Published online Jun 27, 2015. doi: 10.4240/wjgs.v7.i6.98
Peer-review started: December 7, 2014
First decision: February 7, 2015
Revised: April 16, 2015
Accepted: May 5, 2015
Article in press: May 6, 2015
Published online: June 27, 2015
Processing time: 299 Days and 12.6 Hours
Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal tumour of gastro-intestinal tract. Annual incidence of GIST in United States is approximately 3000-4000. Clinical presentation of GIST varies with location and size of tumour but GIST presenting with palpable abdominal mass is rare. We report a case of 38 years old male who presented with large abdominal lump. Computed tomography (CT) scan showed a large solid-cystic lesion encasing second part of duodenum and distal common bile duct. On CT differential diagnosis of Leiomyoma, Leiomyosarcoma and GIST were made. The diagnosis of GIST was confirmed by immune-histochemical study of the biopsy material. Patient underwent pancreaticodudenectomy. Post-operative course was uneventful. Patient was started on Imatinib therapy post-operatively. No recurrence noted at six months follow up.
Core tip: Gastrointestinal stromal tumours presenting with palpable abdominal mass are rare. Diagnosis is based upon histopathology and immunehistochemistry. Pre operatively patient should be evaluated with different modalities for diagnosis and resectability of tumour. Surgical resection with postoperative Imatinib chemotherapy helps to provide long term survival.
- Citation: Bhambare MR, Pandya JS, Waghmare SB, Shetty TS. Gastrointestinal stromal tumour presenting as palpable abdominal mass: A rare entity. World J Gastrointest Surg 2015; 7(6): 98-101
- URL: https://www.wjgnet.com/1948-9366/full/v7/i6/98.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i6.98
Gastro-intestinal stromal tumour (GIST) is the most common primary mesenchymal tumour of gastro-intestinal tract arising from interstitial cell of Cajal or their stem cell precursor[1,2]. The incidence of GIST in United States is approximately 3000-4000 annually[1,2]. GISTs generally arise in stomach (60%-70%), small intestine (25%-35%), rectum and colon (5%-10%), duodenum (4%) mesentry or omentum (7%) and oesophagus (5%)[2]. They commonly affect men with median age of presentation being 55-60 years[3]. Pre-operative diagnosis is difficult due to its non-specific signs and symptoms. GISTs presents commonly as abdominal pain and bleeding. GISTs presenting with palpable abdominal mass is rare[4]. Only 25 such cases have been published in world literature from 2001 to 2011[4]. We report a case of GIST presenting as a large abdominal mass. Computed tomography (CT) abdomen showed a large solid cystic lesion encasing second part of duodenum, and distal common bile duct (CBD) causing its dilatation. Ultrasonography guided biopsy was taken to aid the diagnosis which was confirmed by Histo-pathological and immune-histochemical study. Patient underwent pancreaticodudenectomy. Post-operative course was uneventful. Patient was started on Imatinib post-operatively. No clinical and radiological recurrence noted at six month follow up.
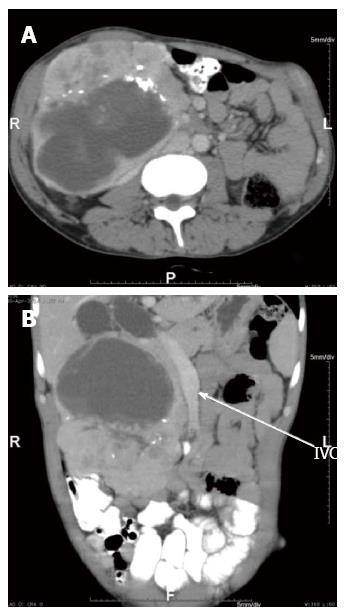
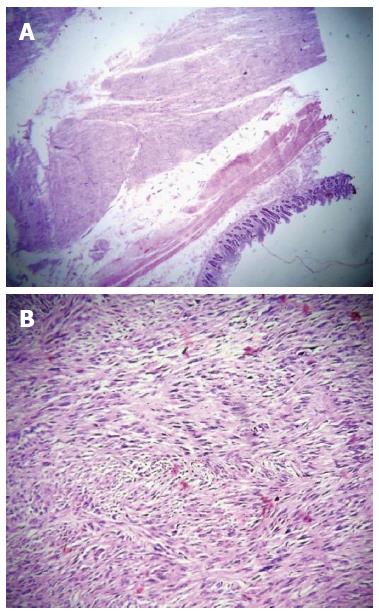
A 38-year-old male presented with lump in abdomen of seven years duration,gradually increasing in size associated with intermittent, non-radiating dull aching pain. On abdominal examination a 14 cm × 12 cm firm to hard lump was palpable in epigastric, right hypochondriac, right lumbar region. Systemic examination showed no distant or lymph node metastasis. CT scan of abdomen showed a large solid cystic mass with lobulated margin measuring 14.8 cm × 11.4 cm × 11.2 cm in right hypochondriac and right lumbar region. It showed amorphous calcification with heterogenous enhancing solid component and septae within cystic areas. Mass appeared to be encasing duodenum and distal bile duct causing dilatation of proximal CBD and IHBRD (Figure 1). The diffential diagnosis based on CT Abdomen was leiomyoma, leiomyosarcoma and GIST. The patient underwent USG-guided biopsy of the tumour (Figure 2). Microscopically, the tumour section showed proliferation of non-specific monomorphic spindle cells and small mesenchymal cells. Mitotic figures and atypical cells were occasionally observed (< 5/50 high-power fields).
On Immunohistochemistry the tumour was positive for Ckit, DOG 1 and SMA whereas it was negative for Desmin and S100.
On exploratory laparotomy through roof top incision a huge mass of 14 cm × 15 cm × 11 cm was found encasing second part of duodenum and adherent to head of pancreas. There was dilatation of CBD. Pancreatico-duodenectomy with en-block resection of mass done (Figure 3). The tumour capsule was intact. Intra-operative and post-operative course was uneventful. Histopathological study revealed GIST of duodenal origin with < 5 mitosis/50 high power field and low to moderate malignant potential. All resection margins were free of tumour (R0). Tablet Imatinib 400 mg was started post-operatively. No clinical and radiological recurrence noted at six month follow up.
GISTs are the most common mesenchymal tumours of gastrointestinal tract, first described by Clarke and Mazur[1,2] in 1983. GISTs are derived from the interstitial cells of Cajal which serves as pace maker of gastrointestinal tract triggering smooth muscle contraction[1,2]. There is male preponderance and peak age is fifth and sixth decade[3].
GISTs are commonly seen in stomach (60%-70%) and rarely in duodenum (4%)[2]. GISTs are characterised by genetic expression of c-kit (a trans-membrane tyrosine kinase receptor) and immune-histo-chemical staining of CD 117, CD34 (70%), SMA (40%) and a novel gene DOG1[2,5].
GISTs are spread by heterogenous route to liver and peritoneum[6] and rarely to lung, bone, lymph nodes.
Pre-operative diagnosis of GIST is difficult as the patient presents with non-specific signs and symptoms[4]. Pain in abdomen and GI bleed being the most common presentation mentioned in the literature[4]. However, patient presenting with palpable abdominal mass is very rare and only 25 cases have been reported[4]. Pre-operative CT Scan and MRI although of not much aid to locate the origin of the tumour, helps in deciding the resectability of the tumour and metastasis[4]. The basic modality of tumour treatment for GIST is surgery with complete removal of the tumour and microscopic negative margins (Ro resection)[4,6].
Recurrence rate of about 40% is reported in patients undergoing complete resection. Most common site of recurrence being local and liver mets[6]. Imatinib has played an important role in neo-adjuvant therapy as well as recurrent disease[2]. In case of advanced disease or resistance/tolerance to imatinib,a newer drug Sunitinib is used as a second line therapy[2].
Prognosis of tumour depends mainly upon size, location and mitotic index[2]. Other important factors are age of presentation, histopathological and immunohistochemistry features and molecular genetics. Poor prognosis is associated with tumours > 5 cm in size and > 5 mitosis per HPF[2].
PET CT is particularly useful auxillary diagnostic modality as baseline for verification of the early response to therapy with Imatinib, aTKI[7]. Literature mentions five year survival rate as 30% and it increases to 54% after complete surgical resection with microscopic negative margins[8].
A 38-year-old male presented with lump in abdomen of seven years duration, gradually increasing in size associated with intermittent, non-radiating dull aching pain.
Physical examination showed firm to hard lump in epigastric, right hypochondriac and lumbar region with no evidence of metastasis.
Hepatoma, malignancy of stomach, lymphoma, gastrointestinal stromal tumours (GIST).
Haemoglobin, haematocrit, liver function test, renal function test were within normal range.
Computed tomography scan of abdomen showed a large solid cystic mass with lobulated margin measuring 14.8 cm × 11.4 cm × 11.2 cm in right hypochondriac and right lumbar region with amorphous calcification, heterogenous enhancing solid component and encasing duodenum and distal bile duct causing dilatation of proximal common bile duct and IHBRD.
USG-guided biopsy of the tumour showed proliferation of non-specific monomorphic spindle cells and small mesenchymal cells. Mitotic figures (< 5/50 high-power fields). Immunohistochemistry of the tumour was positive for C-kit, DOG 1 and SMA whereas it was negative for Desmin and S100.
Pancreatico-duodenectomy with adjuvant imatinib chemotherapy.
Only 25 such cases have been published in world literature from 2001 to 2011.
GISTs are the most common mesenchymal tumour of gastrointestinal tract.
The diffential diagnosis of GIST should be kept in mind while dealing with palpable abdominal mass.
The manuscript presents a case report of a very large GIST of duodenal origin.
P- Reviewer: Topaloglu S, Widmann G S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Dematteo RP, Ballman KV, Antonescu CR, Maki RG, Pisters PW, Demetri GD, Blackstein ME, Blanke CD, von Mehren M, Brennan MF. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;373:1097-1104. |
| 2. | Tan CB, Zhi W, Shahzad G, Mustacchia P. Gastrointestinal stromal tumors: a review of case reports, diagnosis, treatment, and future directions. ISRN Gastroenterol. 2012;2012:595968. |
| 3. | Laperouse P, Raines D, Diamond K, Rivera S, Newman W, Hew AY, Lopez FA. Gastrointestinal stromal tumors: a case report and review of the literature. J La State Med Soc. 2008;160:128-33; quiz 134. |
| 4. | Patil S, Jain S, Kaza RC, Chamberlain RS. Giant gastrointestinal stromal tumor presenting as a palpable abdominal mass: an unusual presentation. ISRN Surg. 2011;2011:894829. |
| 5. | Dorfman DM, Bui MM, Tubbs RR, Hsi ED, Fitzgibbons PL, Linden MD, Rickert RR, Roche PC. The CD117 immunohistochemistry tissue microarray survey for quality assurance and interlaboratory comparison: a College of American Pathologists Cell Markers Committee Study. Arch Pathol Lab Med. 2006;130:779-782. |
| 6. | Miettinen M, Kopczynski J, Makhlouf HR, Sarlomo-Rikala M, Gyorffy H, Burke A, Sobin LH, Lasota J. Gastrointestinal stromal tumors, intramural leiomyomas, and leiomyosarcomas in the duodenum: a clinicopathologic, immunohistochemical, and molecular genetic study of 167 cases. Am J Surg Pathol. 2003;27:625-641. |
| 7. | Sornmayura P. Gastrointestinal stromal tumors (GISTs): a pathology view point. J Med Assoc Thai. 2009;92:124-135. |