Published online Jul 27, 2014. doi: 10.4240/wjgs.v6.i7.136
Revised: May 5, 2014
Accepted: July 12, 2014
Published online: July 27, 2014
Processing time: 137 Days and 16.6 Hours
AIM: To identify their diagnostic and prognostic clinical characteristics in a large series.
METHODS: Retrospective review of clinicopathologic and imaging characteristics of patients diagnosed with lymphoepithelial cysts and cystic lymphangiomas of the pancreas at Massachusetts General Hospital.
RESULTS: Twelve patients were identified between 1/1/1997 and 8/1/2007. Their median age was 55.5 years (range 19-78 years), and 6 were females. The lesion was incidentally discovered in half of the patients. Contrast enhanced computed tomography demonstrated that the cysts had thin walls, without calcifications, pancreatic duct dilation or pancreatic parenchyma invasion. Endoscopic ultrasound with fine needle aspiration (EUS/FNA) confirmed the diagnosis of a lymphoepithelial cyst in 3 patients, one of whom was spared an operation and continues to do well after 6 years. Eleven patients had a resection: 3 pancreaticoduodenectomies, 7 distal pancreatectomies, and 1 enucleation. The median size of the cysts was 3 cm (range 2-20 cm). At a median follow-up of 57 mo no recurrences or other pancreas-related conditions occurred.
CONCLUSION: Lymphoepithelial cysts and cystic lymphangiomas of the pancreas can be diagnosed with a combination of contrast-enhanced computed tomography scans and EUS/FNA. If the lesion is asymptomatic, an operation might be avoided.
Core tip: Lymphoepithelial cysts and cystic lymphangiomas of the pancreas represent rare, benign cystic lesions. The experience with their diagnosis and treatment is limited mostly to case reports. This report describes our experience with twelve lymphoepithelial cysts and cystic lymhangiomas of the pancreas, analyzing their clinicopathologic characteristics, the role of contrast enhanced computed tomography and endoscopic ultrasound with fine needle aspiration for their diagnosis with an emphasis on non-surgical management when a correct diagnosis can be established in an asymptomatic patient.
- Citation: Konstantinidis IT, Kambadakone A, Catalano OA, Sahani DV, Deshpande V, Forcione DG, Wargo JA, Fernandez-del Castillo C, Lillemoe KD, Warshaw AL, Ferrone CR. Lymphoepithelial cysts and cystic lymphangiomas: Under-recognized benign cystic lesions of the pancreas. World J Gastrointest Surg 2014; 6(7): 136-141
- URL: https://www.wjgnet.com/1948-9366/full/v6/i7/136.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i7.136
The differential diagnosis of cystic lesions of the pancreas includes a variety of inflammatory and neoplastic lesions, some of which have malignant potential, any of which may be symptomatic or not[1].
Among the least known pancreatic cystic lesions are the lymphoepithelial cysts and the cystic lymphangiomas[2]. Their natural history is unknown, but asymptomatic cysts might be left alone if diagnosed accurately. A diagnosis may be possible with a combination of imaging and endoscopic ultrasound with fine needle aspiration (EUS/FNA).
In this study we report our experience with twelve patients diagnosed with lymphoepithelial cysts or cystic lymphangiomas over a period of more than 10 years, focusing on diagnostic evaluation and surgical treatment and exploring the potential of avoiding an operation on asymptomatic patients.
Review of a pathology database was performed to identify patients diagnosed with lymphoepithelial cysts and cystic lymphangiomas between 1/1/1997-8/1/2007. A prospectively maintained surgical database since 1/2001 was used to identify the relative frequency of the lymphoepithelial cysts and cystic lymphangiomas among the pancreatic cysts who underwent surgical resection.
Clinical data evaluated included gender, age, presenting symptoms, past medical history, laboratory values, operative procedures and pathology reports. The available computed tomography (CT) scans and endoscopic ultrasound studies performed at the Massachusetts General Hospital were re-reviewed. Pancreatic fistula was defined according to the international study group definition[3]. Operative mortality was defined as death within 30 d of the operation.
This study was approved by the institutional review board (IRB) of the Massachusetts General Hospital.
Statistical analysis was conducted using SPSS software (version 20.0; SPSS, Chicago, Ill). Continuous variables are shown as median and range. Categorical or dichotomous data are presented in frequencies and percentage (%) as appropriate. This study was approved by the IRB of the Massachusetts General Hospital (MGH).
Between 1997 and 2007, 12 patients with cystic lymphangiomas or lymphoepithelial cysts were identified, representing approximately 2% of the pancreatic cystic lesions resected during this period. Median age for these 12 patients was 55.5 years (range 19-78) and 6 (50%) were females. The clinicopathologic data of these patients are shown in Table 1. Half of the patients were asymptomatic. Of the 6 symptomatic patients, 4 presented with abdominal pain (two patients presented with severe, abrupt, abdominal pain and the other two with episodes of right lower and left upper quadrant abdominal pain), 1 with fever, and 1 with nausea. One patient had previously undergone resection of ruptured lymphangiomas at an outside hospital 5 and 10 mo prior to presentation. He underwent a distal pancreatectomy for a second recurrence of a retroperitoneal lymphangioma.
| Factors | LECP (n = 8) | Lymphangioma (n = 4) |
| Median age, yr (range) | 60.5 (24-78) | 37.5 (19-69) |
| Females | 2 (25) | 4 (100) |
| Symptomatic | 4 (50) | 2 (50) |
| Abdominal pain | 2 (25) | 2 (50) |
| Other (nausea, fever) | 2 (25) | 0 |
| Operation | 7 (87.5) | 4 (100) |
| Distal pancreatectomy | 4 (50) | 3 (75) |
| Pancreaticoduodenectomy | 2 (25) | 1 (25) |
| Enucleation | 1 (12.5) | 0 |
| Pathology | ||
| Median size, cm (range) | 2 (2-7.6) | 10.5 (2.5-20) |
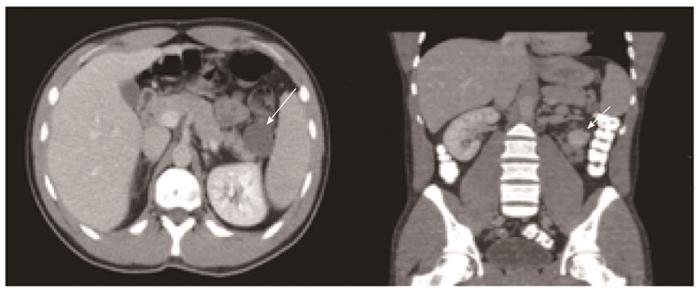
The results of the diagnostic evaluation of these patients are shown in Table 2. All of the patients had normal biochemical studies including serum CA 19-9 levels. Abdominal contrast-enhanced computerized tomography (CECT) scans were available for review in 8 (67%) patients. On CT evaluation, lymphoepithelial cysts/lymphangiomas were seen as low attenuation lesions with thin walls without evidence of calcifications, pancreatic duct dilatation, vascular invasion or enlarged lymph nodes (Figure 1). Cyst septa were evident in most of the cysts (62.5%), and there was a mural nodule in one cystic lymphangioma.
| Factors | LECP(n = 8) | Lymphangioma(n = 4) |
| Median CA 19-9, U/mL (range) | 35 (3-79) | 10 (9-36) |
| CT characteristics | ||
| Mean size, cm (range) | 2.3 (1.5-2.9) | 9.2 (2.3-16.5) |
| Loculations | 1 (25) | 0 |
| Microcystic | 1 (25) | 0 |
| Central scar | 0 | 0 |
| Septations | 3 (75) | 2 (50) |
| Calcifications | 0 | 0 |
| Mural nodules | 0 | 1 (25) |
| Thin cyst wall | 4 (100) | 4 (100) |
| Pancreatic Duct Dilatation | 0 | 0 |
| Other (vascular invasion, lymphadenopathy) | 0 | 0 |
| FNA | (n = 6) | (n = 1) |
| Sufficient | 4 (67) | 1 (100) |
| Diagnostic | 3 (50) | 0 |
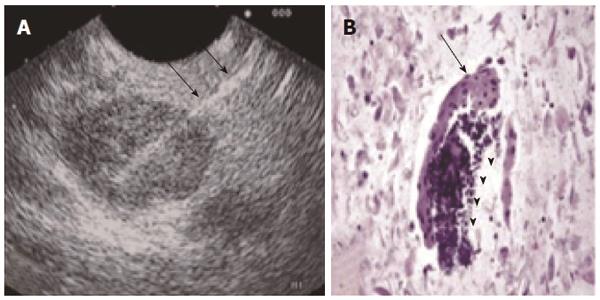
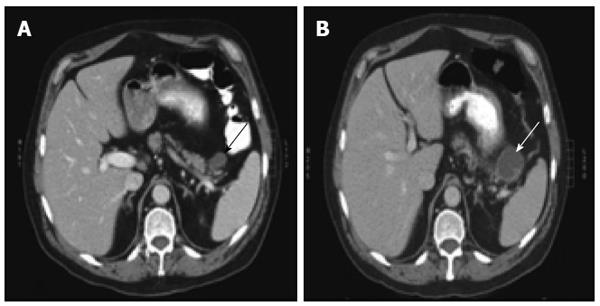
Seven patients (58.3%) underwent an endoscopic ultrasound and fine needle aspiration of the cyst (EUS/FNA). Samples were sufficient for cytology evaluation in 71.4% of patients and led to the diagnosis of a lymphoepithelial cyst in 50% of patients who harbored lymphoepithelial cysts based on demonstration of anucleated squamous cells and a lymphoid component (Figure 2). Based on the EUS/FNA results and stable imaging over the course of 6 years one patient was spared an operation. Two other patients were initially spared an operation with the presumptive diagnosis of a benign cyst but both patients eventually underwent a resection due to an increase in cyst size or the suspicion of nodules on subsequent imaging (Figure 3). Histological examination confirmed a lymphoepithelial cyst and a lymphangioma in these cases.
The operations performed included 3 pancreaticoduodenectomies, 7 distal pancreatectomies and 1 enucleation. There was no operative mortality. Pancreatic fistulas developed in two patients after Whipple operations for lymphoepithelial cysts (1 grade A and 1 grade B fistula). At a median follow up of 56.6 mo (range 1-148 mo) no recurrences or other pancreas-related conditions occurred in any of the eleven patients; all of them remain asymptomatic.
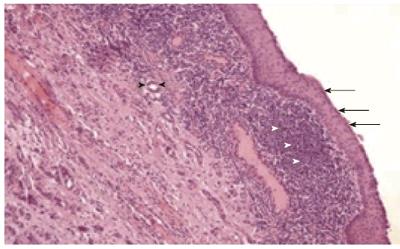
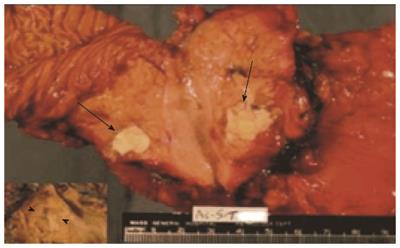
Pathologic assessment of the resected specimens confirmed seven lymphoepithelial cysts and four cystic lymphangiomas (Figure 4). The macroscopic appearance of lymphoepithelial cysts demonstrated a cyst filled with characteristic keratinaceous, cheesy material (Figure 5). Cystic lymphangiomas were filled with chylous fluid consistent with lymph. Median size of the cysts at pathologic review was 2 cm, with a range of 1.5 to 7.6 cm for the lymphoepithelial cysts and 10.5 cm for the cystic lymphangiomas (range: 2.5-20 cm). One patient had two lymphoepithelial cyst measuring 1.5 cm and 2 cm in size.
The widespread use of abdominal imaging has led to the increasing identification of asymptomatic pancreatic cystic lesions. Seventy-one percent of cysts in a recent report from our institution were serendipitous imaging findings[4]. It becomes likely that uncommon lymphoepithelial cysts and cystic lymphangiomas will increasingly be found incidentally. Although an accurate preoperative diagnosis of pancreatic cysts is not always feasible, criteria associated with an increased risk of malignancy have been established by expert consensus[5] and subsequently validated[6,7] and updated[8]. Establishing a correct diagnosis in a benign asymptomatic cyst can spare the patient a pancreatectomy, which even in specialized tertiary centers carries significant morbidity[9].
This report, representing one of the largest case series describing the clinicopathologic characteristics of lymphoepithelial cysts and cystic lymphangiomas, provides insights into their correct management and spotlights establishment of an accurate diagnosis to avoid an operation in asymptomatic patients. In 3 (50%) of our asymptomatic patients a non-surgical approach was initially chosen on the basis of the probability of a benign lesion in an asymptomatic patient. Two of those eventually underwent resection because of new suspicious imaging findings, but the third continues to do well without intervention during follow-up of 6 years.
Lymphoepithelial cysts of the pancreas are most often found in men in their fifth and six decades of life; 75% of our patients were males who had a median age of 60.5 years. Their characteristic pathologic features are a squamous epithelial lining and surrounding lymphoid tissue, which can be identified on EUS/FNA[1].
Cystic lymphangiomas are benign multicystic lesions that are believed to result from blockage of the lymphatic system and, for unknown reasons, are more common in young females. They can be very large in size and they are frequently located in the peripancreatic tissues in close association with the pancreas. They harbor an endothelial cell lining[10]. In our series four patients were female and had median age of 37.5 years. The largest lesion was 16.5 cm.
The preoperative diagnostic evaluation of the patients in our study included a combination of biochemical and tumor markers, CECT scans of the abdomen and EUS/FNA. Although elevations of serum CA 19-9[11], cyst fluid CA 19-9[12] and persistence of elevated CA 19-9 post-resection[13] have been described in lymphoepithelial cysts, none of our patients had such abnormal levels. Thus, we believe that this marker has no utility in the clinical assessment of these cystic lesions[14]. Consistent with published reports[15], CECT scans in our patients demonstrated cysts with thin walls, without evidence of calcifications, pancreatic duct dilation or local invasion. Cystic lymphangiomas additionally contain septa, appear multiloculated, and may have papillary projections[16]. A mural nodule (which proved to be an organizing hematoma) was seen in one of our patients who had a lymphangioma. On EUS/FNA lymphoepithelial cysts demonstrate anucleated squamous cells on cytology while their pathology is consistent with a keratinized squamous lining with a lymphocytic infiltrate in the cyst wall[1]. This characteristic, identifiable in 75% of the fine needle aspirations in our study, helps the differentiation from other squamous epithelium-lined cysts (dermoid cysts, splenic epidermoid cysts, squamous cell cancer, primary or metastatic)[12,17-20]. The cyst aspirates may be thick, milky, gray or frothy[2]. Cystic lymphangiomas characteristically contain chylous, milky fluid with a very high triglyceride level, commonly > 3000-5000 mg/dL, consistent with lymph. Cytologic features are consistent with lymphoid tissue[21-23]. They are lined by endothelium with immunohistochemical markers including factor VIII-R Ag, CD 31 and CD 34[10].
Our experience with these uncommon benign pancreatic cysts demonstrates that accurate diagnosis may be feasible through a combination of a contrast-enhanced abdominal CT scan and cyst fluid analyses acquired via endoscopic ultrasound and fine needle aspiration. These results can direct the appropriate management strategy, and asymptomatic patients can be spared an operation.
Part of this work was presented at the 2008 Annual Meeting of the American Pancreatic Association November 6-7, 2008 Chicago Illinois.
The treatment of pancreatic cysts is a continuously evolving field. Amongst the least well studied pancreatic cystic lesions are lymphoepithelial cysts and cystic lymphangiomas of the pancreas. Familiarity with their correct diagnosis is crucial as they can be followed non-operatively in asymptomatic patients.
The existing literature on lymphoepithelial cysts and cystic lymphangiomas of the pancreas is limited to case reports. In this report the authors demonstrate our experience with twelve patients, one of the largest single institution experience reported, emphasizing on their correct diagnosis and treatment.
Lymphoepithelial cysts and cystic lymphangiomas of the pancreas can be diagnosed with a combination of contrast-enhanced computed tomography scans and endoscopic ultrasound with fine needle aspiration. Conservative management avoiding a major surgery can be followed as long as the lesions remain asymptomatic.
The description of the experience with the diagnosis and treatment of these rare pancreatic cystic lesions will aid in their safe management.
Lymphoepithelial cysts and cystic lymphangiomas of the pancreas represent rare, benign cystic lesions. Their lining is being characterized by squamous epithelial lining with surrounding lymphoid tissue and endothelial cells respectively.
This is a retrospective study regarding lymphoepithelial cysts or cystic lymphangiomas in 12 patients. This is a very uncommon pancreatic pathology and the paper carries a significant number of patients.
P- Reviewer: Chaib E, Fourtounas C, Li B S- Editor: Song XX L- Editor: A E- Editor: Wang CH
| 1. | Adsay NV, Hasteh F, Cheng JD, Bejarano PA, Lauwers GY, Batts KP, Klöppel G, Klimstra DS. Lymphoepithelial cysts of the pancreas: a report of 12 cases and a review of the literature. Mod Pathol. 2002;15:492-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 105] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Sakorafas GH, Smyrniotis V, Reid-Lombardo KM, Sarr MG. Primary pancreatic cystic neoplasms of the pancreas revisited. Part IV: rare cystic neoplasms. Surg Oncol. 2012;21:153-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula D. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3282] [Cited by in RCA: 3512] [Article Influence: 175.6] [Reference Citation Analysis (34)] |
| 4. | Ferrone CR, Correa-Gallego C, Warshaw AL, Brugge WR, Forcione DG, Thayer SP, Fernández-del Castillo C. Current trends in pancreatic cystic neoplasms. Arch Surg. 2009;144:448-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, Yamaguchi K, Yamao K, Matsuno S; International Association of P. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1539] [Cited by in RCA: 1441] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 6. | Rodriguez JR, Salvia R, Crippa S, Warshaw AL, Bassi C, Falconi M, Thayer SP, Lauwers GY, Capelli P, Mino-Kenudson M. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology. 2007;133:72-79; quiz 309-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 318] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 7. | Pelaez-Luna M, Chari ST, Smyrk TC, Takahashi N, Clain JE, Levy MJ, Pearson RK, Petersen BT, Topazian MD, Vege SS. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol. 2007;102:1759-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 205] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 8. | Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K; International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 1614] [Article Influence: 124.2] [Reference Citation Analysis (0)] |
| 9. | Fernández-del Castillo C, Morales-Oyarvide V, McGrath D, Wargo JA, Ferrone CR, Thayer SP, Lillemoe KD, Warshaw AL. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery. 2012;152:S56-S63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 175] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 10. | Paal E, Thompson LD, Heffess CS. A clinicopathologic and immunohistochemical study of ten pancreatic lymphangiomas and a review of the literature. Cancer. 1998;82:2150-2158. [PubMed] |
| 11. | Yamaguchi T, Takahashi H, Kagawa R, Takeda R, Sakata S, Yamamoto M, Nishizaki D. Lymphoepithelial cyst of the pancreas associated with elevated CA 19-9 levels. J Hepatobiliary Pancreat Surg. 2008;15:652-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Centeno BA, Stockwell JW, Lewandrowski KB. Cyst fluid cytology and chemical features in a case of lymphoepithelial cyst of the pancreas: A rare and difficult preoperative diagnosis. Diagn Cytopathol. 1999;21:328-330. [PubMed] |
| 13. | Yamamoto K, Fujimoto K, Matsushiro T, Ota K. Lymphoepithelial cyst in the pancreas: a case report. Gastroenterol Jpn. 1990;25:758-761. [PubMed] |
| 14. | Tsuchiya Y, Suzuki S, Sakaguchi T, Kojima Y, Okamoto K, Kurachi K, Konno H, Baba S, Nakamura S. Lymphoepithelial cyst of the pancreas: report of a case. Surg Today. 2000;30:856-860. [PubMed] |
| 15. | Kim YH, Auh YH, Kim KW, Lee MG, Kim KS, Park SY. Lymphoepithelial cysts of the pancreas: CT and sonographic findings. Abdom Imaging. 1998;23:185-187. [PubMed] |
| 16. | Leung TK, Lee CM, Shen LK, Chen YY. Differential diagnosis of cystic lymphangioma of the pancreas based on imaging features. J Formos Med Assoc. 2006;105:512-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Bolis GB, Farabi R, Liberati F, Macciò T. Lymphoepithelial cyst of the pancreas. Report of a case diagnosed by fine needle aspiration biopsy. Acta Cytol. 1998;42:384-386. [PubMed] |
| 18. | Liu J, Shin HJ, Rubenchik I, Lang E, Lahoti S, Staerkel GA. Cytologic features of lymphoepithelial cyst of the pancreas: two preoperatively diagnosed cases based on fine-needle aspiration. Diagn Cytopathol. 1999;21:346-350. [PubMed] |
| 19. | Policarpio-Nicolas ML, Shami VM, Kahaleh M, Adams RB, Mallery S, Stanley MW, Bardales RH, Stelow EB. Fine-needle aspiration cytology of pancreatic lymphoepithelial cysts. Cancer. 2006;108:501-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Nasr J, Sanders M, Fasanella K, Khalid A, McGrath K. Lymphoepithelial cysts of the pancreas: an EUS case series. Gastrointest Endosc. 2008;68:170-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Jathal A, Arsenescu R, Crowe G, Movva R, Shamoun DK. Diagnosis of pancreatic cystic lymphangioma with EUS-guided FNA: report of a case. Gastrointest Endosc. 2005;61:920-922. [PubMed] |
| 22. | Dries AM, McDermott J. Diagnosis of cystic lymphangioma of the pancreas with endoscopic ultrasound-guided fine needle aspiration. Am J Gastroenterol. 2008;103:1049-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Applebaum B, Cunningham JT. Two cases of cystic lymphangioma of the pancreas: a rare finding in endoscopic ultrasonography. Endoscopy. 2006;38 Suppl 2:E24-E25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |