Published online Nov 27, 2015. doi: 10.4240/wjgs.v7.i11.345
Peer-review started: June 14, 2015
First decision: August 4, 2015
Revised: September 16, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: November 27, 2015
Processing time: 168 Days and 10.5 Hours
Twist of stomach remnant post sleeve gastrectomy is a rare entity and difficult to diagnose pre-operatively. We are reporting a case of gastric volvulus post laparoscopic sleeve gastrectomy, which was managed conservatively. A 38-year-old lady with a body mass index of 54 underwent laparoscopic sleeve gastrectomy. Sleeve gastrectomy was performed over a 32 French bougie using Endo-GIA tri-stapler. On post-operative day 1, patient had nausea and non-bilious vomiting. An upper gastrointestinal gastrografin study on post-operative days 1 and 2 revealed collection of contrast in the fundic area of stomach with poor flow distally, and she vomited gastrograffin immediately post procedure. With the suspicion of a stricture in the mid stomach as the cause, the patient was taken back for a exploratory laparoscopy and intra-operative endoscopy. We found a twist in the gastric tube which was too tight for the endoscope to pass through. This was managed conservatively with a long stent to keep the gastric tube straight and patent. The stent was discontinued in 7 d and the patient did well. In laparoscopic sleeve gastrectomy the stomach is converted into a tube and is devoid of its supports. If the staples fired are not aligned appropriately, it can predispose this stomach tube to undergo torsion along its long axis. Such a twist can be avoided by properly aligning the staples and by placing tacking sutures to the omentum and new stomach tube. This twist is a functional obstruction rather than a stricture; thus, it can be managed by endoscopy and stent placement.
Core tip: Twist of the stomach remnant post sleeve gastrectomy is a rare entity. We are reporting a case of gastric twist post laparoscopic sleeve gastrectomy. This was managed conservatively with a long stent for 7 d. In laparoscopic sleeve gastrectomy the stomach is converted into a tube and is devoid of its supports, making it prone for twisting. Such a twist can be avoided by properly aligning the staples and by placing tacking sutures to the omentum. This twist is a functional obstruction rather than a stricture; thus, it can be managed by endoscopy and stent placement.
- Citation: Subhas G, Gupta A, Sabir M, Mittal VK. Gastric remnant twist in the immediate post-operative period following laparoscopic sleeve gastrectomy. World J Gastrointest Surg 2015; 7(11): 345-348
- URL: https://www.wjgnet.com/1948-9366/full/v7/i11/345.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i11.345
Laparoscopic sleeve gastrectomy is a restrictive bariatric surgical strategy. Compared to other bariatric surgeries, this procedure has relatively lower surgical risk in patients with extreme obesity. However sleeve gastrectomy does have complications which includes leaks, bleeding, splenic trauma, sleeve stenosis, and gastroesophageal reflux[1].
Gastric volvulus is a rare condition which involves the rotation of all or part of the stomach around the anatomic axes[1]. We would like to report a case of twist of the gastric remnant in the immediate post laparoscopic sleeve gastrectomy period, done for morbid obesity. This was managed non operatively with stent placement.
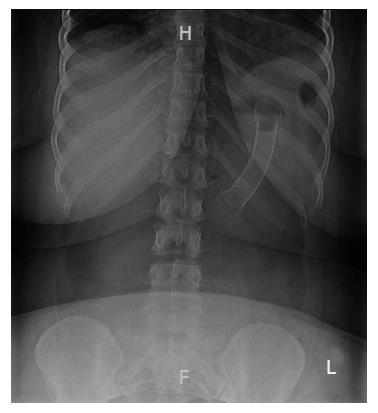
A 38-year-old morbidly obese lady with a body mass index of 54 underwent laparoscopic sleeve gastrectomy. Sleeve gastrectomy which was performed over a thirty two french bougie using Endo-GIA stapler with the tri staple purple load (Covidien Tri-Staple™, Mansfield, MA). Intraoperatively, post application of stapler, there was a bleeding from the stapled line at the mid stomach which was managed by a single imbricating stitch. On post-operative day 1, patient had persisting nausea and non bilious vomiting. An upper gastrointestinal (GI) gastrografin study revealed collection of contrast in the fundic area of stomach with poor flow distally; she vomited gastrografin immediately post procedure (Figure 1). She was kept nil per os (NPO) and the upper GI gastrografin study was repeated on post-operative day 2. Similar findings of collection of contrast in the fundic region of stomach with very little filling distally were noted. This raised a suspicion of stricture in the mid stomach. With a suspicion of the imbricating stitch in the mid stomach as the cause, the patient was taken back for a exploratory laparoscopy and intra operative endoscopy.
During exploratory laparoscopy, the stitch did not seem to be causing any constriction. The stitch was cut and no bleeding was noted. An intraoperative endoscopy showed complete obstruction in the mid stomach with inability pass the scope beyond the obstruction. Manipulation of stomach laparoscopically with simultaneous scope manipulation was needed to negotiate the narrowed mid stomach. A diagnosis of twist of the stomach along the long axis of the tubular remnant was made. She was kept NPO and started on total parenteral nutrition.
A long esophageal 18 mm × 15 cm long, fully silicone covered stent (WallFlex™, Boston Scientific, Natick, MA) was placed endoscopically on post-operative day 6 (Figure 2). She was able to tolerate liquid diet and was discharged home. The stent was removed endoscopically a week after its placement. She was put on a liquid diet for 2 wk and advanced to soft diet subsequently, which she tolerated well. Patient was seen to be doing well on a 6-mo follow-up visit.
Sleeve gastrectomy is a safe, reproducible technique with a relatively low rate of complications. Benefits of sleeve gastrectomy include the lower complications, the maintenance of normal gastro-intestinal continuity, the absence of mal-absorption and the ability to convert to multiple other operations. Excising the ghrelin producing stomach mass plays a significant role compared to other gastric restrictive procedures[2]. Laparoscopic sleeve gastrectomy is still associated with complications, these include, but are not limited to: Staple line leak (1.17%), post-operative hemorrhage (3.57%), and the irreversibility of gastrectomy[3].
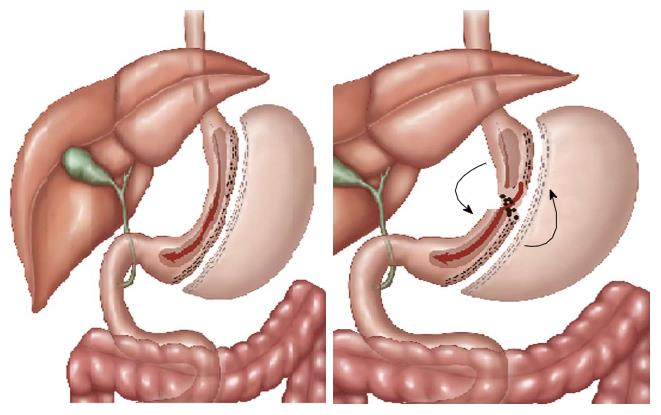
Gastric volvulus is a rare condition which involves the rotation of the stomach around the anatomic axes. There are two forms of gastric volvulus, organo-axial (axis is longitudinal and passes through the pylorus and gastroesophageal junction) and mesenteric-axial (axis is transverse and passes through the middle of stomach). Gastrosplenic, gastrophrenic, gastrocolic, and gastrohepatic ligaments hold the stomach in anatomotical position. Stomach can be prone for volvulus whenever there is laxity in the gastric fixation or incorrect positioning of the stomach post surgical manipulation[1]. Twist of the gastric remnant is a condition similar to the organo-axial gastric volvulus.
Sleeve stenosis, which is currently seen in 0.2% to 4% of laparoscopic sleeve gastrectomies, can occur due to the intentionally creating a narrow tube of the stomach[4]. A twisted or spiral sleeve caused by the progressive rotation of the staple line in an anterior to posterior plane can lead to a functional narrowing despite a fairly normal luminal diameter, and is another cause of symptomatic stenosis. This functional stenosis makes it difficult for gastric contents to pass through, in spite of easy passage of the endoscope or balloon dilator through the narrowed area. This can be equated to twisting a straight balloon wherein there is a twist at the incisura (Figure 3). An endoscope can be made to pass through by twisting in the same direction, which will undo the twist. Unless supported by a stent, the twist recurs on withdrawal of the endoscope. Scarring caused by hematomas can also lead to sleeve stenosis. Mechanical short-segment stenosis may be treated successfully with single or multiple endoscopic balloon dilation. But mechanical long-segment stenosis may ultimately require conversion to Roux-en-Y gastric bypass[4].
The dissection performed during sleeve gastrectomy including separation of greater omentum from the greater curvature of the stomach, makes the remnant stomach prone for volvulus as there are no fixations along the entire greater curvature[1]. Cases of organoaxial gastric volvulus have been reported after laparoscopic gastric banding, due to excessive dissection of the posterior wall of the stomach, which makes it mobile[5,6]. It is recommended to do a proper posterior dissection of the stomach in sleeve gastrectomy in order to achieve a symmetric stapling of the posterior and anterior wall to avoid twisting of the remnant stomach tube[7]. Pexy of omentum to the gastric remnant may also help to avoid such a twist in the remnant stomach after sleeve gastrectomy.
Flexible covered stents use has been described for patients with suture line leaks and strictures following sleeve gastrectomy[4,8]. Following stent placement, patients may experience nausea, hypersialysis, early satiety and mild retro-sternal discomfort, which usually disappear in the first few days. Stent removal is not always easy, due to scarring around the stent, and mucosal injury and bleeding are frequently seen after removal. Another complication is stent migration, which can be seen in up to one third of cases[8].
Our patient developed obstruction due to torsion along the long axis of the remnant stomach on post operative day 1. There is a possibility of asymmetrical staples leading to initiation of the twist but completion of twist to an extent of obstruction as in a volvulus is attributed to a long tubular remnant with no supports. We feel that in this patient, creation of a longer stomach tube post removal of ligaments namely gastrosplenic and gastrophrenic made the tubular stomach devoid of its support, which then became susceptible to torsion. Some degree of a twist is seen in every stomach post laparoscopic sleeve gastrectomy but none of these cause functional stricture. These twists can be managed non-operatively with placement of covered stent. Also, mobilized omentum can tacked to the gastric tube on the stapled side and this could help in prevention of rotation by virtue of its weight.
The tubular gastric remnant is devoid of its supports and is predisposed to volvulus. In this present case we feel that a twist could have been initiated by asymmetrical staples which then progressed to a complete torsion in the organo-axial axis with functional stricture due to a long tubular remnant without anatomical support. We currently tack the mobilized omentum to the stapled side of gastric tube to help prevent post-operative twist. This condition can be managed non-operatively with placement of covered stent. There is always an option of converting it to a Roux-en-Y gastric bypass if the non-operative management fails.
A 38-year-old morbidly obese lady with a body mass index of 54 underwent laparoscopic sleeve gastrectomy and presented with post-operative gastric remnant twist.
Post-operative gastric remnant twist.
Stricture, post-operative edema, hematoma.
All labs were within normal limits.
Upper gastrointestinal gastrograffin study showed collection of contrast in the fundic area of stomach with poor flow distally.
Placement of a long stent endoscopically.
Most of the reports are of gastric volvulus which was managed by operative intervention.
During laparoscopic gastric sleeve resection the authors currently tack the mobilized omentum to the stapled side of gastric tube to help prevent post-operative twist and post-operative gastric twist can be managed non-operatively with placement of covered stent.
This is a nice and well documented case report.
P- Reviewer: De Palma GD S- Editor: Ji FF
L- Editor: A E- Editor: Li D
| 1. | Del Castillo Déjardin D, Sabench Pereferrer F, Hernàndez Gonzàlez M, Blanco Blasco S, Cabrera Vilanova A. Gastric volvulus after sleeve gastrectomy for morbid obesity. Surgery. 2013;153:431-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Gumbs AA, Gagner M, Dakin G, Pomp A. Sleeve gastrectomy for morbid obesity. Obes Surg. 2007;17:962-969. [PubMed] |
| 3. | Shi X, Karmali S, Sharma AM, Birch DW. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20:1171-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 219] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 4. | Parikh A, Alley JB, Peterson RM, Harnisch MC, Pfluke JM, Tapper DM, Fenton SJ. Management options for symptomatic stenosis after laparoscopic vertical sleeve gastrectomy in the morbidly obese. Surg Endosc. 2012;26:738-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Bortul M, Scaramucci M, Tonello C, Spivach A, Liguori G. Gastric wall necrosis from organo-axial volvulus as a late complication of laparoscopic gastric banding. Obes Surg. 2004;14:285-287. [PubMed] |
| 6. | Kicska G, Levine MS, Raper SE, Williams NN. Gastric volvulus after laparoscopic adjustable gastric banding for morbid obesity. AJR Am J Roentgenol. 2007;189:1469-1472. [PubMed] |
| 7. | Lacy A, Ibarzabal A, Pando E, Adelsdorfer C, Delitala A, Corcelles R, Delgado S, Vidal J. Revisional surgery after sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |