Published online May 27, 2015. doi: 10.4240/wjgs.v7.i5.78
Peer-review started: September 4, 2014
First decision: February 7, 2015
Revised: February 23, 2015
Accepted: March 16, 2015
Article in press: March 18, 2015
Published online: May 27, 2015
Processing time: 258 Days and 0.2 Hours
Segmental arterial mediolysis (SAM) is characterized by intra-abdominal, retroperitoneal bleeding or bowel ischemia, and the etiology is unknown. A 44-year-old man complaining of abdominal pain was admitted to our hospital. He had been admitted for a left renal infarction three days earlier and had a past medical history of cerebral aneurysm with spontaneous remission. The ruptured site of the splenic arterial aneurysm was clear via a celiac angiography, and we treated it using trans-arterial embolization. Unfortunately, the aneurysm reruptured after two weeks, and we successfully treated it with distal pancreatomy and splenectomy. We recommended a close follow-up and prompt radiological or surgical intervention because SAM can enlarge rapidly and rupture.
Core tip: Segmental arterial mediolysis (SAM) related to intra-abdominal, retroperitoneal bleeding or bowel ischemia has a mortality approaching 25%-50%. We treated the splenic artery aneurismal re-rupture associated with SAM after trans-catheter arterial embolization with a distal pancreatomy and splenectomy. We recommend close follow-ups and prompt radiological or surgical intervention because SAM can increase rapidly and rupture.
- Citation: Matsuda Y, Sakamoto K, Nishino E, Kataoka N, Yamaguchi T, Tomita M, Kazi A, Shinozaki M, Makimoto S. Pancreatectomy and splenectomy for a splenic aneurysm associated with segmental arterial mediolysis. World J Gastrointest Surg 2015; 7(5): 78-81
- URL: https://www.wjgnet.com/1948-9366/full/v7/i5/78.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i5.78
The first case of a distinct arterial lesion in the large abdominal muscular arteries was described by Slavin et al[1] in 1976 and was termed segmental arterial mediolysis (SAM) in 1995[1,2]. Alterations of SAM stem from two separate lesions: mediolysis and a tear that separates the outer medial muscle from the adventitia[3]. As a result, sudden hemorrhage due to an aneurysm rupture or dissection occurs in the abdomen, retroperitoneum, or brain[3,4]. Cases of SAM that are complicated by intra-abdominal hemorrhage have mortality rates approaching 25%-50%[5,6]. In this report, we present a case of SAM, which was associated with trans-arterial embolization (TAE) and surgical resection for a splenic artery aneurysm that had enlarged rapidly within a short time period.
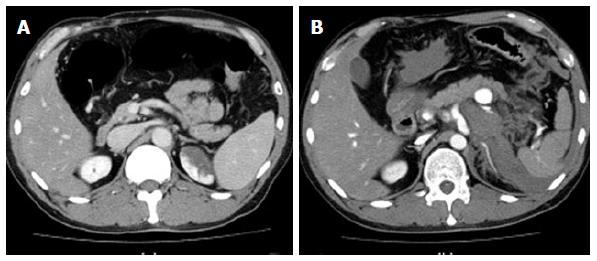
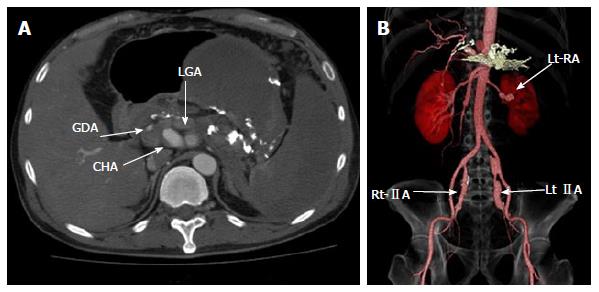
A 44-year-old man had been previously admitted to the hospital for treatment of a left renal infarction. He was received balloon angioplasty because the ventral branch of the left renal artery had been dissected. Three day after hospital discharge, he returned to the hospital due to complaints of abdominal pain. The pain gradually worsened after discharge. This patient had a past medical history of cerebral aneurysm with spontaneous remission (with no family history). When he arrived, his vital signs indicated hypotension (96/62 mmHg); normal sinus rhythm (81 beats/min); and normal body temperature (36.9 °C). A physical examination revealed only abdominal tenderness. The laboratory findings indicated inflammation (white blood cell count: 13300/μL, C-reactive protein: 3.133 mg/dL) and no anemia (hemoglobin: 14.4 g/dL, hematocrit: 40.4%). Enhanced computed tomography (CT) demonstrated a 20 mm aneurysm of the splenic artery with extravasation and hematoma accumulated around the retroperitoneum (Figure 1). In addition, the CT scan revealed other aneurysms, which had a string of beads appearance, in the common hepatic, left gastric, gastroduodenal, left renal, and both internal iliac arteries. These aneurysms were not present two weeks earlier (Figure 2).
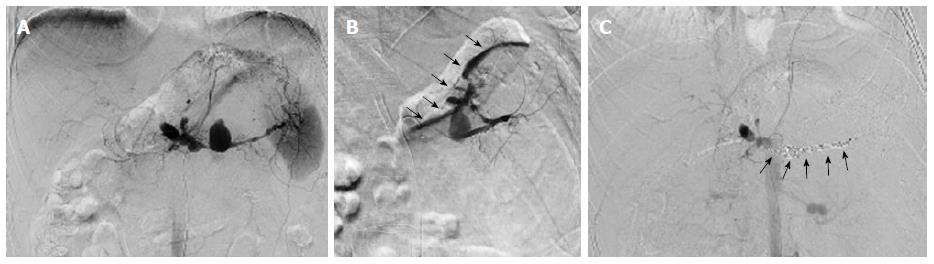
We confirmed the ruptured site of the splenic arterial aneurysm via celiac angiography. The microcatheter was inserted at the distal site of the aneurysm, and the ruptured aneurysm was successfully managed by TAE. After the intervention, the aneurysm was not enhanced, and surgical treatment was avoided (Figure 3). After TAE, we followed up the aneurysms via enhanced CT scanning, and there was no extravasation or enlargement. Unfortunately, this patient had abdominal pain again two weeks later because the aneurysm re-ruptured. We performed an emergency operation due to unstable vital signs. Additionally, he underwent distal pancreatectomy and splenectomy because the aneurysm was located within the pancreatic body, and the resection of splenic artery was difficult. The postoperative complications included pancreatic fistula and intra-abdominal abscess. On day 9, he was treated with an antimicrobial agent (Vancomycin: 1 g/d) for 10 d because the abscess culture demonstrated coagulase negative staphylococcus. In addition, we performed abscess drainage for 28 d postoperatively. He was discharged 30 d after surgery.
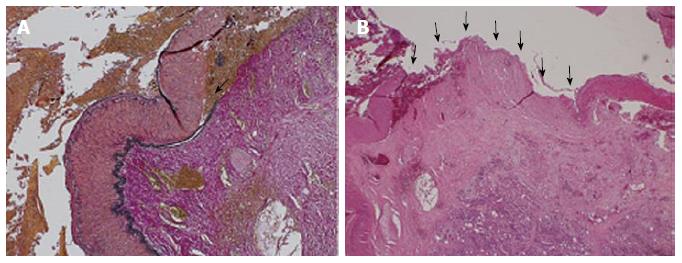
Histopathology revealed an adventitial-medial junction created by separation of the media from the adventitia and organized thrombi deposited at the site. There was no infiltration of inflammatory cells and no arterial sclerosis (Figure 4).
Splanchnic artery aneurysms (SAAs) are relatively rare and most commonly occur in the splenic artery (60%)[7]. Multiple SAAs are very rare (3.6%-15% of patients with visceral aneurysms). When multiple SAAs are present, other disorders, such as SAM, should be suspected[8]. SAM may also be accompanied by coronary arterial lesions or intra-cranial vascular lesions[9]. Michael et al[10] reported that the vascular changes completely vanished after treatment of un-ruptured aneurysms. This patient had 6 SAAs in different sites, and we clinically considered that the previous cerebral aneurysm with spontaneous remission was caused by SAM. Uchiyama et al[11] suggested that clinical criteria were required because some patients are treated with embolization. Nishikawa et al[8] clinically diagnosed their patient with SAM based on the following: (1) multiple SAAs; (2) middle to old age; (3) non-inflammatory, non-atherosclerosis, and non-genetic backgrounds; (4) radiological features demonstrate a bead-like appearance, irregular dilatation and stenosis; and (5) acute vessel remodeling[8].
The differential diagnosis of SAM includes arteriosclerotic disease, infection, connective tissue disorders (e.g., polyarteritis nodosa), congenital disease (e.g., Marfan syndrome), and especially fibromuscular dysplasia (FMD). FMD is primarily observed in young females.
The histological findings in SAM also overlap with FMD. Lie et al[12] proposed that SAM might represent a variant of FMD. Slavin et al[2] suggested that it might represent a precursor to certain types of FMD. They did not wish to imply that all cases of FMD are preceded by SAM and described that SAM demonstrated a partial to total loss of media with replacement fibrosis and remained a non-specific aneurysm[2]. In this patient, the pathological findings revealed an adventitial-medial junction created by the separation of the media from the adventitia. As a result, we diagnosed SAM based on the clinical and pathological findings.
Treatment of SAM involves embolization, surgical bypass, or resection of the injured arteries. Ryan et al[13] described the first case of coil embolization. Since then, successful endovascular management is common, and TAE is successful in 88% of attempted cases with no reported mortality. Only 3 cases have reported unsuccessful outcomes with endovascular treatment requiring open surgical intervention[6]. One case had difficulties in the catheterization, and two cases were hemodynamically unstable. We considered that the angiography did not demonstrate extravasation because our patient was hemodynamically unstable. As a result, endovascular management serves as a reliable, minimally invasive treatment option and may also provide a temporary solution before definitive surgery at a later date[6].
Although SAM related to intra-abdominal, retroperitoneal bleeding or bowel ischemia has a mortality rate approaching 25%-50%[5,6], the surgical intervention for re-rupture after TAE was successful in this patient. SAAs (except splenic artery) are followed up with a short time period because the risk of rupture is low.
In conclusion, close follow-up is necessary for SAAs when SAM is suspected. If necessary, radiological or surgical intervention should be promptly pursued because multiple SAAs associated with SAM may increase rapidly and rupture.
A 44-year-old male with a history of cerebral aneurysm with spontaneous remission had abdominal pain.
Segmental arterial mediolysis (SAM).
Arteriosclerotic disease, infection, connective tissue disorders (e.g., polyarteritis nodosa), congenital disease (e.g., Marfan syndrome), and especially fibromuscular dysplasia.
White blood cell count was 13300/μL and C-reactive protein was 3.133 mg/dL.
Enhanced computed tomography demonstrated a 20 mm aneurysm of the splenic artery with extravasation.
Histopathology revealed an adventitial-medial junction created by separation of the media from the adventitia and organized thrombi deposited at the site.
The authors performed distal pancreatectomy and splenectomy because the aneurysm was located within the pancreatic body, and the resection of splenic artery was difficult.
Rerupture of a splenic artery aneurysm, associated with segmental arterial mediolysis after transcatheter arterial embolization is rare.
SAM stem from mediolysis and a tear that separates the outer medial muscle from the adventitia.
Close follow-up is necessary for splanchnic artery aneurysms when SAM is suspected.
Good management of an unusual situation.
P- Reviewer: Bandyopadhyay SK, Koda K, Lima M, Shelat VG, Shimoyama S, Venskutonis D S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Slavin RE, Gonzalez-Vitale JC. Segmental mediolytic arteritis: a clinical pathologic study. Lab Invest. 1976;35:23-29. [PubMed] |
| 2. | Slavin RE, Saeki K, Bhagavan B, Maas AE. Segmental arterial mediolysis: a precursor to fibromuscular dysplasia. Mod Pathol. 1995;8:287-294. [PubMed] |
| 3. | Slavin RE. Segmental arterial mediolysis: course, sequelae, prognosis, and pathologic-radiologic correlation. Cardiovasc Pathol. 2009;18:352-360. [PubMed] |
| 4. | Inada K, Maeda M, Ikeda T. Segmental arterial mediolysis: unrecognized cases culled from cases of ruptured aneurysm of abdominal visceral arteries reported in the Japanese literature. Pathol Res Pract. 2007;203:771-778. [PubMed] |
| 5. | Sakano T, Morita K, Imaki M, Ueno H. Segmental arterial mediolysis studied by repeated angiography. Br J Radiol. 1997;70:656-658. [PubMed] |
| 6. | Shenouda M, Riga C, Naji Y, Renton S. Segmental arterial mediolysis: a systematic review of 85 cases. Ann Vasc Surg. 2014;28:269-277. [PubMed] |
| 7. | Moore WS. Vascular surgery: a comprehensive review. 3rd ed. Philadelphia, PA: Saunders 1991; . |
| 8. | Nishikawa Y, Hoshina K, Sasaki H, Hosaka A, Yamamoto K, Okamoto H, Shigematsu K, Miyata T. Acute remodeling of an adjoining aneurysm after endovascular treatment of a ruptured splanchnic arterial aneurysm: a case of clinically diagnosed segmental arterial mediolysis. Ann Vasc Dis. 2012;5:449-453. [PubMed] |
| 9. | Ro A, Kageyama N, Takatsu A, Fukunaga T. Segmental arterial mediolysis of varying phases affecting both the intra-abdominal and intracranial vertebral arteries: an autopsy case report. Cardiovasc Pathol. 2010;19:248-251. [PubMed] |
| 10. | Michael M, Widmer U, Wildermuth S, Barghorn A, Duewell S, Pfammatter T. Segmental arterial mediolysis: CTA findings at presentation and follow-up. AJR Am J Roentgenol. 2006;187:1463-1469. [PubMed] |
| 11. | Uchiyama D, Koganemaru M, Abe T, Tomita N, Nonoshita M, Higaki K, Sakamoto T, Hayabuchi N. A case of successful transcatheter arterial embolization for intraabdominal hemorrhage due to suspected segmental mediolytic arteriopathy. Jpn J Intervent Radiol. 2005;20:278-281 Available from: http://www.jsivr.jp/journal/abstract/20_3.html. |
| 12. | Lie JT. Segmental mediolytic arteritis. Not an arteritis but a variant of arterial fibromuscular dysplasia. Arch Pathol Lab Med. 1992;116:238-241. [PubMed] |
| 13. | Ryan JM, Suhocki PV, Smith TP. Coil embolization of segmental arterial mediolysis of the hepatic artery. J Vasc Interv Radiol. 2000;11:865-868. [PubMed] |