Published online Jan 27, 2015. doi: 10.4240/wjgs.v7.i1.10
Peer-review started: October 24, 2014
First decision: November 27, 2014
Revised: December 22, 2014
Accepted: December 29, 2014
Article in press: January 4, 2015
Published online: January 27, 2015
Processing time: 88 Days and 15.1 Hours
AIM: To present the effectiveness of minimal invasive vascular zet ligation in the surgical treatment of haemorrhoidal disease (HD).
METHODS: Among 138 patients with 2nd-4th grade internal HD having several complaints and operated at our hospital between 2003-2013; 116 patients who regularly attended 1-year control were included in the study. Operation times, postoperative early period pain, satisfaction score, complications and relapse details were obtained from computer records retrospectively. Visual Analogous Scale (VAS) scores were used for patient satisfaction on the 3rd, 7th and 21st days. Technique; fixed suture which is constituted by the first leg of the Z-shaped suture (to pass by the mucosa and muscular layer) was put in the pile root in order to ensure vascular ligation and fixation. The second leg of the Z-shaped suture is constituted by mobile suture and it passes by the pile mucosa and submucosa which prolapses 5-10 mm below the first suture.
RESULTS: Seventy-five of the patients (65%) were male, 41 of them (35%) were female and their age average was 41. The mean operation time was 12 ± 4.8 min. VAS/satisfaction score was found as 2.2/4.3, 1.8/4.0, 1.2/4.4 respectively on the 3rd, 7th, and 21st days. Four of the patient (3.5%) had relapse.
CONCLUSION: This technique is an easily applicable, cost efficient way of operation which increases patient satisfaction.
Core tip: The non surgical and surgical therapy of symptomatic hemorrhoidal disease, cannot achieve the same results at each patient. The vascular Z suture technique, is an innovative technique employed in the surgical therapy of symptomatic haemorrhoid of 3-4 degree. This technique is reducing significantly the complications which are annoying both the postoperative patient and the surgeon. The product of ten years experience and development, this technique has a facile application and increases the postoperative life quality of the patient. The most distinctive and highest qualities of this technique are embed in the shortness of the operation time, easy applicability and reduction in the postoperative bleeding and pain symptoms of the patient as well as a shorter recovery period.
- Citation: Gemici K, Okuş A, Ay S. Vascular Z-shaped ligation technique in surgical treatment of haemorrhoid. World J Gastrointest Surg 2015; 7(1): 10-14
- URL: https://www.wjgnet.com/1948-9366/full/v7/i1/10.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i1.10
Haemorrhoidal disease (HD) is one of the oldest diseases known by mankind. In 1888, Fredrick Salmon defined the surgical technique which is a combination of excision and ligation for haemorrhoids[1]. Today, Milligan-Morgan (Open method) and Ferguson (Closed method) haemorrhoidectomy are commonly used in symptomatic grade 3, 4 HD in particular[2]. The conventional haemorrhoidectomy which is used in the treatment of third and fourth grade haemorrhoids has severe morbidity and long recovery times[3]. Towards the middle of this century, there was a tendency towards non-operative methods because conventional haemorrhoidectomy operations were more painful and they wear away at the patient[4]. In United States, nearly 58% of the patients above years of age are estimated to have this disease and one-third of these are exposed to surgical intervention[5]. Since there is no smooth muscles on the walls of the vascular structures that constitute HD, it was shown that they were sinusoidal structures and haemorrhages resulted from perisinusoidal arteriolar. Three theories were suggested as of the twelfth century, which are namely varicose veins theory, vascular hyperplasia and anal cushions’ slide out theory. Thompson’s anal cushions’ slide out theory with detailed anatomic studies has been the most accepted theory. The treatment contains diet arrangement, medical treatment, non-operative treatment and operative treatment. Sclerotherapy, Infrared coagulation, rubber band ligation and radiofrequency ablation can be listed among the most commonly used non-operative treatments. The most commonly used operative methods are conventional haemorrhoidectomy, stapler haemorrhoidectomy, plication and doppler-guided haemorrhoidal artery ligation (DGHAL)[6]. Being a treatment method which does not contain tissue excision and necrosis, Vascular Z ligation technigue (VZLT) ensures vascular ligation, fixation and mucopex by a single suture. This study of ours aims to define this technique and present its effect on the postoperative morbidity and recovery process in the surgical treatment of HD.
Among 138 patients with 2nd-4th grade internal HD having several complaints and operated at our hospital between 2003 and 2013; 116 patients who regularly attended 1-year control were included in the study. The patients were explained the informed patient consent which involved extensive information about the operation made and presented alternative methods and their permissions were obtained.
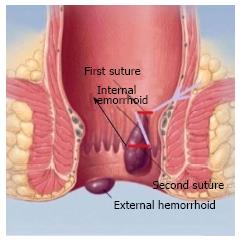
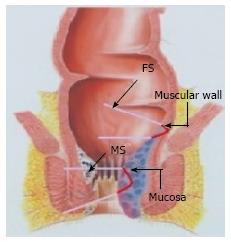
The patients were operated under spinal anaesthesia without applying preoperative enema by applying 1 g cefazolin IV in gynaecological position. The technical drawing of the process can be seen in Figures 1 and 2. The first leg of the Z-shaped suture is constituted by the fixed suture. Fixed suture passes by the mucosa and muscular layer from the root of the enlarged and prolapsed sinusoidal network. The second leg of the Z-shaped suture is constituted by the mobile suture; it is put such that it passes by the piles mucosa and submucosa which prolapses 5-10 mm below the first suture. 3/0 round 26 mm polyglactin (vicryl®Ethicon) was used as suture material. This process was applied on nearly three to four piles. Fixed suture ensures vascular ligation and fixation, mobile suture hangs up the venous piles.
Operation times, preoperative early period Visual Analogous Scale (VAS), satisfaction score and complications were obtained from the computer records retrospectively. The most commonly used one for the pain score was VAS (0 = no pain, 10 = intense pain), and numeric scale (0 = not satisfied and 5 = very satisfied) were used as the satisfaction score. Numeric scores were applied on the patients on the 3rd, 7th and 21st days. While complications such as haemorrhage, infection, urinary retention and incontinence were question in the acute period, anal stenosis was questioned in the 3rd month. The patients’ complaints were questioned at the monthly controls and they were evaluated for recurrence. Haemorrhage, pain and new pile formation were considered relapse.
All data was recorded in SPSS® for Windows (version 21-Chicago, IL, United States) for analysis. The statistical review of the study was performed by a biomedical statistician and statistical review is performed before the submission. The statistical methods of this study were reviewed by M. Sinan IYISOY from Selcuk University, Faculty of medicine, Department of Medical statistics.
Seventy-five of the patients (65%) were male, 41 of them (35%) were female and their age average was 41. The demographic and other characteristics of the patients can be seen in Table 1. Third grade haemorrhoid was found in 63 (54%) of the patients.
| n (%) | Median (range) | |
| Gender | ||
| Female | 41 (35) | 43 (19-55) |
| Male | 75 (65) | 38 (18-65) |
| Hemoroit grade | ||
| Grade 2 | 11 (10) | |
| Grade 3 | 63 (54) | |
| Grade 4 | 42 (36) |
The most frequent complaint of the patients (41 patients) was haemorrhage only. The number of patients who had anal itching (Patients with soiling) and discomfort was 15 (Table 2). The mean operation time was 12 min, and follow-up time was 13 mo.
| Mean (range) | Pain (%) | Hemorrhage (%) | Pain + Hemorrhage (%) | Soiling (%) | |
| Complaints | 24 (21) | 41 (35) | 36 (31) | 15 (13) | |
| Operative time | 12 min (3-23) | ||||
| Follow-up time | 13 mo (8-19) |
The preoperative image of the patient with Grade 4 HD can be seen in Figure 3 and the postoperative one can be seen in Figure 4. The VAS pain score of the patients on the third day was 2.2 while it regressed to 1.2 on the twenty-first day. None of our patients required narcotic analgesics. Satisfaction score was beyond 4 between the third and twenty-first days. Five of our patients developed acute haemorrhage which did not require surgical treatment and blood transfusion and could be kept under control by medical treatment in 1 wk on average. Eight of our patients who mostly consisted of males and developed urinary retention were only attached urethral catheter and followed and they recovered in three days on average. No anal stenosis was observed in any of the patients in the controls in the third month (Table 3). Four of our patients developed relapse. There were grade 2 haemorrhoid in all patients which developed relapse. Three of them had symptoms of pain and haemorrhage and one of them had only haemorrage. Earliest relapse occured in three months and the only symptom was rectal haemorrhage. The other relapses occured in 5th, 7th, 12th months.
| n (%) | 3rd day (range) | 7th day (range) | 21st day (range) | |
| VAS | 2.2 (1-6) | 1.8 (1-4) | 1.2 (1-4) | |
| SS | 4.3 (2-5) | 4.0 (2-5) | 4.4 (2-5) | |
| Acut hemorrhage | 5 (4.3) | |||
| Infection | 2 (1.6) | |||
| Urinary retention | 8 (6.9) | |||
| Anal stenosis | 0 | |||
| Recurrence | 4 (3.5) |
Patients with relapse recovered by medical treatment and there was no need for reoperation.
The purpose of most methods which have been developed until today for the surgical treatment of HD is based on things such as reducing the blood flow of haemorrhoids, keeping excess haemorrhoidal tissue away and fixing the remaining mucosa and anoderm on the tissue below[7]. The treatment of the symptomatic haemorrhoids which did not give response by change in diet and medical treatment is usually made by non-operative or operative methods. Before planning an interventional process for the treatment of HD, it is essential to determine indication whole and complete. In a study which was done in Cleveland, the correct diagnosing rate of surgeons in benign perianal pathologies was found as 70.4%. This study is an important one in that it shows misdiagnosis and wrong treatment in 29.6% of the patients[8]. It has been reported that it is wrong not to immediately apply surgical treatment to the patients with haemorrhoidal prolapsus only[9]. Non-operative methods can be applied to the patients with symptomatic grade 1, 2 and selected grade 3 HD. Surgical treatment can be preferred in the HD where these treatments fail or complications emerge. Surgical treatment might vary based on the physiopathology of HD. While haemorrhoidectomy method is preferred in the HD which emerges upon the slide out of the anal cushion, stapler haemorrhoidopexy can be preferred in the HD which is accompanied by rectal mucosa prolapsus. If HD emerges as a result of arteriovenous hyperperfusion in the haemorrhoidal pile, these patients can be applied DGHAL technique as the surgical treatment[6]. As a result of eighteen prospective randomized studies, it was found that haemorrhoidectomy was the most effective method in the surgical treatment of HD. However, high complication (particularly such as pain, urinary retention, haemorrhage) rates and long-term job loss are the most important problems[10].
Although minimal invasive VZLT that we used in our study is an operative method, vascular ligation, fixation and mucopexy are ensured by a single suture without making tissue excision. VZLT is similar to DGHAL technique with the suture which is put on the root of haemorrhoid, and it is similar to rubber band ligation in collecting the piles. However, severe septic complications can emerge dependent on the necrosis tissue which generates in the distal of the band in the rubber band ligation technique. The success rate of rubber band ligation at 1-2 degree HD is 65%-75% and new bandings can be required in the later periods[11]. No severe septic complication was observed in our study. Vacuum effect can sometimes draw anoderm into the band during rubber band ligation application and severe pains can emerge as a result. In our technique, it is less likely to take anoderm inside because mobile suture is passed through by seeing the mucosa. In our technique, while applying fixed suture on the root of the haemorrhoid, no expensive tool is required as in the DGHAL technique. Giordano et al[12] reported an average operation time of 32 (23-47) min in their study which added mucopexy to the DGHAL technique[12]. Twelve minutes on average is enough for the devascular ligation, fixation and mucopexy process of VZLT. VZLT is an invasive technique as much as non-operative treatment methods. While non-operative treatment methods are mainly applied on internal grade 1-2 HD, VZLT can be applied on all grades of internal HD. But, how come does our technique ensures sufficient mucopexy in grade 4 internal HD without excision? Through the decongestion (diminution) in the distal by the fixed suture (vascular ligation). Five to ten mm hanging process of the mobile suture ensures sufficient mucopexy in the patients as it can be seen in Figure 4. In non-operative and operative methods, the treatment is mostly based on tissue excision, tissue necrosis or mucopexy. Most of the postoperative complications develop dependent to tissue excision and necrosis[9]. As there is no tissue excision and necrosis in our technique, postoperative complications rate is lower and the emerging complications are less severe.
The treatment of HD varies from change in diet to radical surgery according to the grade of haemorrhoid and symptoms. Although the surgical treatment of HD which does not respond to medical treatment is an effective treatment, it can lead to severe complications. Many technological applications have recently become a current issue in order to reduce these complications. The retrospective nature of the study, the lack of comparison with other techniques and the short follow-up time were the limits of the study. The minimal invasive VZLT that is applied by us has higher postoperative patient satisfaction, lower VAS and complication rate. This technique is an easily learnable, applicable and cost efficient method. Being a minimal invasive method in the surgical treatment of HD, we think VLZT can be safely and effectively applied.
Many surgical therapy methods were defined due to the unpredictable complications occurred in the surgical post-therapy period of the hemorrhoidal disease. The anatomic structure, physiology of the site and the contamination factors are increasing the unexpected complication ratios. Vascular Z ligation technigue (VZLT) is an innovative method developed in order to minimize these complications which are annoying both the patient and the surgeon.
The background of the surgical therapy of hemorrhoidal disease lays on the fixation of the sagged mucosa and Pake resection. In the VZLT used by the authors, the fixation is ensured by the first sutures while the suspending of the Pake is ensured by the second sutures.
The authors’ technique does not involve the sagged Pake resection which is responsible for a large part of the postoperative complication. The innovation of this technique is that the fixation of the mucosa and hanging of the Pake is achieved through minimum sutures.
VZLT may be safely applied in the surgical therapy of symptomatic hemorrhoidal disease due to its easy applicability and high postoperative patient comfort.
Haemorrhoids are normally venous structures located in the anal region. The hemorrhoidal disease occurs as a result of their expansion and sagging. Z a patterned suture is a technique.
Haemorrhoidal plication has been used as one of effective surgical treatments for advanced internal haemorrhoids.
P- Reviewer: De Nardi P, Lee FYJ, Lohsiriwat V, Santoro GA S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Ellesmore S, Windsor AC. Surgical History of Haaemorrhoids. Surgical Treatment of Haemorrhoids. London: Springer 2002; 1-4. [DOI] [Full Text] |
| 2. | Agbo SP. Surgical management of hemorrhoids. J Surg Tech Case Rep. 2011;3:68-75. [PubMed] |
| 3. | Khanna R, Khanna S, Bhadani S, Singh S, Khanna AK. Comparison of Ligasure Hemorrhoidectomy with Conventional Ferguson’s Hemorrhoidectomy. Indian J Surg. 2010;72:294-297. [PubMed] |
| 4. | Hulme-Moir M, Bartolo DC. Hemorrhoids. Gastroenterol Clin North Am. 2001;30:183-197. [PubMed] |
| 5. | Cohen Z. Symposium on outpatient anorectal procedures. Alternatives to surgical hemorrhoidectomy. Can J Surg. 1985;28:230-231. [PubMed] |
| 6. | Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol. 2012;18:2009-2017. [PubMed] |
| 7. | Beck DE. Hemorrhoids. Handbook of colon rectal surgery. 2nd ed. New York: Marcel Dekker Inc 2003; 325-344. |
| 8. | Grucela A, Salinas H, Khaitov S, Steinhagen RM, Gorfine SR, Chessin DB. Prospective analysis of clinician accuracy in the diagnosis of benign anal pathology: comparison across specialties and years of experience. Dis Colon Rectum. 2010;53:47-52. [PubMed] |
| 9. | Korkut MA, Çalışkan C, Ünsal MG. Current Therapeutical Approach for the Treatment of Haemorrhoideal Disease. TKRCD. 2009;19:53-63. |
| 10. | Cataldo P, Ellis CN, Gregorcyk S, Hyman N, Buie WD, Church J, Cohen J, Fleshner P, Kilkenny J, Ko C. Practice parameters for the management of hemorrhoids (revised). Dis Colon Rectum. 2005;48:189-194. [PubMed] |
| 11. | Beck D, Roberts P, Rombeau J, Stamos M, Wexner S. Benign Anorektal: Hemoroids. USA: Springer 2009; 225-259. |
| 12. | Giordano P, Tomasi I, Pascariello A, Mills E, Elahi S. Transanal dearterialization with targeted mucopexy is effective for advanced haemorrhoids. Colorectal Dis. 2014;16:373-376. [PubMed] |