Published online Apr 27, 2014. doi: 10.4240/wjgs.v6.i4.70
Revised: October 24, 2013
Accepted: February 20, 2014
Published online: April 27, 2014
Processing time: 315 Days and 20.3 Hours
We reviewed the data of all patients managed for retroperitoneal paragangliomas (PGLs) between June 2010 and June 2011 to present our experience concerning this uncommon entity to highlight diagnostic and therapeutic challenges of retroperitoneal PGLs. All patients were admitted to the department of general and hepatobiliary surgery in the regional hospital of Jendouba, Tunisia. The size of the tumor was taken at its largest dimension, as determined in a computed tomography (CT) scan and pathological reports. There were 4 patients (all women) with a median age of 48 years (range 46-56 years). Abdominal pain was the commonest presentation. CT showed and localized the tumors which were all retroperitoneal. All patients had successful surgical resection of the tumors under invasive arterial blood pressure monitoring. One patient underwent surgery for a presumed tumor of the pancreatic head. The fresh-mount microscopic study of the peroperative biopsy yielded inflammatory tissue without malignancy and no resection was performed. Final histological examination of the biopsy concluded PGL. A second laparotomy was performed and the tumor was entirely resected. The diagnosis was made after surgery by histology in all patients. The control of the blood pressure was improved after surgery in 3 patients. Paragangliomas are rare tumors. The retroperitoneal localization is uncommon. Complete surgical resection remains the only curative treatment but it is often challenging as these tumors are located near multiple vital blood vessels.
Core tip: Retroperitoneal paragangliomas are uncommon tumors causing considerable difficulty in both diagnosis and treatment. Its complete surgical removal is often challenging as these tumors are located near multiple vital blood vessels. Any surgeon could face such a rare tumor.
- Citation: Kallel H, Hentati H, Baklouti A, Gassara A, Saadaoui A, Halek G, Landolsi S, Ouaer ME, Chaieb W, Maamouri F, Mannaï S. Retroperitoneal paragangliomas: Report of 4 cases. World J Gastrointest Surg 2014; 6(4): 70-73
- URL: https://www.wjgnet.com/1948-9366/full/v6/i4/70.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i4.70
Paragangliomas (PGLs), or extra-adrenal phaeochromocytomas, are tumors arising from chromaffin tissues. Abdominal localizations are less frequent than head and neck. Retroperitoneal PGLs are more uncommon, causing considerable difficulty in diagnosis and treatment. In this article, we present our experience concerning this uncommon entity to highlight diagnostic and therapeutic challenges of retroperitoneal PGLs.
We reviewed the data of all patients managed for retroperitoneal PGLs between June 2010 and June 2011. All patients were admitted to the department of general and hepatobiliary surgery in the regional hospital of Jendouba, Tunisia. The size of the tumor was taken at its largest dimension, as determined in a computed tomography (CT) scan and pathological reports.
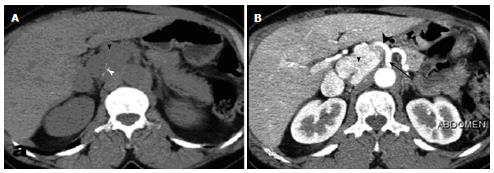
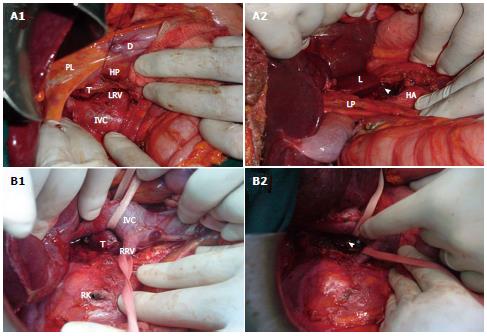
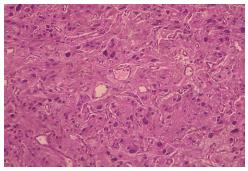
There were 4 patients (all women) with a median age of 48 years (range 46-56 years). The clinical features are shown in Table 1. Abdominal pain was the commonest presentation, followed by hypertension in 3 cases, headache and palpitation in 2 cases and sweating in 1 case. No abdominal mass was detected on palpation in any patient. Abdominal CT showed and localized the tumor in all patients. The tumor measured from 4 to 6 cm in diameter and showed obvious intensification after contrast material administration (Figure 1). All tumors were retroperitoneal. The diagnosis was evoked preoperatively by the CT data for the 3 first patients. Patient 4 underwent surgery for a presumed tumor of the pancreatic head. Surgical exploration revealed a soft mass of the pancreatic head without dilatation of the common bile duct. The fresh-mount microscopic study of the peroperative biopsy yielded inflammatory tissue without malignancy. No resection was performed. Final histological examination of the biopsy concluded PGL. A second laparotomy was performed. The tumor was adherent to the pancreatic parenchyma and the inferior vena cava. It was carefully dissected and entirely resected. Final histological examination of the specimen confirmed the diagnosis of PGL. All patients had successful surgical resection of the tumors under invasive arterial blood pressure monitoring. Complete surgical removal was difficult because the tumors were located near multiple vital blood vessels: celiac region for patient 1 (Figure 2A), right para aortic for patient 2, retrocaval for patient 3 (Figure 2B) and near the pancreatic head for patient 4. There was no evidence of malignancy, as judged by local infiltration or the presence of metastasis. The diagnosis was made after surgery by histology in all cases because of the unavailability of measurements of urinary and plasma adrenaline, noradrenaline and metanephrine concentrations in our hospital. Histology revealed a tumor composed of spindle to polygonal cells with abundant basophilic granular cytoplasm and moderate pleomorphism. The cell architecture was trabecular and nested, pathognomonic of paraganglioma (Figure 3). Low mitotic activity was observed and there was no capsular invasion. The tumor was encapsulated and demarcated from the surrounding effaced pancreatic parenchyma in patient 4. Tumor cells stained positively for synaptophysin, chromogranin and S100 in all cases (Figure 4). The morphological and immunohistochemical profile was consistent with extra-adrenal PGL. The control of the blood pressure was improved after surgery in 3 patients.
| Patient | Age (yr)/sex | Abdominal pain | Hypertension | Palpitation | Headache | Sweating | Location | Size (cm) |
| 1 | 54/F | Y | N | Y | N | Y | Celiac region | 6 |
| 2 | 46/F | Y | Y | N | Y | N | Right para-aortic | 4 |
| 3 | 56/F | Y | Y | Y | N | N | Retrocaval Near right adrenal | 5 |
| 4 | 48/F | Y | Y | N | Y | N | Near pancreatic head | 5 |
Retroperitoneal PGL is a rare pathological entity that occurs most often in young adults[1]. PGLs are often unique; multiple tumors are observed in only 10% of the cases. Signs and symptoms are variable and frequently paroxysmal due to the variable and disorderly release of catecholamines by the tumor. The typical presentation is a combination of variable hypertension with paroxysmal symptoms, either occurring spontaneously or provoked by high abdominal pressure during anteflexion, urination or defecation[2]. The diagnosis of catecholamine-secreting tumors should be based on the determination of plasma or urinary metanephrine concentration[2]. Preoperative imaging tests are used to locate the tumor, to determine whether it is single or multiple, adrenal or ectopic, benign or malignant and isolated or present with other neoplasms in the context of familial syndromes. Magnetic resonance imaging is similar to CT in the diagnosis of PG, but it is preferred in children and pregnant women[2]. Some authors propose 123I-MIBG scintigraphy to diagnose secreting PGLs, with a sensitivity and specificity of 90% and 99% respectively[1]. Complete surgical removal provides a 5 year survival of 75%. It is then considered as the only curative treatment of PGLs[1] but it is often challenging as these highly vascular tumors are located near multiple vital blood vessels. Preoperative pharmacological preparation is necessary. It has an important role in achieving the safest and most successful outcome[3]. Given the hypervascular aspect of the tumor, some authors propose pre-operative embolization. Laparoscopic resection of PGL has been reported in the literature, with all the known advantages of the mini-invasive surgery. In our patients, we performed open surgery because of the localization of the tumor in contact with important vessels. PGLs also have potential to be malignant. It has been reported in the literature that around 20% of PGLs could be malignant with poor survival[4]. While histopathological findings are not very useful to differentiate between benign and malignant PGLs, extensive local invasion and distant metastasis have been used as indicators for malignancy[5-7]. Recurrences and malignancy are more frequent in cases with large or extra-adrenal tumors. Patients should be followed up indefinitely, particularly if they have inherited or extra-adrenal tumors.
In conclusion, paragangliomas are rare tumors with a limited number of cases reported. The localization in the retroperitoneal region is uncommon and is a challenge for surgical resection. Complete surgical resection remains the only curative treatment. Lifetime follow-up is necessary to detect recurrences.
There were 4 patients (all women) with a median age of 48 years (range 46-56 years). Abdominal pain was the commonest presentation. Computed tomography showed and localized the tumors which were all retroperitoneal.
One patient underwent surgery for a presumed tumor of the pancreatic head. The fresh-mount microscopic study of a preoperative biopsy yielded inflammatory tissue without malignancy and no resection was performed. Final histological examination of the biopsy concluded paragangliomas. A second laparotomy was performed and the tumor was entirely resected.
The diagnosis was made after surgery by histology in all patients.
The retroperitoneal localization is uncommon. Complete surgical resection remains the only curative treatment but it is often challenging as these tumors are located near multiple vital blood vessels.
The authors report on a relatively uncommon condition. It would be worth detailing the histopathology and defining how this differs from other retroperitoneal neoplastic lesions.
P- Reviewers: Bassotti G, Freeman HJ S- Editor: Gou SX L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Puche P, Jacquet E, Colombo PE, Jaber S, Alric P, Carabalona JP, Bouyabrine H, Domergue J, Navarro F. Surgical management of a preaortic paraganglioma: Report of one case. Ann Chir. 2006;131:559-563. [PubMed] |
| 2. | Plouin PF, Gimenez-Roqueplo AP. Initial work-up and long-term follow-up in patients with phaeochromocytomas and paragangliomas. Best Pract Res Clin Endocrinol Metab. 2006;20:421-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Niemann U, Hiller W, Behrend M. 25 years experience of the surgical treatment of phaeochromocytoma. Eur J Surg. 2002;168:716-719. [PubMed] |
| 4. | Andersen KF, Altaf R, Krarup-Hansen A, Kromann-Andersen B, Horn T, Christensen NJ, Hendel HW. Malignant pheochromocytomas and paragangliomas - the importance of a multidisciplinary approach. Cancer Treat Rev. 2011;37:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Arrabal-Polo MA, Arrabal-Martin M, Lopez-Leon VM, Abad-Menor F, Valle-Diaz de la Guardia F, Mijan-Ortiz JL, Zuluaga-Gomez A. Spontaneous retroperitoneal abscess as the first clinical manifestation of a non-functioning retroperitoneal paraganglioma. Ann R Coll Surg Engl. 2010;92:W17-W19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Sangster G, Do D, Previgliano C, Li B, LaFrance D, Heldmann M. Primary retroperitoneal paraganglioma simulating a pancreatic mass: a case report and review of the literature. HPB Surg. 2010;2010:645728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Moslemi MK, Abolhasani M, Vafaeimanesh J. Malignant abdominal paraganglioma presenting as a giant intra-peritoneal mass. Int J Surg Case Rep. 2012;3:537-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |