Published online Sep 27, 2014. doi: 10.4240/wjgs.v6.i9.183
Revised: July 4, 2014
Accepted: July 17, 2014
Published online: September 27, 2014
Processing time: 174 Days and 5.7 Hours
Gastric necrosis is a rare condition because of the rich blood supply and the extensive submucosal vascular network of the stomach. “Gas-bloat” syndrome is a well known Nissen fundoplication postoperative complication. It may cause severe gastric dilatation, but very rarely an ischemic compromise of the organ. Other factors, such as gastric outlet obstruction, may concur to cause an intraluminal pressure enough to blockade venous return and ultimately arterial blood supply and oxygen deliver, leading to ischaemia. We report a case of a 63-year-old women, who presented a total gastric necrosis following laparoscopic Nissen fundoplication and a pyloric phytobezoar which was the trigger event. No preexisting gastric motility disorders were present by the time of surgery, as demonstrated in the preoperative barium swallow, thus a poor mastication (patient needed no dentures) of a high fiber meal (cabbage) may have been predisposing factors for the development of a bezoar in an otherwise healthy women at the onset of old age. A total gastrectomy with esophagojejunostomy was performed and patient was discharged home after a 7-d hospital stay with no immediate complications. We also discuss some technical aspects of the procedure that might be important to reduce the incidence of this complication.
Core tip: Gastric necrosis is a rare condition because of the rich blood supply and the extensive submucosal vascular network of the stomach. “Gas-bloat” syndrome is a Nissen fundoplication postoperative complication that causes gastric dilatation, but very rarely an ischemic compromise of the organ. We report a case of a 63-year-old women, who presented a total gastric necrosis following laparoscopic Nissen fundoplication and we discuss technical aspects of the procedure that are important to prevent this complication.
- Citation: Salinas J, Georgiev T, González-Sánchez JA, López-Ruiz E, Rodríguez-Montes JA. Gastric necrosis: A late complication of nissen fundoplication. World J Gastrointest Surg 2014; 6(9): 183-186
- URL: https://www.wjgnet.com/1948-9366/full/v6/i9/183.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i9.183
The rich blood supply of the stomach preserves this viscera from ischemic events, even after the ligation of all the major vessels[1] (a. gastrica dextra, a. gastrica sinistra, a. gastro-omentalis dextra, a. gastro-omentalis sinistra and aa. gastricae breves). Notwithstanding this fact, acute gastric dilatation accompanied with or without gastric outlet obstruction[2-7], eating disorders[8-10] or gas-bloat syndrome are recognized causes of ischemic gastric necrosis.
The gas-bloat syndrome is defined as a variable group of symptoms resulting from the inability to relieve gas from the stomach after fundoplication. It’s incidence may vary from 1% to 85%[11]. Gastrointestinal gas may proceed either from an excessive production (carbohydrate or fat rich food, small intestinal bacterial overgrowth) or from an excess of swallowed air (disphagia secondary to orophagryngeal or esophageal motility disorders or anxiety disorders with inefficient chewing, gastroesophageal reflux disease, etc.). The predominant complaint is bloating, but other symptoms include abdominal distention, early satiety, nausea, upper abdominal pain, flatulence, inability to belch, and inability to vomit[11]. Antireflux surgery may contribute to the obstruction of gas blow into the esophagus by means of different mechanisms[12] (surgically altered physiology of the gastroesophageal junction, surgical injury to the vagus nerve, mechanic compression of the wrap), specially when associated to previous gastroesophageal motility disorders, such as delayed gastric emptying.
Delayed gastric emptying is a preexisting condition in many of the patients undergoing antireflux surgery. It is associated with gastroesophageal reflux disease (GERD) in up to 40% of patients, but Nissen fundoplication is known to accelerate gastric emptying and has a high rate of success controlling GERD-related symptoms[13], thus delayed gastric emptying is not a contraindication for antireflux surgery[14]. Nevertheless, a thoughtful preoperative assessment of esophagogastric motility with barium swallow is mandatory and may identify a subset of patients that will still have symptoms related to motility disorders postoperative.
Very few cases of near-total or total gastric necrosis following Nissen fundoplication have been reported. We present a case of gastric necrosis following laparoscopic Nissen fundoplication and pyloric obstruction by a phytobezoar.
A 63-year-old women was admitted to our Emergency Room with a history of sudden abdominal pain, without nausea or vomiting. No other symptoms were reported. Past medical history revealed acetylsalicylic acid intolerance, osteoporosis, supraspinatus rupture and gastroesophageal reflux disease secondary to a type I hiatal hernia, with a normal barium swallow esophagogastric motility pattern, a DeMeester of 33.1 and pathologic acid-clearance in pH-metry and a mild hypotonic lower esophageal sphincter in manometry, for which she underwent laparoscopic Nissen fundoplication 7 mo ago, with no postoperative complications and a 3-d hospital stay. The surgical record described a Rossetti-Nissen fundoplication without diversion of short gastric vessels (SGV), with a short wrap (3 cm) and suturing of the valve to the right crura. Treatment history revealed no medication that could interfere with upper digestive tract motility.
On physical examination, she was conscious, alert and oriented. Blood pressure was 123/75 mmHg with a pulse rate of 76/min. The abdomen was distended, painful to palpation with generalized peritonism and involuntary guarding in the epigastrium. Bowel sounds were diminished. Laboratory findings revealed: hemoglobin, 14.6 g/dL; hematocrit, 44.7%; white blood cell count, 18900/μL (with 15500 neutrophils); platelet count, 372000/μL; lactic dehydrogenase and amylase were elevated to 251 U/L (normal, 87-246 U/L) and 564 U/L (normal, 25-115 U/L), respectively. Arterial blood gases showed a metabolic acidosis with a blood pH of 7.23.
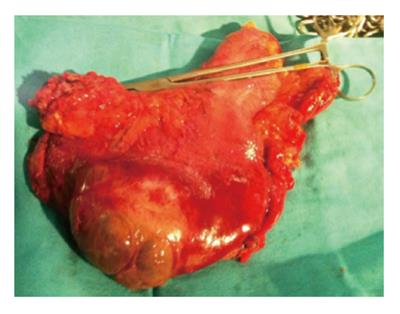
The patient was taken to the radiology department and plain abdominal films were performed (Figure 1). A gastroscopy was performed after X-rays, since a nasogastric tube couldn’t be placed, and a wide area of mucosal necrosis was found in the posterior wall of the lesser curvature (Figure 2). In the operating room an extreme gastric dilatation was found with ischemic changes. The lesser sac was opened and dissection of the posterior gastric surface confirmed endoscopic findings. An anterior longitudinal gastrotomy was performed and trapped air was released. Suction of the gastric chamber through the gastrotomy revealed a phytobezoar in the pyloric channel. Total gastrectomy (Figure 3) with esophagojejunostomy and Roux-en-Y reconstruction was performed. The pathology (Figure 4) revealed a transmural submassive ischemic necrosis with intravascular thrombi. After a postoperative period without complications, the patient was successfully discharged home.
Gastric dilatation is a minor postoperative complication that can eventually occur after major surgery. This condition usually resolves spontaneously or with the insertion of a nasogastric tube for gastric decompression. On the contrary, ischemic necrosis following extreme gastric dilatation is a very rare phenomenon and requires urgent diagnosis and surgical treatment.
Clinical manifestations of the “gas-bloat” syndrome (abdominal pain, distension, tympanic percussion, etc.) are common to many other abdominal pathologies, that without a full comprehension of the surgical history, may delay the diagnosis with the increased morbidity and mortality that this entails. Early surgical consult for the evaluation of patients with abdominal pain and surgical history is vital in the emergency room context and decisive for patient outcome.
In the Nissen antireflux procedure, compression of the distal oesophagus by the gastric wrap is required to ensure the one-way valve effect that prevents gastric reflux. Expelling trapped air and belching is therefore sometimes hindered, resulting in a progressive gastric dilatation. Thanks to the anterograde propulsion, which works as an exhaust valve, this condition is intermittent. When anterograde propulsion is totally or partially blocked, gastric distension progressively tightens the periesophageal wrap, thus increasing the intragastric pressure and compromising blood flow. Some studies have shown that an intragastric pressure greater than 20-30 cm H2O is necessary to cause the occlusion of the gastric luminal blood circulation[15]. Cases of gastric necrosis following acute small bowel obstruction based on adhesions and gastric outlet obstruction based on antral gastric cancer and trichophytobezoar after an antireflux technique[3-5] have been reported. In infants, this rare post Nissen complication has also been described[16]. In the case we present, the trigger event was a phytobezoar causing pyloric obstruction.
Since 1955, when Rudolph Nissen performed his first fundoplication, many other procedures that try to reduce the incidence of postoperative complications, including the “gas-bloat” syndrome, have been developed, without a loss of effectiveness in preventing gastroesophageal reflux disease, as demonstrated in several randomized controlled trials and long case series[17-20].
Nevertheless, due to the lack of long-term effectiveness data, it is hard to recommend one type of fundoplication over an other, and Rossetti-Nissen laparoscopic fundoplication still a valid and widespread procedure with a low rate of postoperative complications[17], when performed by trained surgeons. Some technical aspects during a Nissen fundoplication are important, specially for the novice surgeon, and should be considered to avoid surgery-related complications, including the “gas-bloat” syndrome. This may include a short wrap (typically no more than 2 cm), instead of a long one, or the systematic division of the SGV to facilitate a tension-free wrapping[21,22]. The latter is controversial and some prospective randomized trials have proven the contrary: a higher incidence of gas-bloat syndrome when the SGV are divided[23]. In the case presented, no division of the gastric short vessels was performed, but a floppy fundoplication was achieved, and the patient referred no complaints in follow-ups. So the authors do not consider that the preservation of the gastric short vessels was a contributing factor in this particular case.
An important issue to be also remarked is the importance of identifying patients with anxiety and comfort or binge eating conducts, which could have been disregarded in the preoperative consult, and that could potentially have higher risk of complications in the long term. Antidepressant medication and early psychiatric consult might be necessary.
The only symptom referred by the patient was sudden and intense pain in epigastrium.
Main clinical findings were upper abdominal distension, tympanic percussion and peritoneal irritation.
Differential diagnosis was mainly based on past surgical history: acute gastric dilatation vs small bowell obstruction.
Laboratory findings were congruent with an acute inflammatory process with poor splacnic perfusion: high leukocyte count and high lactic dehydrogenase and amylase.
Plain abdominal X-ray is more than adequate to diagnose gastric distension, but a computed tomography-scan may be also helpful to note ischemic changes and involvement.
Routine Hematoxylin-Eosin stain was performed to find out ischemic tissue injuries.
Surgery was mandatory in this case based on clinical and analytical findings, and a total gastrectomy was performed.
Antireflux surgery, although it might not be of extreme complexity, it is not free of severe complications and common pitfalls such as long or tightened wraps should be avoided. Also, patients with antireflux surgery and anxiety symptoms or eating disorders should be recognized and properly treated with psychiatric consult if necessary.
The case report is useful as it serves to highlight that fundoplication can have serious complications.
P- Reviewer: Beales ILP, Conzo G, Yin YW S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Babkin BP, Armour JC, Webster DR. Restoration of the Functional Capacity of the Stomach when Deprived of its Main Arterial Blood Supply. Can Med Assoc J. 1943;48:1-10. [PubMed] |
| 2. | Aydin I, Pergel A, Yucel AF, Sahin DA, Ozer E. Gastric Necrosis due to Acute Massive Gastric Dilatation. Case Rep Med. 2013;2013:847238. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Powell JL, Payne J, Meyer CL, Moncla PR. Gastric necrosis associated with acute gastric dilatation and small bowel obstruction. Gynecol Oncol. 2003;90:200-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Patuto N, Acklin Y, Oertli D, Langer I. Gastric necrosis complicating lately a Nissen fundoplication. Report of a case. Langenbecks Arch Surg. 2008;393:45-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Lee D, Sung K, Lee JH. Acute gastric necrosis due to gastric outlet obstruction accompanied with gastric cancer and trichophytobezoar. J Gastric Cancer. 2011;11:185-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Glick PL, Harrison MR, Adzick NS, Webb HW, DeLorimier AA. Gastric infarction secondary to small bowel obstruction: a preventable complication after Nissen fundoplication. J Pediatr Surg. 1987;22:941-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Barker JA, Burnett H, Carlson GL. Gastric necrosis complicating acute gastric dilatation after Nissen fundoplication. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Patocskai EJ, Thomas JM. Gastric necrosis in a patient with bulimia. Eur J Surg. 2002;168:302-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Abdu RA, Garritano D, Culver O. Acute gastric necrosis in anorexia nervosa and bulimia. Two case reports. Arch Surg. 1987;122:830-832. [PubMed] |
| 10. | Nakao A, Isozaki H, Iwagaki H, Kanagawa T, Takakura N, Tanaka N. Gastric perforation caused by a bulimic attack in an anorexia nervosa patient: report of a case. Surg Today. 2000;30:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Richter JE. Gastroesophageal reflux disease treatment: side effects and complications of fundoplication. Clin Gastroenterol Hepatol. 2013;11:465-471; quiz e39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 12. | Spechler SJ. The management of patients who have “failed” antireflux surgery. Am J Gastroenterol. 2004;99:552-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Patti MG, Fisichella PM, Perretta S. Preoperative evaluation of patients with gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A. 2001;11:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Bais JE, Samsom M, Boudesteijn EA, van Rijk PP, Akkermans LM, Gooszen HG. Impact of delayed gastric emptying on the outcome of antireflux surgery. Ann Surg. 2001;234:139-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Edlich RF, Borner JW, Kuphal J, Wangensteen OH. Gastric blood flow. I. Its distribution during gastric distention. Am J Surg. 1970;120:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Bass KD, Meagher DP, Haase GM. Gastric necrosis after fundoplication: a novel approach for esophageal preservation. J Pediatr Surg. 1998;33:1720-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | O’Boyle CJ, Watson DI, Jamieson GG, Myers JC, Game PA, Devitt PG. Division of short gastric vessels at laparoscopic nissen fundoplication: a prospective double-blind randomized trial with 5-year follow-up. Ann Surg. 2002;235:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 79] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Carlson MA, Frantzides CT. Complications and results of primary minimally invasive an-tireflux procedures: a review of 10,735 reported cases. J Am Coll Surg. 2001;193:428-439. [RCA] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 151] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 19. | Anvari M, Allen C. Laparoscopic Nissen fundoplication: two-year comprehensive follow-up of a technique of minimal paraesophageal dissection. Ann Surg. 1998;227:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Watson DI, Pike GK, Baigrie RJ, Mathew G, Devitt PG, Britten-Jones R, Jamieson GG. Prospective double-blind randomized trial of laparoscopic Nissen fundoplication with division and without division of short gastric vessels. Ann Surg. 1997;226:642-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 172] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 21. | Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Guidelines for Surgical Treatment of Gastroesophageal Reflux Disease (GERD). 2010;. |
| 22. | Soper NJ. Fundoplication and the short gastric vessels: divide and conquer. Ann Surg. 2002;235:171-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |