Published online Dec 27, 2015. doi: 10.4240/wjgs.v7.i12.403
Peer-review started: July 12, 2015
First decision: August 14, 2015
Revised: August 21, 2015
Accepted: September 25, 2015
Article in press: September 28, 2015
Published online: December 27, 2015
Processing time: 179 Days and 12.3 Hours
Gall bladder torsion (GBT) is a relatively uncommon entity and rarely diagnosed preoperatively. A constant factor in all occurrences of GBT is a freely mobile gall bladder due to congenital or acquired anomalies. GBT is commonly observed in elderly white females. We report a 77-year-old, Caucasian lady who was originally diagnosed as gall bladder perforation but was eventually found with a two staged torsion of the gall bladder with twisting of the Riedel’s lobe (part of tongue like projection of liver segment 4A). This together, has not been reported in literature, to the best of our knowledge. We performed laparoscopic cholecystectomy and she had an uneventful post-operative period. GBT may create a diagnostic dilemma in the context of acute cholecystitis. Timely diagnosis and intervention is necessary, with extra care while operating as the anatomy is generally distorted. The fundus first approach can be useful due to altered anatomy in the region of Calot’s triangle. Laparoscopic cholecystectomy has the benefit of early recovery.
Core tip: Gall bladder torsion is a rare surgical entity that should be considered in a case of suspicious acute cholecystitis not responding to conservative management. Delay in diagnosis and treatment may lead to gall bladder gangrene, gall bladder perforation, biliary peritonitis or septicaemia. The condition is seldom recognized preoperatively due to its clinical resemblance to acute cholecystitis. We report a 77-year-old, Caucasian lady who was originally diagnosed as gall bladder perforation but was eventually found to have a two staged torsion of the gall bladder with twisting of the Riedel’s lobe. This dual entity has so far not been reported in literature.
- Citation: Sunder YK, Akhilesh SP, Raman G, Deborshi S, Shantilal MH. Laparoscopic management of a two staged gall bladder torsion. World J Gastrointest Surg 2015; 7(12): 403-407
- URL: https://www.wjgnet.com/1948-9366/full/v7/i12/403.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i12.403
Gall bladder torsion (GBT) is a process, in which there is a mechanical organo-axial torsion that occurs along the gall bladder’s longitudinal axis involving cystic pedicle, with a pre-requisite of freely mobile gall bladder. Wendel[1] first described gall bladder torsion in 1898. Thereafter over 300 cases have been reported in literature and only few were operated laparoscopically. However till date, there has been no report in literature regarding a “two-staged torsion” along with a “tornado” like twisting of the Riedel’s lobe.
GBT commonly occurs in the geriatric population, with 85% of patients above 60 years of age. It is found more frequently in the white race with female to male ratio of 3:1[2]. As this entity is rare and its symptoms overlap with those of acute cholecystitis, it is difficult to diagnose preoperatively[3,4]. Timely intervention may prevent the morbidity and mortality associated with GBT. We present here a rare case of a two staged gall bladder torsion masquerading as a perforated gall bladder.
A 77-year-old, thin, Caucasian lady presented with acute pain in the right upper abdomen, radiating to the back for 4 d. There was no history of fever, jaundice or similar complaints in the past. On general examination, she was afebrile with a pulse rate of 96/min. She also had scoliosis. Her abdomen was soft, tenderness and guarding was present in right hypochondrium and Murphy’s sign was positive.
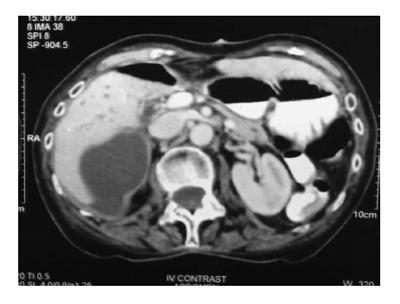
There were no signs of peritonitis. Laboratory investigations showed WBC 14000/cu mm and normal liver function tests. The CT scan showed a peripherally enhancing fluid collection along the segment 5 and 6 of the liver (Figures 1 and 2), and no gall bladder was seen in the gall bladder fossa. A diagnosis of gall bladder perforation with a subhepatic collection was made.
The patient was advised laparoscopic cholecystectomy but she refused surgery. She was managed conservatively with bowel rest, intravenous fluids, injectable antibiotics and analgesics. The patient did not improve and had increased WBC counts. After 4 d, she gave consent for surgery.
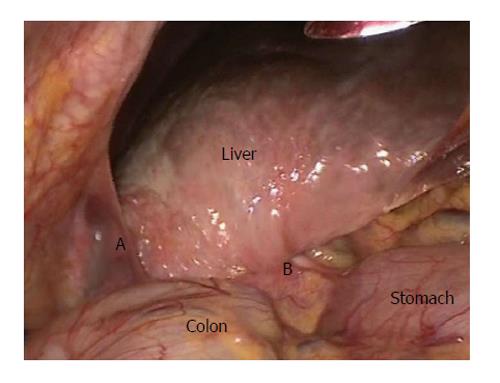
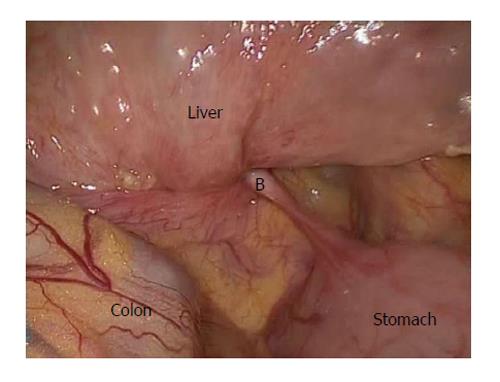
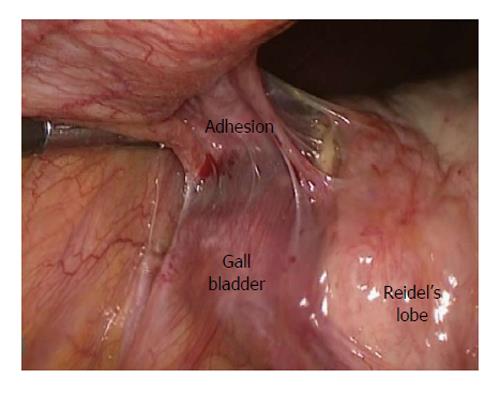
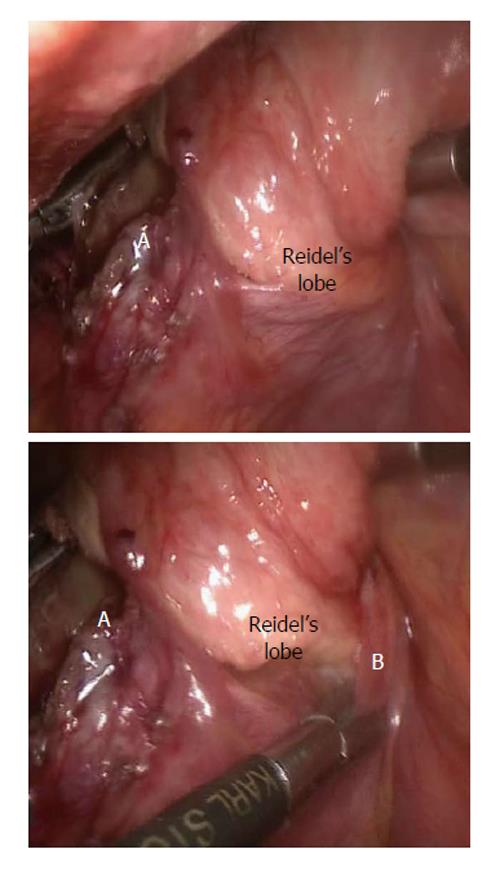
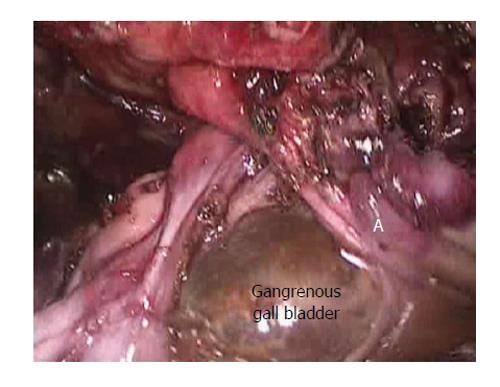
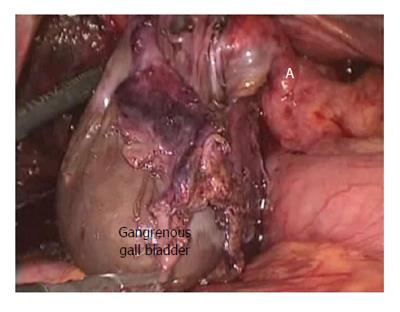
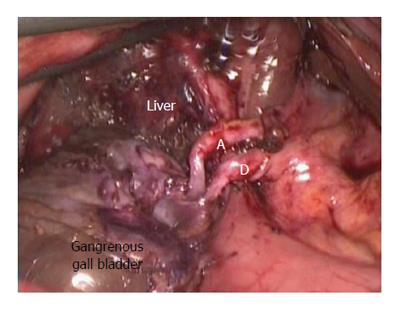
Intraoperatively, we found thick peritoneal folds arising from the pylorus and the hepatic flexure that were pulled into the region of Calot’s triangle along with the Riedel’s lobe. The gall bladder was adherent to the lateral abdominal wall (Figures 3-5). However, it was still unclear whether these pulled in structures contained the hilar structures or the cystic pedicle. As the anatomy was grossly distorted, we used the fundus first approach to avoid any injury to the hilar structures (Figure 6). After adhesiolysis, the gall bladder was found to be gangrenous till its neck. The gall bladder itself was rotated through 360° in the anticlockwise direction around the fixed cystic pedicle and its neck. There also was a band like adhesion between the neck and the Riedel’s lobe (Figure 7). After releasing this band, we noticed a remnant 90° anticlockwise rotation. This was also derotated (Figure 8). The cystic duct was found to be unusually long and twisted (Figures 8 and 9). The common bile duct (CBD) was kinked, pulled anteriorly and was lying close to the anterior edge of the liver. The cholecystectomy was thereafter safely completed.
In our case, the gall bladder may have undergone a two staged torsion. The first stage is a 90° anticlockwise rotation during the initial period of symptoms. This might have been followed by the adhesive band formation between the neck and the anomalous Riedel’s lobe. Subsequently, the gall bladder might have undergone the second stage of a 360° anticlockwise rotation, this time taking the Riedel’s lobe and the peritoneal folds (arising from the pylorus and the hepatic flexure). The delay in surgery may have led to the adhesions between the gall bladder and its surrounding structures after undergoing torsion.
An intra-operative cholangiogram was done and it was normal. The gall bladder was removed in an endo-bag through umbilical port. It did not contain any calculi. The histopathology report showed features of gangrenous gall bladder. Postoperatively, the patient improved and was discharged after three days.
GBT has been reported in patients ranging from 2 to 100 years old patients[5,6], more frequently in elderly white females. Loss of fat and elasticity may be responsible for its occurrence in the elderly population[7].
Gross classified the congenital floating gall bladder into two types. In type 1, the gall bladder and cystic duct are attached to the inferior surface of the liver via mesentery and in type 2, only the cystic duct is attached to the liver[8].
The pre-requisite for torsion is a “floating” gall bladder, where the entire organ is covered with peritoneum and is connected to the porta by a cystic pedicle enveloped in peritoneum. Torsion can also occur when the neck, or, along with the neck, part of gall bladder body is attached to the liver with a long pedicle. Several precipitating factors have been proposed as intense peristalsis of the neighbouring organs, blunt trauma to the abdomen, tortuous atherosclerotic cystic artery and kypho-scoliosis. Gall bladder stones are found only in 20%-33% of patients. Clockwise rotation of the gall bladder can occur due to intense stomach peristalsis or anti-clockwise due to transverse colon peristalsis[7]. But, there are no strong evidences to support these factors. Peristalsis is a continuous phenomenon, with up to 5% of the population have floating gall bladder[2,9]. In our case, there was a two staged torsion along with twisting of the Riedel’s lobe. To cause this type of torsion, an abnormally large force may be required and source of this force needs to be evaluated, as the above said precipitating factors do not seem to be the culprit.
Surgeons should have a high index of suspicion for GBT in acute cholecystitis patients, who fail to improve with conservative management. These patients should be considered for further careful imaging studies and prompt surgical intervention is required.
However, our patient presented with features of acute cholecystitis and on further imaging (CT scan), it was diagnosed as gall bladder perforation. Eventually, on laparoscopy, we found GBT with partially twisted Riedel’s lobe with the gall bladder being loosely adhered to the surrounding structures due to delay in surgical intervention.
GBT is difficult to diagnose pre-operatively because it is rare and the presentation is similar to that of acute cholecystitis[10,11]. Very few cases have been diagnosed precisely on pre-operative imaging[12]. The classical findings of GBT on ultrasound are a large “floating gall bladder”. On CT scan, presence of the gall bladder outside its normal position, an echogenic conical structure (twisted mesentery) and a prominent cystic artery to the right of gall bladder, GBT should be borne in mind[4,13,14]. MRI abdomen may accurately visualize the twisted cystic duct than any other imaging modality[15]. In very few cases, CT abdomen showed hugely enlarged gall bladder with its unusual shape and configuration[14]. GBT has been treated mostly by open surgical approach in past with few case reports using the laparoscopic approach. Laparoscopy adds the advantage of clearing the diagnostic dilemma and faster recovery.
As the anatomy is not very clear in GBT, one should be careful while dissecting in the region of the Calot’s triangle, as chances of CBD injury are high due to distorted anatomy. The fundus first approach can be useful due to distorted anatomy in the region of Calot’s triangle. The overall mortality in gall bladder torsion is approximately 5%[16].
Gall bladder torsion is an uncommon surgical entity that should be considered in a case of suspicious acute cholecystitis not improving on conservative management. Delay in diagnosis may lead to gall bladder gangrene, gall bladder perforation, biliary peritonitis, or septicaemia. Such complications may obscure the preoperative diagnosis of GBT. A rare possibility of an accompanying twisted Riedel’s lobe alters the anatomy and makes dissection cumbersome. Laparoscopic cholecystectomy is more feasible and safer than open approach.
A 77-year-old Caucasian lady with right upper quadrant pain since 4 d.
Her abdomen was soft with tenderness and guarding in the right hypochondrium and Murphy’s sign was positive.
Acute cholecystitis, gall bladder perforation.
WBC count 14000/cu, the other laboratory reports were within normal limits.
The computed tomography scan showed a peripherally enhancing fluid collection along segments 5 and 6 of the liver and no gall bladder was seen in the gall bladder fossa.
Final Histopathological report was suggestive of gangrenous gall bladder.
Laproscopic cholecystectomy.
Gall bladder torsion (GBT) is a rare entity, mostly seen in the geriatric population, masquerading as acute cholecystitis. In this case, it presented as gall bladder perforation. A two staged torsion was seen probably due to delayed surgical treatment.
In GBT, there is a mechanical organo-axial torsion that occurs along its longitudinal axis involving the cystic pedicle, with a prerequisite of a freely mobile gall bladder.
This entity is seldom diagnosed preoperatively. It mimics acute cholecystitis. The dissection in the region of Calot’s triangle must be done carefully due to the distorted anatomy.
This is uncommon case for laparoscopic cholecystectomy.
P- Reviewer: Al-Gayyar MMH, Lee KG S- Editor: Qiu S L- Editor: A E- Editor: Liu XM
| 1. | Wendel AV. VI. A Case of Floating Gall-Bladder and Kidney complicated by Cholelithiasis, with Perforation of the Gall-Bladder. Ann Surg. 1898;27:199-202. [PubMed] |
| 2. | Stieber AC, Bauer JJ. Volvulus of the gallbladder. Am J Gastroenterol. 1983;78:96-98. [PubMed] |
| 3. | Narchi H, Thomas M. Acute abdominal pain in a 6-year-old child. Eur J Pediatr. 1999;158:943-945. [PubMed] |
| 4. | Kitagawa H, Nakada K, Enami T, Yamaguchi T, Kawaguchi F, Nakada M, Yamate N. Two cases of torsion of the gallbladder diagnosed preoperatively. J Pediatr Surg. 1997;32:1567-1569. [PubMed] |
| 5. | Schroder DM, Cusumano DA. Laparoscopic cholecystectomy for gallbladder torsion. Surg Laparosc Endosc. 1995;5:330-334. [PubMed] |
| 6. | Taha AM, Welling RE. Acute torsion of the gallbladder in a 100-year-old female patient. J Natl Med Assoc. 1985;77:404-410. [PubMed] |
| 7. | Saber A. Gall bladder Volvulus [Internet]. Emedicine.medscape.com. Available from: http://emedicine.medscape.com/article/195100-overview#a0102. |
| 8. | Gross RE. Congenital anomalies of the gall bladder. A review of 148 cases with report of double gall bladder. Arch Surg. 1936;32:131-162. |
| 9. | Christoudias GC. Gallbladder volvulus with gangrene. Case report and review of the literature. JSLS. 1997;1:167-170. [PubMed] |
| 10. | Carter R, Thompson RJ, Brennan LP, Hinshaw DB. Volvulus of the gallbladder. Surg Gynecol Obstet. 1963;116:105-108. [PubMed] |
| 12. | Shaikh AA, Charles A, Domingo S, Schaub G. Gallbladder volvulus: report of two original cases and review of the literature. Am Surg. 2005;71:87-89. [PubMed] |
| 13. | Yeh HC, Weiss MF, Gerson CD. Torsion of the gallbladder: the ultrasonographic features. J Clin Ultrasound. 1989;17:123-125. [PubMed] |
| 14. | Merine D, Meziane M, Fishman EK. CT diagnosis of gallbladder torsion. J Comput Assist Tomogr. 1987;11:712-713. [PubMed] |
| 15. | Kimura T, Yonekura T, Yamauchi K, Kosumi T, Sasaki T, Kamiyama M. Laparoscopic treatment of gallbladder volvulus: a pediatric case report and literature review. J Laparoendosc Adv Surg Tech A. 2008;18:330-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Mouawad NJ, Crofts B, Streu R, Desrochers R, Kimball BC. Acute gallbladder torsion - a continued pre-operative diagnostic dilemma. World J Emerg Surg. 2011;6:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |