = 237, 2.4%), and they did not have a significantly different risk of death. Authors concluded that the laparoscopic approach is associated with lower complication rates compared with the open approach for the surgical treatment of diverticulitis with colonic resection and primary anastomosis.
Lastly the laparoscopic approach for exploration, peritoneal lavage, and drainage has recently been developed as a treatment option for patients with acute perforated diverticulitis. However only a small number of studies have been published to date[42-44]. Two prospective cohort studies, nine retrospective case series and two case reports reporting 231 patients have been published. The majority of patients (77%) had purulent peritonitis (Hinchey III). The laparoscopic peritoneal lavage approach successfully controlled in 95.7% of cases abdominal and systemic sepsis. Mortality was 1.7%, morbidity 10.4%. Four patients (1.7%) received colostomy[42]. In 2010 the Ladies trial protocol has been published about this topic. This is a nationwide multicentre randomised trial on perforated diverticulitis performed in The Netherlands that aims to provide evidence on the merits of laparoscopic lavage and drainage for purulent generalised peritonitis and on them optimal resectional strategy for both purulent and faecal generalised peritonitis (Trial registration: Netherlands Trial Register NTR2037). No results have still been published.
In conclusion, laproscopy in the treatment of acute diverticulitis demonstrated to be a safe and effective procedure (Level of evidence 3).
Colonoscopy or foreign bodies induced iatrogenic perforations are slightly rare and serious complications. Resolution of this condition typically requires segmental colonic resection. In this case, a laparoscopic approach may be ideal in order to minimize the effects of such a complication. Especially if exists the possibility to perform a direct suture of a recent and small perforation[44]. No studies exist about the comparison between the open and laparoscopic repair of iatrogenic foreign bodies colonic perforations. Similarly no prospective studies comparing laparoscopic and open approaches have been conducted, but several retrospective studies have demonstrated that laparoscopic resection is often effective in resolving colonic perforation due to colonoscopy and that it may offer certain clinical advantages over the open procedure[45] (Level of evidence 4).
Gastroduodenal perforations have decreased significantly in recent years due to the widespread use of stress ulcer prophylaxis and other medical therapies for peptic ulcer disease among critically ill patients. Other causes of gastro-duodenal perforation include trauma, neoplasm, foreign body ingestion, or iatrogenic (endoscopic procedures)[46]. No trials exist about the laparoscopic management of post-traumatic, neoplastic, iatrogenic or foreign body due perforations. Literature however reports many studies about the laparoscopic management of perforated peptic ulcer[47].
Although non-operative management is often attempted, in most cases of perforated peptic ulcer the surgery is considered the standard method of source control[48-51].
Several prospective case-control studies have documented the successful laparoscopic repair of perforated gastric and duodenal ulcers. Recently published literature includes a few systematic reviews[52,53], three controlled, randomized trials published in a 10-year period from 1996 to 2009[53-55] compare open and laparoscopic approaches in the treatment of gastroduodenal perforations and one meta-analysis published in 2004[56].
In 2010, Bertleff et al[52] published a literature systematic review investigating laparoscopic corrections of perforated peptic ulcers. Data from 56 papers were extracted and systematically analyzed. The overall conversion rate for laparoscopic procedures addressing perforated peptic ulcers was 12.4%. The perforation diameter appeared to be the most significant factor affecting the rate of conversion. The operating time was significantly longer and the incidence of recurrent leakage at the site of repair significantly higher for the laparoscopic groups. However, laparoscopic patients reported significantly less post-operative pain and exhibited reduced morbidity, less mortality, and shorter hospital stays. The authors concluded that there are solid evidence to support the use of laparoscopic procedures as the primary treatment of choice when addressing perforated peptic ulcers. However, patients 70 years or older with a Boey score of 3 and symptoms persisting longer than 24 h were associated with higher morbidity and mortality rates, and as such, they are typically not viable candidates for laparoscopic procedures.
Lau et al[53] in 1996 published the first randomized trial where 103 patients were randomly assigned to receive either laparoscopic suture repair or laparoscopic suturless repair or open repair or open sutureless repair of perforated peptic ulcers. Laparoscopic repair of perforated peptic ulcer (either sutureless either not) took significantly longer than open repairs (94.3 ± 40.3 min vs 53.7 ± 42.6 min), but the amount of analgesic required after laparoscopic repair was significantly less than in open surgery (median 1 dose vs 3 doses). There was no significant difference in the four groups of patients in terms of duration of nasogastric aspiration, duration of intravenous drip, total hospital stay, time to resume normal diet, visual analogue scale score for pain in the first 24 h after surgery, morbidity, reoperation, and mortality rates[53].
In 2002, Siu et al[54] published the results from another randomized trial where 130 patients with a clinical diagnosis of perforated peptic ulcer were randomly assigned to undergo either open or laparoscopic omental patch repair. Nine patients with a surgical diagnosis other than perforated peptic ulcer were excluded; 121 patients entered the final analysis. The two groups were homogeneous in respect to age, sex, site and size of perforations, and American Society of Anesthesiology classification. Nine patients needed conversion to open technique. The laparoscopic repair group patients required significantly less parenteral analgesics and showed a visual analog pain scores in days 1 and 3 after surgery were significantly lower. Laparoscopic repair required significantly less time than open repair. The median postoperative stay was 6 d in the laparoscopic group vs 7 d in the open group. The laparoscopic group showed a lower chest infections rate. There were two intra-abdominal collections in the laparoscopic group. One patient in the laparoscopic group and three patients in the open group died after surgery[54].
In 2009, Bertleff et al[55] published the results from the last randomized trial where 109 patients with symptoms of perforated peptic ulcer and evidence of air under the diaphragm were scheduled to receive either laparoscopic (52 patients) or open (49 patients) repair. The operating time in the laparoscopy group resulted significantly longer than in the open group (75 min vs 50 min). Differences regarding postoperative dosage of opiates and the visual analog scale (VAS) for pain scoring system were in favor of the laparoscopic procedure. The VAS score on postoperative days 1, 3, and 7 was significant lower in the laparoscopic group. Complications were equally distributed. Hospital stay was also comparable (6.5 d in the laparoscopic vs 8.0 d in the open group)[55].
The only existing meta-analysis published in 2004 by Lau et al[56] in 2004, included 13 studies (658 patients) among which 2 were randomized trials, comparing open and laparoscopic repair in perforated gastro-duodenal peptic ulcers. The overall success rate for laparoscopic repair of perforated peptic ulcer was 84%. Reported rates of conversion to open repair ranged from 0% to 29.1%. Five studies demonstrated a significantly longer operative time for laparoscopic repair, whereas another five trials showed no significant difference. The postoperative assessment of pain score was reported by three studies which showed a lower pain score after laparoscopic repair than after open repair. A significant reduction in the dosage of opiate analgesic required in the laparoscopic group was observed in eight studies. Chest infection was the most common postoperative morbidity. The meta-analyses showed a lower overall chest infection rate after laparoscopic repair (OR = 0.79; 95%CI: 0.38-1.62; P = 0.51). Wound infection was the second most common morbidity after open repair. The meta-analyses showed that laparoscopic repair reduces the wound infection rate (OR = 0.39; 95%CI: 0.16-0.94; P = 0.036). The leakage was more common after laparoscopic repair. The meta-analyses demonstrated a lower leakage rate after open repair (OR = 1.49; 95%CI: 0.53-4.24; P = 0.45). There were no significant difference between open and laparoscopic repair in intra-abdominal collection rate. Prolonged ileus was less common after laparoscopic repair (OR = 0.62; 95%CI: 0.20-1.92; P = 0.41). The reoperation rate after was significantly lower after open repair (OR = 2.52; 95%CI: 1.02-6.20; P = 0.045). The overall mortality rate favored laparoscopic repair (OR = 0.63; 95%CI: 0.34-1.15; P = 0.13)[56].
In conclusion, laparoscopy showed to be safe and effective in treating gastro-duodenal perforations (Level of evidence 1).
Small bowel perforations are more uncommon sources of peritonitis in industrialized nations than they are in less-developed countries. Most small intestinal perforations are a result of undetected intestinal ischemia. Treatment most commonly involves resection of the affected bowel segment. In less-developed countries, small bowel perforations usually accompany enteric fever or intestinal tuberculosis[57].
The laparoscopic management of small bowel perforations has been well documented in retrospective series[58], but studies that systematically compare and contrast this procedure with open surgery especially in intestinal infections are needed (Level of evidence 4).
Post-operative peritonitis is a life-threatening manifestation of IAIs that is characterized by high rates of both subsequent complications and mortality.
The inability to effectively control the septic source is one of the most important factors associated with the high mortality rates[59,60].
Delaying a re-laparotomy for more than 24 h in the event of organ failure results in high mortality rates for patients exhibiting post-operative IAIs.
The value of physical tests and laboratory parameters in diagnosing abdominal sepsis is extremely limited. CT scans are believed to yield the most accurate diagnosis. Early (non-delayed) follow-up surgery appears to be the most viable means of treating post-operative infections[59,60].
The laparoscopic control and treatment of post-operative infections have been well documented in recent literature. The diagnostic accuracy of laparoscopy allows for the successful diagnosis of post-operative complications. A few retrospective studies have demonstrated that the laparoscopic approach may prevent delayed diagnoses for post-operative infections and enable experienced surgeons to better control the post-operative source of infection[61,62] (Level of evidence 4).
Laparoscopic procedures have become widely accepted by the medical community as a primary means of diagnosing and treating IAIs.
The diagnostic accuracy of laparoscopy enables surgeons to better identify the causative pathology of acute abdominal disease, and subsequent procedures can be employed to effectively treat a variety of IAIs. Depending on the patients’ symptoms and clinical conditions, on pathological severity, and on the attending surgeon’s personal experience, laparoscopy may be recommended for the treatment of many IAIs.
Laparoscopy is gaining interest in the field of emergency surgery with several diagnostic and therapeutic possibilities.
Laparoscopic procedures are becoming widely accepted as a primary means of diagnosing and treating intra-abdominal infections (IAIs) but good quality evidences are lacking.
This systematic review provides the best level of evidence available on this topic.
This review provides clearly the status of the art of laparoscopy in intra abdominal infections, suggesting the need of further studies in some specific area.
This is a highly valuable study. It provides the first assessment of laparoscopic therapy for IAIs, and clearly provides a data set for moving the operative management of these infections forward.
P- Reviewer: Solomkin JS S- Editor: Yu J L- Editor: A E- Editor: Jiao XK
| 1. | Pieracci FM, Barie PS. Management of severe sepsis of abdominal origin. Scand J Surg. 2007;96:184-196. [PubMed] |
| 2. | Di Saverio S. Emergency laparoscopy: a new emerging discipline for treating abdominal emergencies attempting to minimize costs and invasiveness and maximize outcomes and patients’ comfort. J Trauma Acute Care Surg. 2014;77:338-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Kiviluoto T, Sirén J, Luukkonen P, Kivilaakso E. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 254] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 4. | Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L. Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg. 2005;92:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 143] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Kum CK, Goh PM, Isaac JR, Tekant Y, Ngoi SS. Laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 1994;81:1651-1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Chau CH, Tang CN, Siu WT, Ha JP, Li MK. Laparoscopic cholecystectomy versus open cholecystectomy in elderly patients with acute cholecystitis: retrospective study. Hong Kong Med J. 2002;8:394-399. [PubMed] |
| 7. | Pessaux P, Regenet N, Tuech JJ, Rouge C, Bergamaschi R, Arnaud JP. Laparoscopic versus open cholecystectomy: a prospective comparative study in the elderly with acute cholecystitis. Surg Laparosc Endosc Percutan Tech. 2001;11:252-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Lujan JA, Parrilla P, Robles R, Marin P, Torralba JA, Garcia-Ayllon J. Laparoscopic cholecystectomy vs open cholecystectomy in the treatment of acute cholecystitis: a prospective study. Arch Surg. 1998;133:173-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 127] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med. 1991;324:1073-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1006] [Cited by in RCA: 918] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 10. | Z’graggen K, Wehrli H, Metzger A, Buehler M, Frei E, Klaiber C. Complications of laparoscopic cholecystectomy in Switzerland. A prospective 3-year study of 10,174 patients. Swiss Association of Laparoscopic and Thoracoscopic Surgery. Surg Endosc. 1998;12:1303-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 110] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Söderlund C, Frozanpor F, Linder S. Bile duct injuries at laparoscopic cholecystectomy: a single-institution prospective study. Acute cholecystitis indicates an increased risk. World J Surg. 2005;29:987-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Adamsen S, Hansen OH, Funch-Jensen P, Schulze S, Stage JG, Wara P. Bile duct injury during laparoscopic cholecystectomy: a prospective nationwide series. J Am Coll Surg. 1997;184:571-578. [PubMed] |
| 13. | Avrutis O, Friedman SJ, Meshoulm J, Haskel L, Adler S. Safety and success of early laparoscopic cholecystectomy for acute cholecystitis. Surg Laparosc Endosc Percutan Tech. 2000;10:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Brodsky A, Matter I, Sabo E, Cohen A, Abrahamson J, Eldar S. Laparoscopic cholecystectomy for acute cholecystitis: can the need for conversion and the probability of complications be predicted? A prospective study. Surg Endosc. 2000;14:755-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Eldar S, Sabo E, Nash E, Abrahamson J, Matter I. Laparoscopic cholecystectomy for acute cholecystitis: prospective trial. World J Surg. 1997;21:540-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 126] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 16. | Borzellino G, Sauerland S, Minicozzi AM, Verlato G, Di Pietrantonj C, de Manzoni G, Cordiano C. Laparoscopic cholecystectomy for severe acute cholecystitis. A meta-analysis of results. Surg Endosc. 2008;22:8-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Catena F, Ansaloni L, Bianchi E, Di Saverio S, Coccolini F, Vallicelli C, Lazzareschi D, Sartelli M, Amaduzzi A, Amaduzz A. The ACTIVE (Acute Cholecystitis Trial Invasive Versus Endoscopic) Study: multicenter randomized, double-blind, controlled trial of laparoscopic versus open surgery for acute cholecystitis. Hepatogastroenterology. 2013;60:1552-1556. [PubMed] |
| 18. | Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010;97:141-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 234] [Article Influence: 15.6] [Reference Citation Analysis (1)] |
| 19. | Siddiqui T, MacDonald A, Chong PS, Jenkins JT. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. 2008;195:40-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 150] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 20. | Lau H, Lo CY, Patil NG, Yuen WK. Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis: a metaanalysis. Surg Endosc. 2006;20:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 171] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 21. | Papi C, Catarci M, D’Ambrosio L, Gili L, Koch M, Grassi GB, Capurso L. Timing of cholecystectomy for acute calculous cholecystitis: a meta-analysis. Am J Gastroenterol. 2004;99:147-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 141] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Gutt CN, Encke J, Köninger J, Harnoss JC, Weigand K, Kipfmüller K, Schunter O, Götze T, Golling MT, Menges M. Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg. 2013;258:385-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 300] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 23. | Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, Leandro G, Montori G, Ceresoli M, Corbella D. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015;18:196-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 248] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 24. | Hadad SM, Vaidya JS, Baker L, Koh HC, Heron TP, Hussain K, Thompson AM. Delay from symptom onset increases the conversion rate in laparoscopic cholecystectomy for acute cholecystitis. World J Surg. 2007;31:1298-101; discussion 1298-101;. [PubMed] |
| 25. | Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96:473-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 355] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 26. | Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, Rex L, Badume I, Granström L. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006;30:1033-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 351] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 27. | Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 284] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 28. | Di Saverio S, Mandrioli M, Sibilio A, Smerieri N, Lombardi R, Catena F, Ansaloni L, Tugnoli G, Masetti M, Jovine E. A cost-effective technique for laparoscopic appendectomy: outcomes and costs of a case-control prospective single-operator study of 112 unselected consecutive cases of complicated acute appendicitis. J Am Coll Surg. 2014;218:e51-e65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 29. | Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X, Liu Y. Laparoscopic versus conventional appendectomy--a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010;10:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 218] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 30. | Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG, Wei HB. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc. 2011;25:1199-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 151] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 31. | Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929-1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 32. | Walsh CA, Tang T, Walsh SR. Laparoscopic versus open appendicectomy in pregnancy: a systematic review. Int J Surg. 2008;6:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 33. | Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg. 2012;99:1470-1478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 34. | Pugliese R, Di Lernia S, Sansonna F, Scandroglio I, Maggioni D, Ferrari C, Costanzi A, Chiara O. Laparoscopic treatment of sigmoid diverticulitis: a retrospective review of 103 cases. Surg Endosc. 2004;18:1344-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Titu LV, Zafar N, Phillips SM, Greenslade GL, Dixon AR. Emergency laparoscopic surgery for complicated diverticular disease. Colorectal Dis. 2009;11:401-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Zapletal C, Woeste G, Bechstein WO, Wullstein C. Laparoscopic sigmoid resections for diverticulitis complicated by abscesses or fistulas. Int J Colorectal Dis. 2007;22:1515-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Letarte F, Hallet J, Drolet S, Charles Grégoire R, Bouchard A, Gagné JP, Thibault C, Bouchard P. Laparoscopic emergency surgery for diverticular disease that failed medical treatment: a valuable option? Results of a retrospective comparative cohort study. Dis Colon Rectum. 2013;56:1395-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Royds J, O’Riordan JM, Eguare E, O’Riordan D, Neary PC. Laparoscopic surgery for complicated diverticular disease: a single-centre experience. Colorectal Dis. 2012;14:1248-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Chouillard E, Maggiori L, Ata T, Jarbaoui S, Rivkine E, Benhaim L, Ghiles E, Etienne JC, Fingerhut A. Laparoscopic two-stage left colonic resection for patients with peritonitis caused by acute diverticulitis. Dis Colon Rectum. 2007;50:1157-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 40. | Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES, Bemelman WA, Heres P, Lacy AM, Engel AF. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg. 2009;249:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 240] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 41. | Mbadiwe T, Obirieze AC, Cornwell EE, Turner P, Fullum TM. Surgical management of complicated diverticulitis: a comparison of the laparoscopic and open approaches. J Am Coll Surg. 2013;216:782-788; discussion 788-790;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 42. | Toorenvliet BR, Swank H, Schoones JW, Hamming JF, Bemelman WA. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a systematic review. Colorectal Dis. 2010;12:862-867. [PubMed] |
| 43. | Alamili M, Gögenur I, Rosenberg J. Acute complicated diverticulitis managed by laparoscopic lavage. Dis Colon Rectum. 2009;52:1345-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 44. | Brown CV. Small bowel and colon perforation. Surg Clin North Am. 2014;94:471-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 45. | Rotholtz NA, Laporte M, Lencinas S, Bun M, Canelas A, Mezzadri N. Laparoscopic approach to colonic perforation due to colonoscopy. World J Surg. 2010;34:1949-1953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Nirula R. Gastroduodenal perforation. Surg Clin North Am. 2014;94:31-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Di Saverio S, Bassi M, Smerieri N, Masetti M, Ferrara F, Fabbri C, Ansaloni L, Ghersi S, Serenari M, Coccolini F. Diagnosis and treatment of perforated or bleeding peptic ulcers: 2013 WSES position paper. World J Emerg Surg. 2014;9:45. [PubMed] |
| 48. | Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK. A randomized trial of nonoperative treatment for perforated peptic ulcer. N Engl J Med. 1989;320:970-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 158] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 49. | Boey J, Lee NW, Koo J, Lam PH, Wong J, Ong GB. Immediate definitive surgery for perforated duodenal ulcers: a prospective controlled trial. Ann Surg. 1982;196:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 60] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 50. | Millat B, Fingerhut A, Borie F. Surgical treatment of complicated duodenal ulcers: controlled trials. World J Surg. 2000;24:299-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 51. | Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2013;2:CD004778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 52. | Bertleff MJ, Lange JF. Laparoscopic correction of perforated peptic ulcer: first choice? A review of literature. Surg Endosc. 2010;24:1231-1239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 105] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 53. | Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ, Chung SC, Li AK. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996;224:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 189] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 54. | Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, Tai YP, Li MK. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002;235:313-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 196] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 55. | Bertleff MJ, Halm JA, Bemelman WA, van der Ham AC, van der Harst E, Oei HI, Smulders JF, Steyerberg EW, Lange JF. Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg. 2009;33:1368-1373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 56. | Lau H. Laparoscopic repair of perforated peptic ulcer: a meta-analysis. Surg Endosc. 2004;18:1013-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 90] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 57. | Coccolini F, Ansaloni L, Catena F, Lazzareschi D, Puviani L, Pinna AD. Tubercular bowel perforation: what to do? Ulus Travma Acil Cerrahi Derg. 2011;17:66-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 58. | Sinha R, Sharma N, Joshi M. Laparoscopic repair of small bowel perforation. JSLS. 2009;9:399-402. [PubMed] |
| 59. | Torer N, Yorganci K, Elker D, Sayek I. Prognostic factors of the mortality of postoperative intraabdominal infections. Infection. 2010;38:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 60. | Mulier S, Penninckx F, Verwaest C, Filez L, Aerts R, Fieuws S, Lauwers P. Factors affecting mortality in generalized postoperative peritonitis: multivariate analysis in 96 patients. World J Surg. 2003;27:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 111] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 61. | Rosin D, Zmora O, Khaikin M, Bar Zakai B, Ayalon A, Shabtai M. Laparoscopic management of surgical complications after a recent laparotomy. Surg Endosc. 2004;18:994-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 62. | Kirshtein B, Domchik S, Mizrahi S, Lantsberg L. Laparoscopic diagnosis and treatment of postoperative complications. Am J Surg. 2009;197:19-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |