Published online Nov 27, 2015. doi: 10.4240/wjgs.v7.i11.313
Peer-review started: June 26, 2015
First decision: July 25, 2015
Revised: September 8, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: November 27, 2015
Processing time: 156 Days and 23.9 Hours
While diverticular disease is extremely common, the natural history (NH) of its most frequent presentation (i.e., sigmoid diverticulitis) is poorly investigated. Relevant information is mostly restricted to population-based or retrospective studies. This comprehensive review aimed to evaluate the NH of simple sigmoid diverticulitis. While there is a clear lack of uniformity in terminology, which results in difficulties interpreting and comparing findings between studies, this review demonstrates the benign nature of simple sigmoid diverticulitis. The overall recurrence rate is relatively low, ranging from 13% to 47%, depending on the definition used by the authors. Among different risk factors for recurrence, patients with C-reactive protein > 240 mg/L are three times more likely to recur. Other risk factors include: Young age, a history of several episodes of acute diverticulitis, medical vs surgical management, male patients, radiological signs of complicated first episode, higher comorbidity index, family history of diverticulitis, and length of involved colon > 5 cm. The risk of developing a complicated second episode (and its corollary to require an emergency operation) is less than 2%-5%. In fact, the old rationale for elective surgery as a preventive treatment, based mainly on concerns that recurrence would result in a progressively increased risk of sepsis or the need for a colostomy, is not upheld by the current evidence.
Core tip: The natural history of sigmoid diverticulitis is poorly understood. While there is a clear lack of uniformity in terminology, which results in difficulties interpreting and comparing findings between studies, this comprehensive review demonstrates the benign nature of simple sigmoid diverticulitis. The overall recurrence rate is relatively low. Several risk factors are found to be associated with recurrence.
- Citation: Buchs NC, Mortensen NJ, Ris F, Morel P, Gervaz P. Natural history of uncomplicated sigmoid diverticulitis. World J Gastrointest Surg 2015; 7(11): 313-318
- URL: https://www.wjgnet.com/1948-9366/full/v7/i11/313.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i11.313
Colonic diverticulosis is an increasingly common condition in the Western world. Half of the population is affected by the 6th decade and two-thirds by the 9th decade[1,2]. Fortunately, the majority of patients with diverticulosis remains asymptomatic; diverticulitis, the most common presentation of diverticular disease, has a life time prevalence of 25%[3,4]. The diagnosis of sigmoid diverticulitis is usually suspected clinically in a patient presenting with acute lower abdominal pain, associated with an inflammatory syndrome. The preferred imaging modality is computed tomography (CT)[5] scan, which may also demonstrate complicated diverticulitis (abscess, fistula or peritonitis)[6]. A full colonoscopy once the acute inflammatory process has resolved[5] is recommended in order to exclude cancer or inflammatory bowel disease[7]. Most patients presenting with simple diverticulitis will be successfully managed symptomatically or with antibiotics alone[8-11].
Whilst diverticular disease is extremely common, there are few prospective series documenting the natural history (NH) of sigmoid diverticulitis[12,13]. Studies from the 1960s had suggested that a recurrent episode of diverticulitis occurs in > 40% of patients, and that these are complicated in up to 60%[14]. However, recent series suggest that the NH of sigmoid diverticulitis, in the era of modern antibiotics, is more benign[15,16], as shown in our prospective cohort study[17]. A few have looked at the incidence and severity of recurrent diverticulitis but with the diagnosis based upon clinical parameters only[18]. Without a CT scan it is difficult to differentiate between simple and Hinchey I-II diverticulitis[10,19,20]. So, the existing studies probably do not provide reliable information regarding the NH of simple diverticulitis.
The object of this review is to evaluate the NH of simple sigmoid diverticulitis.
There is a clear lack of uniformity in terminology resulting in difficulties interpreting and comparing findings between studies[10,18].
NH can be defined as the longitudinal outcomes for patients whose disease was managed non-operatively[21]. In our own cohort (NCT01015378), we chose a definition of simple diverticulitis, which comprised 4 criteria[22]: (1) Clinical: Acute lower abdominal pain or discomfort; (2) Biological: Inflammatory syndrome [C-reactive protein (CRP) > 50 mg/L or white blood cell count > 11000 G/mm3]; (3) Radiological: Signs of inflammation of the sigmoid and/or descending colon on a CT scan ideally performed with triple contrast injection (oral, rectal, and intra-venous); and (4) Endoscopic: To document the presence of diverticula (i.e., confirming the diagnosis) and rule out another associated condition.
All patients are usually encouraged to undergo routine colonoscopy six to twelve weeks after the first attack, in order to rule out malignancy, although the evidence supporting this practice is weak[10,18].
Regarding outcomes, a diagnosis of recurrent diverticulitis implied that the patient has completely recovered from their first episode. An interval of 12 wk without symptoms in between two attacks was required. All the aforementioned criteria were required to confirm a recurrent diverticulitis (including an abdominal CT). The Hinchey classification[23], or its modified versions[24], was used to stage complicated diverticulitis. In addition, we considered a fistula and a stenosis as a complicated attack[18].
Recent advances in the understanding of diverticular pathophysiology and NH have led to substantial changes in diverticulitis treatment guidelines[21].
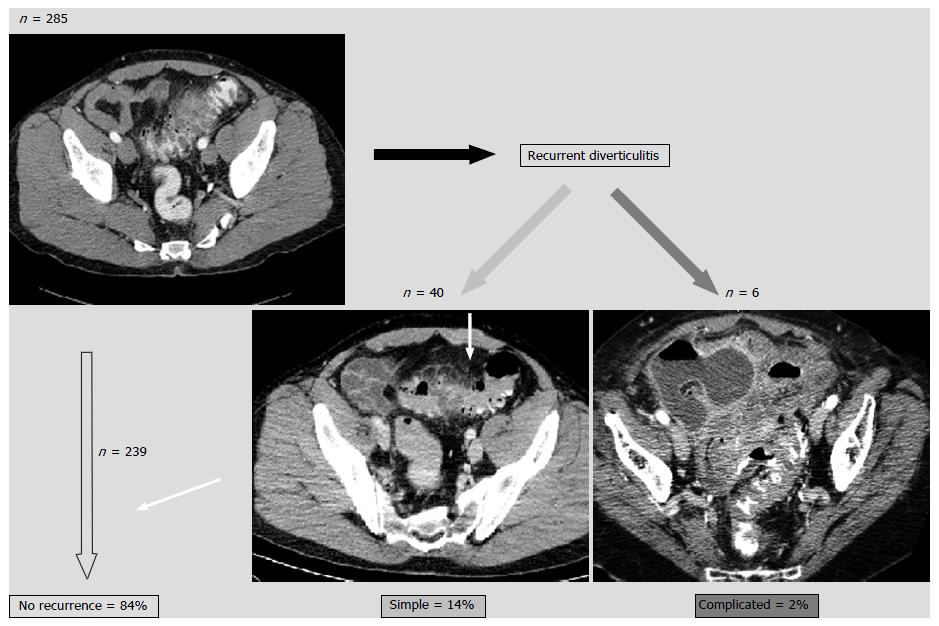
We have recently published a large prospective single center cohort study focusing on the NH of sigmoid diverticulitis[17]. We demonstrated that, after a first episode of simple diverticulitis, the overall recurrence rate was 16%, and that 87% of recurrences were of similar severity (Figure 1). Of note, four patients only (1.4%) underwent emergency surgery for complicated (Hinchey stages III/IV) diverticulitis. The main predictor of recurrence after a first attack was a serum CRP > 240 mg/L. Subsequently, 23 (8.2%) patients proceeded to an elective laparoscopic sigmoid colectomy because of chronic symptoms. In addition, as reported by others, the highest risk of recurrence was within the first year (10%) and dropped to approximately 3% in the years thereafter[25,26].
In series without adequate imaging with CT scan as a prerequisite for inclusion, recurrence rates ranged from 13% to 47% (Table 1), depending on the definition used by the authors. Two United States series using large administrative databases have reported recurrence rates between 13% and 19%, which is in accordance with the results from our institution[17] and from other centers[27,28]. Indeed, in a study population of 3165 patients with acute diverticulitis, Broderick-Villa et al[28] reported a recurrence rate of 13.3% after a follow-up of 8.9 years. Less than 4% presented with a second recurrence, as others have shown[26].
| Ref. | No. of patients | Type of study | FU | Recurrence rate | Comments |
| Lahat et al[38], 2013 | 261 | Prospective | 88 mo | 21.5% | 21% operated, 46.6% asymptomatic |
| Buchs et al[17], 2013 | 280 | Prospective | 24 mo | 16.4% | RF: CRP > 240 |
| Humes and West[35], 2012 | 2950 | Population-based cohort study | 7.99 yr | - | Risk of fistula correlates to the number of prior episodes of diverticulitis |
| Binda et al[36], 2012 | 743 | Multicenter, retro-prospective | 10.7 yr | 17.2%1 | RF: < 40 yr, 3 episodes |
| Hall et al[16], 2011 | 672 | Retrospective | 42.8 mo | 36% | RF: Family history, length of involved colon > 5 cm, retroperitoneal abscess |
| Mäkelä et al[20], 2010 | 555 | Retrospective | - | 42% | 38% of recurrence diagnosed on clinical findings |
| Eglinton et al[26], 2010 | 320 | Retrospective | 101 mo | 18.8% | 4.7% more than one recurrent episode |
| Pittet et al[19], 2009 | 271 | Retrospective | - | 25% | Similar severity |
| Mueller et al[48], 2005 | 252 | Retrospective | 89 mo | 47% (with 10% readmitted) | Based on symptoms |
| Anaya and Flum[27], 2005 | 25058 | Cohort study, retrospective | - | 19% | RF: < 50 yr, number of recurrent episodes |
| Broderick-Villa et al[28], 2005 | 3165 (2366 managed conservatively) | Cohort study, retrospective | 8.9 yr | 13.3% | RF: < 50 yr, charlson comorbidity index ≥ 1 |
| Biondo et al[40], 2002 | 327 | Retrospective | 24-90 mo | 15.9% | Age not a RF |
| Chautems et al[15], 2002 | 118 | Prospective | 9.5 yr | 31% | Considering only patients undergoing an operation |
| Somasekar et al[34], 2002 | 108 | Two-center, retrospective | - | 2.7%1 | Only patients with complicated disease |
| Mäkelä et al[43], 1998 | 366 | Retrospective | - | 22% | RF: < 50 yr, male |
| Ambrosetti et al[44], 1997 | 300 | Prospective | 46 mo | 2% | RF: Radiological signs of complicated first episode |
| Parks[14], 1969 | 317 | Retrospective | - | 24.6% | Only readmitted patients |
The emerging picture is then that recurrence is relatively rare, and that recurrent diverticulitis is rarely severe[16,26]. The results of our study[17] confirm that a non-surgical strategy for the treatment of uncomplicated diverticulitis is safe in the long term[29]. They also contradict the once popular view that diverticulitis is a progressive disease[30]. Out of the 6 patients (2.1%) who developed complicated diverticulitis during follow-up, four (1.4%) patients developed peritonitis (Hinchey III/IV) and underwent emergency Hartmann operation. A conservative policy after a first episode of simple diverticulitis is thus associated with a colostomy rate, which is similar to the risk of anastomotic dehiscence after an elective sigmoid colectomy[31]. Eglinton et al[26] found a risk of 5% for developing complicated disease after a first episode of uncomplicated diverticulitis. The risk of stoma formation was only 0.9%, all of which were temporary and subsequently reversed. Most perforations do not occur after recurrences, but after the first attack of acute diverticulitis[19,30,32-34]. Humes and West[35] however showed that, although most patients in their study (72.3%) had suffered no prior episodes of acute diverticulitis, further episodes of acute diverticulitis were associated with an increased risk of developing a fistula (OR = 1.54, 95%CI: 1.08-2.19), but there was no clear relationship with perforation or abscess.
Among the different risk factors for recurrence, age has often been mentioned (Table 1)[15,36]. In the past, sigmoidectomy was advocated in young patients (< 50 years at the first episode)[37]. But, younger patients have a similar absolute risk of recurrence, and a higher lifetime risk[10]. Buchs et al[17] do not agree with the general thought that younger patients has more aggressive diverticulitis, as suggested by others[26,36,38-40]. We agree the recent shift towards a more conservative management of diverticulitis is effective for all the different age groups. There is no evidence that younger patients should be treated differently from older patients[5,18].
The gravity of inflammation (measured by the CRP level) is associated with a higher probability of recurrence, as shown in our series[17]. The risk of recurrence at 6 mo was 22% for patients with CRP > 240 mg/L during their initial episode. Recently, CRP was seen as an interesting marker in simple cases of sigmoid diverticulitis. A level higher than 200 mg/L can be associated with local complication[41,42]. We recently proposed that the diagnostic criteria for diverticulitis should include CRP[22]. In our series, free pelvic fluid seen on CT was not associated with further recurrence. However, the discovery of a pneumoperitoneum was of borderline significance. Others groups have reported risk factors for recurrence, including: Age younger than 40 (or 50), a history of a least 3 episodes of acute diverticulitis, medical vs surgical management, male patients, radiological signs of complicated first episode (abscess formation and extra-colonic contrast or gas), higher comorbidity index, family history of diverticulitis, and length of involved colon > 5 cm[16,27,28,36,43,44].
In addition, risk factors for the development of complicated diverticulitis include smoking, non-steroidal anti-inflammatory drugs use, renal failure, organ transplants and steroid use[10].
After the resolution of an episode of diverticulitis, a variety of medical therapies have been used to prevent future attacks. Supplemental fiber, antispasmodics, rifaximin, Mesalamine 5-aminosalicyclic acid (5-ASA), and probiotics have all been studied. These studies included heterogeneous patients however the history of diverticulitis was poorly characterized[5]. 5-ASA has been reported to reduce the risk of recurrent symptomatic diverticular disease[10], but there is no evidence that it may prevent recurrent diverticulitis. A recent randomized controlled trial showed that 5-ASA did not reduce the risk of recurrence or time to recurrence. The proportion of patients requiring surgery was comparable among 5-ASA and placebo groups[45]. Whilst a protective benefit for these agents has been suggested, their role in prevention of diverticulitis remains to be properly defined[5,46].
This review has some limitations. First, most of the studies consider only individuals who received in-hospital treatment, and it is known that 50% of diverticulitis patients are safely managed in an outpatient setting[18,47]. There is a risk of bias in considering for inclusion the most severe cases of diverticulitis. Second, longer follow-up is needed to draw definitive conclusions. Finally, the clear lack of uniformity in terminology results in difficulties interpreting and comparing findings between studies.
In conclusion, we have demonstrated the benign nature of simple sigmoid diverticulitis in the vast majority of cases, with a low rate of recurrence, and most importantly a very low rate of subsequent peritonitis requiring emergency surgery. The risk of complication after sigmoidectomy for simple diverticulitis is probably superior than the risk to develop a complication related to the disease itself. And surgery does not completely protect against recurrence[36]. The old rationale for elective surgery as a preventive treatment, based mainly on concerns that recurrence would result in progressively increased risk of sepsis or the need of colostomy[21], is thus not supported by current series.
P- Reviewer: Contini S, Nuno-Guzman CM, Steele SR
S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Lidor AO, Segal JB, Wu AW, Yu Q, Feinberg R, Schneider EB. Older patients with diverticulitis have low recurrence rates and rarely need surgery. Surgery. 2011;150:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 252] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 3. | Floch MH, Bina I. The natural history of diverticulitis: fact and theory. J Clin Gastroenterol. 2004;38:S2-S7. [PubMed] |
| 4. | Rafferty J, Shellito P, Hyman NH, Buie WD. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 463] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 5. | Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 386] [Article Influence: 35.1] [Reference Citation Analysis (1)] |
| 6. | Ambrosetti P. Acute diverticulitis of the left colon: value of the initial CT and timing of elective colectomy. J Gastrointest Surg. 2008;12:1318-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Wong WD, Wexner SD, Lowry A, Vernava A, Burnstein M, Denstman F, Fazio V, Kerner B, Moore R, Oliver G. Practice parameters for the treatment of sigmoid diverticulitis--supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290-297. [PubMed] |
| 8. | Ambrosetti P, Gervaz P, Fossung-Wiblishauser A. Sigmoid diverticulitis in 2011: many questions; few answers. Colorectal Dis. 2012;14:e439-e446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Poletti PA, Platon A, Rutschmann O, Kinkel K, Nyikus V, Ghiorghiu S, Morel P, Terrier F, Becker CD. Acute left colonic diverticulitis: can CT findings be used to predict recurrence? AJR Am J Roentgenol. 2004;182:1159-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Vennix S, Morton DG, Hahnloser D, Lange JF, Bemelman WA. Systematic review of evidence and consensus on diverticulitis: an analysis of national and international guidelines. Colorectal Dis. 2014;16:866-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012;99:532-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 335] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 12. | Gervaz P, Platon A, Widmer L, Ambrosetti P, Poletti PA. A clinical and radiological comparison of sigmoid diverticulitis episodes 1 and 2. Colorectal Dis. 2012;14:463-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Salem TA, Molloy RG, O’Dwyer PJ. Prospective, five-year follow-up study of patients with symptomatic uncomplicated diverticular disease. Dis Colon Rectum. 2007;50:1460-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Parks TG. Natural history of diverticular disease of the colon. A review of 521 cases. Br Med J. 1969;4:639-642. [PubMed] |
| 15. | Chautems RC, Ambrosetti P, Ludwig A, Mermillod B, Morel P, Soravia C. Long-term follow-up after first acute episode of sigmoid diverticulitis: is surgery mandatory?: a prospective study of 118 patients. Dis Colon Rectum. 2002;45:962-966. [PubMed] |
| 16. | Hall JF, Roberts PL, Ricciardi R, Read T, Scheirey C, Wald C, Marcello PW, Schoetz DJ. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011;54:283-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 158] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | Buchs NC, Konrad-Mugnier B, Jannot AS, Poletti PA, Ambrosetti P, Gervaz P. Assessment of recurrence and complications following uncomplicated diverticulitis. Br J Surg. 2013;100:976-979; discussion 979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Andeweg CS, Mulder IM, Felt-Bersma RJ, Verbon A, van der Wilt GJ, van Goor H, Lange JF, Stoker J, Boermeester MA, Bleichrodt RP. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30:278-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 141] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 19. | Pittet O, Kotzampassakis N, Schmidt S, Denys A, Demartines N, Calmes JM. Recurrent left colonic diverticulitis episodes: more severe than the initial diverticulitis? World J Surg. 2009;33:547-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Mäkelä JT, Kiviniemi HO, Laitinen ST. Spectrum of disease and outcome among patients with acute diverticulitis. Dig Surg. 2010;27:190-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Morris AM, Regenbogen SE, Hardiman KM, Hendren S. Sigmoid diverticulitis: a systematic review. JAMA. 2014;311:287-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 22. | Gervaz P, Ambrosetti P. Time for a (re) definition of (recurrent) sigmoid diverticulitis? Ann Surg. 2011;254:1076-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85-109. [PubMed] |
| 24. | Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, Essani R, Beart RW. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100:910-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 346] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 25. | Haglund U, Hellberg R, Johnsén C, Hultén L. Complicated diverticular disease of the sigmoid colon. An analysis of short and long term outcome in 392 patients. Ann Chir Gynaecol. 1979;68:41-46. [PubMed] |
| 26. | Eglinton T, Nguyen T, Raniga S, Dixon L, Dobbs B, Frizelle FA. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 27. | Anaya DA, Flum DR. Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch Surg. 2005;140:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 201] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 28. | Broderick-Villa G, Burchette RJ, Collins JC, Abbas MA, Haigh PI. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581; discussion 581-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 176] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 29. | Shaikh S, Krukowski ZH. Outcome of a conservative policy for managing acute sigmoid diverticulitis. Br J Surg. 2007;94:876-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 30. | Chapman JR, Dozois EJ, Wolff BG, Gullerud RE, Larson DR. Diverticulitis: a progressive disease? Do multiple recurrences predict less favorable outcomes? Ann Surg. 2006;243:876-830; discussion 880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 31. | Gervaz P, Inan I, Perneger T, Schiffer E, Morel P. A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg. 2010;252:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 32. | Andeweg C, Peters J, Bleichrodt R, van Goor H. Incidence and risk factors of recurrence after surgery for pathology-proven diverticular disease. World J Surg. 2008;32:1501-1506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Klarenbeek BR, Samuels M, van der Wal MA, van der Peet DL, Meijerink WJ, Cuesta MA. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251:670-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 34. | Somasekar K, Foster ME, Haray PN. The natural history diverticular disease: is there a role for elective colectomy? J R Coll Surg Edinb. 2002;47:481-482, 484. [PubMed] |
| 35. | Humes DJ, West J. Role of acute diverticulitis in the development of complicated colonic diverticular disease and 1-year mortality after diagnosis in the UK: population-based cohort study. Gut. 2012;61:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 36. | Binda GA, Arezzo A, Serventi A, Bonelli L, Facchini M, Prandi M, Carraro PS, Reitano MC, Clerico G, Garibotto L. Multicentre observational study of the natural history of left-sided acute diverticulitis. Br J Surg. 2012;99:276-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 38. | Lahat A, Avidan B, Sakhnini E, Katz L, Fidder HH, Meir SB. Acute diverticulitis: a decade of prospective follow-up. J Clin Gastroenterol. 2013;47:415-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Nelson RS, Ewing BM, Wengert TJ, Thorson AG. Clinical outcomes of complicated diverticulitis managed nonoperatively. Am J Surg. 2008;196:969-972; discussion 973-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 40. | Biondo S, Parés D, Martí Ragué J, Kreisler E, Fraccalvieri D, Jaurrieta E. Acute colonic diverticulitis in patients under 50 years of age. Br J Surg. 2002;89:1137-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Käser SA, Fankhauser G, Glauser PM, Toia D, Maurer CA. Diagnostic value of inflammation markers in predicting perforation in acute sigmoid diverticulitis. World J Surg. 2010;34:2717-2722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 42. | Tursi A, Elisei W, Brandimarte G, Giorgetti GM, Aiello F. Predictive value of serologic markers of degree of histologic damage in acute uncomplicated colonic diverticulitis. J Clin Gastroenterol. 2010;44:702-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 43. | Mäkelä J, Vuolio S, Kiviniemi H, Laitinen S. Natural history of diverticular disease: when to operate? Dis Colon Rectum. 1998;41:1523-1528. [PubMed] |
| 44. | Ambrosetti P, Grossholz M, Becker C, Terrier F, Morel P. Computed tomography in acute left colonic diverticulitis. Br J Surg. 1997;84:532-534. [PubMed] |
| 45. | Raskin JB, Kamm MA, Jamal MM, Márquez J, Melzer E, Schoen RE, Szalóki T, Barrett K, Streck P. Mesalamine did not prevent recurrent diverticulitis in phase 3 controlled trials. Gastroenterology. 2014;147:793-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 46. | Maconi G, Barbara G, Bosetti C, Cuomo R, Annibale B. Treatment of diverticular disease of the colon and prevention of acute diverticulitis: a systematic review. Dis Colon Rectum. 2011;54:1326-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 47. | Etzioni DA, Chiu VY, Cannom RR, Burchette RJ, Haigh PI, Abbas MA. Outpatient treatment of acute diverticulitis: rates and predictors of failure. Dis Colon Rectum. 2010;53:861-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 48. | Mueller MH, Glatzle J, Kasparek MS, Becker HD, Jehle EC, Zittel TT, Kreis ME. Long-term outcome of conservative treatment in patients with diverticulitis of the sigmoid colon. Eur J Gastroenterol Hepatol. 2005;17:649-654. [PubMed] |