Published online Mar 27, 2015. doi: 10.4240/wjgs.v7.i3.43
Peer-review started: October 21, 2014
First decision: December 17, 2014
Revised: January 16, 2015
Accepted: February 9, 2015
Article in press: February 11, 2015
Published online: March 27, 2015
Processing time: 162 Days and 21.3 Hours
An intra-abdominal pseudotumor is a rare complication of hemophilia. Surgical treatment is associated with high morbidity and mortality rates and reported cases are scarce. We present a 66-year-old Caucasian male suffering from severe hemophilia type A treated for 10 years with Factor VIII. Major complications from the disease were chronic hepatitis B and C, cerebral hemorrhage and disabling arthropathy. Twenty-three years ago, retro-peritoneal bleeding led to the development of a large intra-abdominal pseudotumor, which was followed-up clinically due to the high surgical risk and the lack of clinical indication. The patient presented to the emergency department with severe sepsis and umbilical discharge that had appeared over the past two days. Abdominal computed tomography images were highly suggestive of a bowel fistula. The patient was taken to the operating room under continuous infusion of factor VIII. Surgical exploration revealed a large infected pseudotumor with severe intra-abdominal adhesions and a left colonic fistula. The pseudotumor was partially resected en bloc with the left colon leaving the posterior wall intact. The postoperative period was complicated by septic shock and a small bowel fistula that required reoperation. He was discharged on the 73rd hospital day and is well 8 mo after surgery. No bleeding complications were encountered and we consider surgery safe under factor VIII replacement therapy.
Core tip: We present a patient suffering from hemophilia A complicated by a large intra-abdominal hemophilic pseudotumor. This condition is rare and there is no consensus for treatment. Emergency resection was required because of bowel complications and septic shock. Based on our experience, we recommend elective surgery prior to complications under appropriate factor VIII replacement therapy.
- Citation: Frezin J, Marique L, Coubeau L, Hubert C, Lambert C, Hermans C, Jabbour N. Successful emergency resection of a massive intra-abdominal hemophilic pseudotumor. World J Gastrointest Surg 2015; 7(3): 43-46
- URL: https://www.wjgnet.com/1948-9366/full/v7/i3/43.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i3.43
Hemophilia A is a congenital disease with an estimated incidence of 10 to 20 cases for 100000 males[1]. Spontaneous bleeding and hemarthrosis are the most frequent complications. Hemophilic pseudotumors are less common, found in severe cases of hemophilia (1%-2%) and mainly located in the limbs[1,2]. Pseudotumors consist of encapsulated, chronic, slowly expanding hematomas. Abdominal pseudotumors are rare and their management is still controversial. Replacement therapy is often the first therapeutic approach. However, surgery is the most effective and the only definitive treatment[2] even though it is associated to high morbidity and mortality rates[3]. Therapeutic alternatives include radiotherapy, percutaneous drainage, embolization and external radiation[2]. We describe our experience in the surgical management of a large intra-abdominal hemophilic pseudotumor.
Our patient is a 66-year-old Caucasian male with severe hemophila type A complicated by arterial hypertension, chronic hepatitis B and C, a cerebral hemorrhage 20 years ago and many spontaneous bleeding episodes causing disabling diffuse arthropathy. His medical treatment includes recombinant factor VIII concentrate 2000 IU (Refacto AF®, Pfizer) twice a week for the past 10 years, spironolactone 25 mg once a day and painkillers.
At the age of 44, an intra-abdominal bleeding episode led to the development of an intra-abdominal hemophilic pseudotumor, which was treated conservatively as it was asymptomatic. Follow-up by annual abdominal computed tomography (CT) showed stability of the tumor with no sign of complication. A year prior to the current episode, the patient was hospitalized for intra-tumoral bleeding with hemorrhagic shock that responded to conservative treatment.
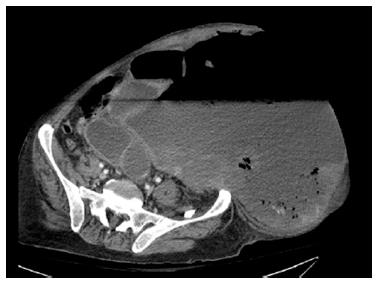
This most recent event started when the patient was admitted to the emergency room for sepsis, recent onset of diarrhea, vomiting and abdominal distension. Physical examination showed abdominal distension without guarding, no bowel sounds and spontaneous fecal discharge from the umbilicus (Figure 1). The laboratory tests were significant for C reactive protein 300.9 mg/L, white blood cell count 17490/L, hemoglobin 10.8 g/dL, platelets 429000/µL, prothrombin time 15.7 s (normal 8.6-13.8 s), factor VIII 59% (after factor VIII replacement). Abdominal CT showed air within the tumor (Figure 2). The patient was brought to the operating room. A bolus of 2000 U factor VIII infusion (Refacto AF®, Pfizer) was given before incision followed by continuous infusion of factor VIII (6000 U per day). Abdominal exploration through a midline incision revealed severe adhesions between the pseudotumor and the small and large bowel. There was no peritonitis. The cyst was filled with stools and old clots and a fistula between the left colon and the tumor was found. Intra-operative management consisted of left hemicolectomy en bloc with the cyst. The posterior cyst wall was left in situ because of involvement of the aorta, inferior vena cava and right ureter. A terminal colostomy was performed, including a Hartmann pouch. Hemostasis was achieved easily. The abdomen was closed after saline irrigation, and 3 drains were left in place. The total operative time was 353 min and the patient was transfused 6 units of red blood cells.
In the immediate postoperative period, the patient was given a continuous infusion of 6000 U/d of factor VIII in order to maintain factor VIII levels between 30% and 40%. On the 3rd postoperative day, he developed a small bowel fistula complicated by intra-abdominal sepsis that required surgical re-exploration. A T-tube was inserted in the fistula site and later served as a feeding jejunostomy.
On the 55th postoperative day, the patient underwent a negative re-exploration because of an inflammatory syndrome with abdominal CT scan findings of portal venous gas and intestinal pneumatosis. He recovered well postoperatively, and quickly resumed enteral feeding. He was discharged to a rehab facility on the 73rd postoperative day.
The patient had no bleeding complication during his hospital stay. Eight months after surgery, he is well.
Hemophilia is a group of inherited blood coagulation disorders. The mutation is located on the X chromosome, therefore only men are afflicted and women are carriers. Depending on the remaining level of factor VIII activity, hemophilia A is classified as mild (> 5%), moderate (1%-5%) or severe (< 1%)[1]. Most common complications are spontaneous bleeding into joints and muscles[4].
Hemophilic pseudotumors are rare complications of hemophilia occurring in approximately 1% to 2% of patients suffering from severe hemophilia[1,2]. The pseudotumor is caused by recurrent bleeding episodes into bone or soft tissue leading to the formation of an encapsulated mass of clotted blood and necrotic tissue. In children, pseudotumors are most likely to occur in the limbs or jaw bone, whilst in adults they predominantly arise in large muscles of the abdomen, pelvis or thigh. They have also been reported to affect the lung, the abdomen or the wall of the stomach[4].
Reports in the literature of patients suffering from intra-abdominal hemophilic pseudotumors are scarce. Reports of successful emergency resections are even scarcer, which makes our case noteworthy. Pseudotumors are painless except during episodes of acute bleeding but can lead to symptoms due to their mass effect[5]. Indeed, as the tumor enlarges, growing pressure on adjacent structures leads to bowel ischemia and/or fistula[5], as described in our case. Erosion into an artery or spontaneous rupture of the tumor can lead to massive bleeding[4].
There is no consensus for the treatment of intra-abdominal hemophilic pseudotumors because of their rarity. Minimizing complications and preserving the function of the affected tissue or organ is the primarily goal. Reluctance to treat surgically is linked to the risk of bleeding. As a result, several other treatment modalities have been attempted, such as radiotherapy, percutaneous drainage, embolization and external radiation[2]. Most authors do not recommend aspiration of the cyst[4]. Indeed, the cyst contents are too thick to permit complete drainage and its aspiration increases the risk of sepsis, relapse or chronic fistula.
When surgery is considered, one should aim for complete resection but it is not possible in all cases. Indeed, both major neurovascular involvement and anatomy distortion caused by the cyst often prevent safe resection[4,5]. Common indications for surgery include evidence of enlargement of the pseudotumor, hemodynamic deterioration or gastro-intestinal complications.
The risk of surgical bleeding can be minimized by judicious administration of factor VIII at induction, during and after surgery under the close supervision of hemophilia specialists. Frequent monitoring to maintain adequate levels of factor VIII makes surgical option safe even when faced with a major hemophilic pseudotumor. In our case, continuous factor VIII replacement therapy was proven effective in preventing bleeding complications during the 3 laparotomies and during the patient's prolonged hospitalization. There are several reports in the literature in favor of surgery in hemophilic patients with continuous or interrupted[1] infusion of clotting factors with minimal risk of hemorrhage.
The particularly large size of the cyst (over 30 cm in diameter) and the duration of its evolution made the resection hazardous in the present patient. The fact that surgical long-term outcome was favorable despite the patient's complications and emergency context should encourage elective resection.
We report a rare case of successful emergency resection of a large abdominal hemophilic pseudotumor. Abdominal surgery in a hemophilic A patient is feasible without hemorrhagic complications under continuous factor VIII replacement therapy. Elective resection of an abdominal hemophilic pseudotumor should be considered prior to the development of major complications.
A hemophilic patient known for a large intra-abdominal hemophilic pseudotumor presenting with abdominal distension, umbilical fecal discharge and vomiting.
Physical examination showed signs of severe sepsis and abdominal distension without guarding.
Peritonitis, intestinal obstruction, pseudotumor infection, bowel fistula.
C reactive-protein (300.9 mg/L), white count (17490/L), hemoglobin (10.8 g/dL), platelets (429000/μL), prothrombin time (15.7 s), factor VIII (59%).
Abdominal computed tomography showed air within the pseudotumor.
Pathological analysis of the surgical specimen confirmed the diagnosis of large bowel fistula into the hemophilic pseudotumor.
Emergency exploratory laparotomy was performed. The pseudotumor was resected en bloc with the left colon because of the presence of a large bowel fistula.
Few cases of successful resection of intra-abdominal hemophilic pseudotumors have been reported. The treatment of those tumors is still controversial.
A hemophilic pseudotumor is a chronic slowly expanding hematoma. An intra-abdominal hemophilic pseudotumor can lead to severe complications such as massive bleeding or bowel fistulas.
Our case describes the management of a complicated intra-abdominal hemophilic pseudotumor requiring an emergency resection. The patient was discharged after 73 d and 2 further exploratory laparotomies due to complications. The authors recommend resection before complication, under appropriate factor VIII replacement therapy.
In this report, the authors described a patient with a hemophilic intraabdominal pseudotumor.
P- Reviewer: Gu DS S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | García-Pérez R, Torres-Salmerón G, Sánchez-Bueno F, García-López A, Parrilla-Paricio P. Intraabdominal hemophilic pseudotumor: case report. Rev Esp Enferm Dig. 2010;102:275-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Castro-Boix S, Pradell-Teigell J, Boqué-Genovard R, Zanón-Navarro V, Nadal-Guinard A, Altisent-Roca C, Armengol-Carrasco M. [Hemophilic pelvic pseudotumor]. Cir Esp. 2007;81:102-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kilic YA, Dundar SV, Onat D, Akhan O. Iliopsoas hemophilic pseudotumor with bowel fistulization. Bratisl Lek Listy. 2009;110:729-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Pakala A, Thomas J, Comp P. Hemophilic pseudotumor: a case report and review of literature. Int J Clin Med. 2012;3:229-233. |
| 5. | Ying SH, Chen WM, Wu PK, Chen CF, Liu CL, Chen TH. Pelvic hemophilic pseudotumor presenting as severe sciatic pain in a patient with no history of hemophilic symptoms. J Orthop Sci. 2012;17:490-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |