Published online May 27, 2014. doi: 10.4240/wjgs.v6.i5.84
Revised: February 12, 2014
Accepted: April 17, 2014
Published online: May 27, 2014
Processing time: 188 Days and 13.6 Hours
In this case report, we discuss single-incision laparoscopic cecectomy for low-grade appendiceal neoplasm after laparoscopic anterior resection for rectal cancer. The optimal surgical therapy for low-grade appendiceal neoplasm is controversial; currently, the options include appendectomy, cecectomy, right hemicolectomy, and open or laparoscopic surgery. Due to the risk of pseudomyxoma peritonei, complete resection without rupture is necessary. We have encountered 5 cases of low-grade appendiceal neoplasm and all 5 patients had no lymph node metastasis. We chose the appendectomy or cecectomy without lymph node dissection if preoperative imaging studies did not suspect malignancy. In the present case, we performed cecectomy without lymph node dissection by single-incision laparoscopic surgery (SILS), which is reported to be a reduced port surgery associated with decreased invasiveness and patient stress compared with conventional laparoscopic surgery. We are confident that SILS is a feasible alternative to traditional surgical procedures for borderline tumors, such as low-grade appendiceal neoplasms.
Core tip: The optimal surgical therapy for low-grade appendiceal neoplasm is controversial. Due to the risk of pseudomyxoma peritonei, complete resection without rupture is necessary. We performed single-incision laparoscopic surgery (SILS), which is reported to be a reduced port surgery associated with decreased invasiveness and patient stress compared with conventional laparoscopic surgery. We are confident that SILS is a feasible alternative to traditional surgical procedures for borderline tumors, such as low-grade appendiceal neoplasms.
- Citation: Fujino S, Miyoshi N, Noura S, Shingai T, Tomita Y, Ohue M, Yano M. Single-incision laparoscopic cecectomy for low-grade appendiceal mucinous neoplasm after laparoscopic rectectomy. World J Gastrointest Surg 2014; 6(5): 84-87
- URL: https://www.wjgnet.com/1948-9366/full/v6/i5/84.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i5.84
Appendiceal mucocele is an uncommon pathology of the appendix (0.08%-0.15% of all appendectomies) that is characterized by the accumulation of mucus in the appendiceal lumen[1,2]. The term mucocele, includes cystadenoma and low-grade appendiceal neoplasm, and is the same as the World Health Organization (WHO)’s classification of low-grade appendiceal neoplasm. Several optimal surgical methods are reported but are still controversial. Complete resection without rupture is definitely necessary because the dissemination of neoplastic cells and mucus in the abdominal cavity, which is often be caused by appendiceal perforation, clinically results in pseudomyxoma peritonei in 10%-15% of cases[3]. Therefore, low-grade appendiceal neoplasms are classified into carcinoma groups in the WHO’s classification. In several reports, the surgical procedures used vary from simple appendectomy to right hemicolectomy[4]. Here, to identify the optimal surgical method to treat appendiceal mucocele, we report the case of a 49-year-old woman with an appendiceal lesion that was laparoscopically resected by a single incision and summarize other cases that involved surgical resections.
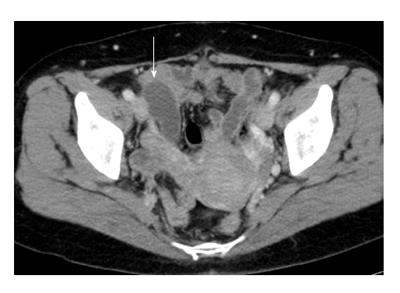
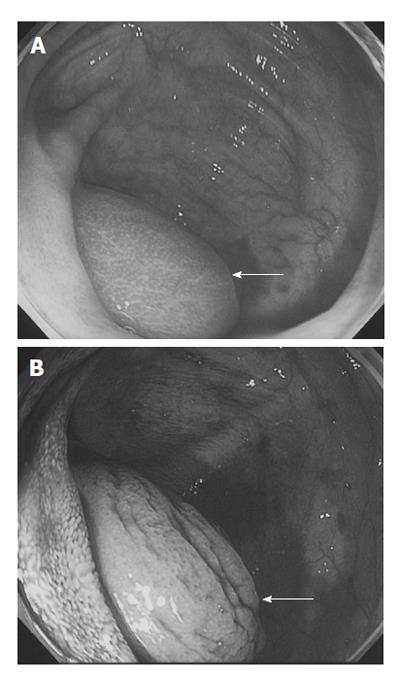
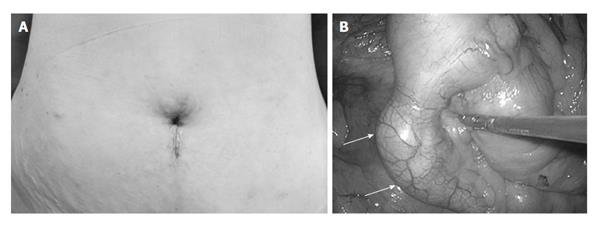
A 49-year-old woman underwent laparoscopic anterior resection for rectal cancer at Osaka Medical Center for Cancer and Cardiovascular Diseases in February 2009. During routine postoperative care, a mucus-filled lesion in the appendix was detected by computed tomography (CT). The patient’s past medical history was not remarkable, except for the rectal cancer. Upon physical examination, there were no remarkable findings. Laboratory tests were within normal ranges. CT revealed a 55 mm × 25 mm tumor that presented as a blind-ended, tubular-shaped, fluid-filled structure in the cecum (Figure 1). Colonoscopy showed that the lesion was covered by normal colonic mucosa in the closed appendix. A colonoscopic biopsy revealed normal mucosa (Figure 2). The lesion was thought to be an appendiceal mucocele of the appendix, and single-incision laparoscopic surgery (SILS) was performed. The surgical choice was made because ultrasound examination showed a movable appendix including the surrounding intestine and no adhesion around the umbilical portion, which had an old scar from the primary operation. Under general anesthesia, the operation started with a trans-umbilical, 2.5 cm-diameter incision (SILS port). A Lap Protector (Hakko Co. Ltd., Nagano, Japan) was folded and the bottom half was inserted into the abdomen through the umbilical incision. The EZ Access (Hakko) was adjusted, and three devices were introduced through it: a flexible laparoscope (Olympus, Tokyo, Japan) and two operating forceps. The pneumoperitoneum was set at 10 mmHg. A smooth and mucus-filled lesion of the appendix was found and there were no ascites or peritoneal nodules indicating malignancy (Figure 3). To excise the tumor without rupture, we cut the peritoneum around the cecum and mobilized it without touching the tumor. After pulling the cecum with the tumor through the SILS port, a cecectomy which included the swollen appendix was performed using a linear stapler (Endo GIA universal; Covidien, Mansfield, MA, United States). The resected bowel contained the appendix (8 cm) and cecum (1 cm). The total operating time was 57 min, and the blood loss was minimal. Histological examination showed low grade epithelial dysplasia, a feature diagnostic of a low-grade appendiceal mucinous neoplasm (Figure 4). Surgical margin was negative and no lymph node metastasis was discovered. The patient recovered without any complications, and was discharged on postoperative day 6. She returned to work, and she is now doing well without any complaint postoperatively.
Appendiceal mucocele itself does not have typical clinical features; more than two-thirds of patients have their appendiceal mucocele removed based on incidental findings, as was the case for our patient[4]. Surgical resection without rupture is necessary, and laparoscopic appendectomy is often used in accordance with the accepted treatment of mucocele[2]. Based on the tumor characteristics, including the location and size, surgical management should differ. Using either an open or a minimally invasive technique still depends on the situation and the preference and experience of the surgeon. Although an open procedure is still recommended in certain appendiceal cases, especially for those with suspected malignancy[5], the laparoscopic technique has been described and recommended as the first choice for treating this disease, rather than conventional open laparotomy. This recommendation is due to the method’s ability to provide useful information regarding the entire abdominal cavity, short recovery post-surgery, and a minimized risk of seeding the tumor during laparoscopic manipulation[6]. Furthermore, SILS has been often applied in several fields, and in colectomies[7-11]. Recent reports show single incision approach through the umbilicus that is called SILS port or grove method. The narrow working space for surgical manipulation for surgical manipulation presents a technical difficulty; however, in certain cases, it is still easy and safe to convert to the conventional laparoscopic surgery with multiple ports or open laparotomy. Laparoscopic surgery has the added benefit of the laparoscope magnifying the surgical field, keeping the surgical space wide by aeroperitoneum. Additionally, in our case, the SILS operation was started but could have been changed to any operation, such as conventional laparoscopic surgery or open surgery, if we had encountered any difficulties (e.g., bleeding, injury to other organs, or difficult surgical manipulation). In a case using the McBurney method, a traditional approach for treating an appendiceal locus with a minimized incision, it would be difficult to change the surgical procedure, leaving only the option of increasing the size of the incision.
We have encountered 6 cases of low-grade appendiceal neoplasm (Table 1); three cases were treated by open surgery for the reason described above, whereas the other 3 cases underwent laparoscopic surgery. In these cases, we chose the appendectomy or cecectomy without lymph node dissection if preoperative imaging studies did not suspect malignancy. In the present case, CT revealed no involvement of the mesoappendix or local lymph node metastasis. All 6 patients are doing well, without recurrence for 6-74 mo after surgery.
| Case | Age (yr)/sex | Chief complaint | Tumor size (mm) | Pathological findings | Operative procedures (lymph node dissection1) | Bleeding (mL) | Operation time (min) | Time after surgery (mo) | Recurrence/survival |
| 1 | 49/F | None | 55 × 25 | Low-grade appendiceal mucinous neoplasm | Single incision laparoscopic cecectomy | 5 | 57 | 6 | None/alive |
| 2 | 61/M | Right lower abdominal pain | 90 × 40 | Low-grade appendiceal mucinous neoplasm | Laparoscopy-assisted ileocecal resection (D3) | 30 | 251 | 14 | None/alive |
| 3 | 61/F | None | 30 × 15 | Low-grade appendiceal mucinous neoplasm | Open appendectomy | 70 | 140 | 25 | None/alive |
| 4 | 81/F | None | 150 × 40 | Low-grade appendiceal mucinous neoplasm | Open ileocecal resection (D3) | 70 | 125 | 29 | None/alive |
| 5 | 69/F | None | 46 × 27 | Low-grade appendiceal mucinous neoplasm | Open appendectomy | 50 | 134 | 32 | None/alive |
| 6 | 51/F | Right hypochondrial pain | 30 × 30 | Mucinous cystadenoma | Laparoscopy-assisted ileocecal resection (D1) | 65 | 280 | 74 | None/alive |
It is thought that minimally invasive procedures, including SILS appendectomy and cecectomy, for low-grade neoplasm, such as mucocele will be considered as the primary treatment choice in several years. The potential benefits include the superior cosmetic results, reduced postoperative pain, faster recovery, and shorter hospital stays.
A 49-year-old woman had no symptom and the disease was detected by computed tomography (CT) during the follow-up course of rectal cancer.
Physical examination shows no remarkable findings.
Appendiceal cancer, carcinoid and cystadenoma.
All laboratory tests were within normal ranges.
CT revealed a 55 mm × 25 mm tumor, which presented as a blind-ended, tubular-shaped, fluid-filled structure in the cecum and colonoscopy showed the lesion covered by normal colon mucosa in the closed appendix.
Histological examination showed low-grade epithelial dysplasia, a feature diagnostic of a low-grade appendiceal mucinous neoplasm.
The tumor was resected by single-incision laparoscopic surgery (SILS).
SILS has been often applied in several fields, and in colectomies.
SILS is used as a reduced port surgery compared to conventional laparoscopic surgery (mostly 5 ports).
This case report shows that SILS is considered as the primary treatment choice for low-grade neoplasm, such as mucocele.
Report is well written. This is an interesting well-described study. The review is well conducted. It addresses an interesting clinical area in an application that has not received a great deal of attention.
P- Reviewers: Chapel A, Ngai TC, Yoldas O S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ
| 1. | Marudanayagam R, Williams GT, Rees BI. Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol. 2006;41:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 158] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Rangarajan M, Palanivelu C, Kavalakat AJ, Parthasarathi R. Laparoscopic appendectomy for mucocele of the appendix: Report of 8 cases. Indian J Gastroenterol. 2006;25:256-257. [PubMed] |
| 3. | Caracappa D, Gullà N, Gentile D, Listorti C, Boselli C, Cirocchi R, Bellezza G, Noya G. Appendiceal mucocele. A case report and literature review. Ann Ital Chir. 2011;82:239-245. [PubMed] |
| 4. | Stocchi L, Wolff BG, Larson DR, Harrington JR. Surgical treatment of appendiceal mucocele. Arch Surg. 2003;138:585-589; discussion 589-590. [PubMed] |
| 5. | Sturniolo G, Barbuscia M, Taranto F, Tonante A, Paparo D, Romeo G, Nucera D, Lentini M. Mucocele of the appendix. Two case reports. G Chir. 2011;32:487-490. [PubMed] |
| 6. | Chiu CC, Wei PL, Huang MT, Wang W, Chen TC, Lee WJ. Laparoscopic resection of appendiceal mucinous cystadenoma. J Laparoendosc Adv Surg Tech A. 2005;15:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Makino T, Milsom JW, Lee SW. Single-incision laparoscopic surgeries for colorectal diseases: early experiences of a novel surgical method. Minim Invasive Surg. 2012;2012:783074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Vestweber B, Galetin T, Lammerting K, Paul C, Giehl J, Straub E, Kaldowski B, Alfes A, Vestweber KH. Single-incision laparoscopic surgery: outcomes from 224 colonic resections performed at a single center using SILS. Surg Endosc. 2013;27:434-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Makino T, Milsom JW, Lee SW. Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg. 2012;255:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 10. | Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC, Delaney CP. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg. 2012;255:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 147] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 11. | Yang TX, Chua TC. Single-incision laparoscopic colectomy versus conventional multiport laparoscopic colectomy: a meta-analysis of comparative studies. Int J Colorectal Dis. 2013;28:89-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Japanese Society for Cancer of the Colon and Rectum (2010). JSCCR Guidelines 2010 for the Treatment of Colorectal Cancer. Tokyo: Kanehara 2010; 13-15. |