Published online Oct 27, 2014. doi: 10.4240/wjgs.v6.i10.201
Revised: July 30, 2014
Accepted: September 17, 2014
Published online: October 27, 2014
Processing time: 165 Days and 4 Hours
This report describes a young female in her second trimester of pregnancy with known ulcerative colitis on maintenance medical therapy. She was admitted for abdominal pain, and workup revealed a colonic stricture and ulceration with contained perforation. After multidisciplinary discussion she was managed with colectomy and end ileostomy. She delivered a healthy newborn 18 wk after surgery. Only a few prior reports described surgical management of inflammatory bowel disease during pregnancy, with recent results indicating low risk of adverse outcomes.
Core tip: Surgical management of inflammatory bowel disease flare during pregnancy are rare and infrequently reported in the literature. This case report summarizes the literature and describes a successful resection of a contained perforation and stricture secondary to ulcerative colitis flare.
- Citation: Overbey D, Govekar H, Gajdos C. Surgical management of colonic perforation due to ulcerative colitis during pregnancy: Report of a case. World J Gastrointest Surg 2014; 6(10): 201-203
- URL: https://www.wjgnet.com/1948-9366/full/v6/i10/201.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i10.201
Inflammatory bowel disease (IBD) encompasses Crohn’s disease (CD) and Ulcerative Colitis (UC). These autoimmune conditions involve mucosal inflammation of the entire gastrointestinal tract in CD and the colon and rectum in UC. While primary management of IBD is medical, surgical indications are generally reserved for toxic colitis, perforation, bleeding, strictures, neoplasms, and failure of medical management.
Although the rate of IBD flare is similar in pregnant and nonpregnant patients (26%-34%), the primary determinant of disease outcome seems to involve quiescence vs active disease at the initiation of pregnancy[1]. Thus the goal in a planned pregnancy is remission before conception[1]. The optimal drug regimen is patient dependent but the aminosalicylate (mesalamine, balsalazide, sulfasalazine), thiopurine (AZA and 6-MP), and anti-TNF (INF, ADA, CZP) classes are generally considered safe in pregnancy. Active disease is a greater risk than active therapy and timing of dosages can avoid the later weeks of pregnancy to mediate placental transfer of these drugs[1,2].
Initial studies reported an association between IBD and adverse outcomes in pregnant patients, possibly mediated by the immunologic phases of pregnancy and specific interactions leading to preterm birth[3]. Surgical management of ulcerative colitis in an ongoing pregnancy is infrequently reported, with only one recent literature review published[4] and additional case reports. Results showed no mortality reported after 1974, and minimal morbidity[4,5]. Other more generalized reports of IBD relapse during pregnancy indicate a colectomy rate of up to 17%[6]. We report a case of a surgically treated complicated IBD during pregnancy.
Our patient is a 23-year-old female with a 13-year history of UC. She was diagnosed with IBD via symptoms and colonoscopic evidence of disease at ten years of age. Over the last 13 years she has been managed with mesalamine and steroid bursts. She underwent repeat colonoscopy secondary to a stricture in the transverse colon near the splenic flexure in 2012. Biopsies at that time were negative for malignancy and the lumen was viewed to be widely patent.
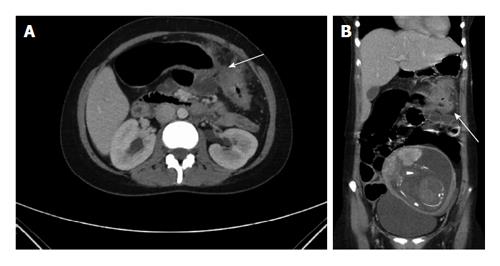
Patient presented to University Hospital at 21 wk of her first pregnancy in April of 2013, with worsening abdominal pain, diarrhea, nausea and intermittent emesis for two months. At the time of admission she was on mesalamine 800 mg bid, and prednisone 30 mg qd, as well as a prenatal vitamin and a proton pump inhibitor. Physical exam revealed a gravid uterus with focal tenderness in the mid epigastric region and the left upper quadrant. Laboratory analysis was significant for leukocytosis at 14.0 × 109/L, erythrocyte sedimentation rate of 75 mm/h and C-reactive protein of 7.0 mg/dL. She underwent a computed tomography scan showing a colonic stricture near the splenic flexure, with dilated proximal colon and a fluid collection surrounding the splenic flexure measuring up to 4.0 cm (Figure 1). She also had a colonoscopy showing a tight, inflamed and friable 8 mm stricture at 45 cm with active ulceration at 35-40 cm. The colonoscope could not be passed through the stricture. Antibiotics were continued from admission (piperacillin-tazobactam and metronidazole), with no signs of hemodynamic instability or sepsis. Multidisciplinary meetings were arranged with gastroenterology, obstetrics and surgery.
Following a week of conservative measures with total parenteral nutrition and no signs of improvement, she underwent a subtotal colectomy (cecum, ascending, transverse, descending, sigmoid colon resected), end ileostomy, and partial gastrectomy due to the colon mass being inseparable from the greater curvature of the stomach. The rectal stump was left in place and oversewn. The fetus was closely monitored.
The post-operative course was uneventful and patient was discharged home on postoperative day five, with steroid taper over the next 7 d. The follow up visit included a normal fetal ultrasound. Pathology revealed diffuse mucosal inflammation (chronic colitis) throughout the colon without skip lesions, with a normal short terminal ileum segment (Figure 2). A colonic ulcer was identified as well as the adherent abscess measuring 5.5 cm. The rest of her pregnancy was uncomplicated and she went on to deliver a healthy infant.
IBD in pregnancy presents a unique challenge. IBD flares can present with symptoms like abdominal pain, hematochezia, or varying degrees of perforation as illustrated by our case.
The goal in treating any IBD flare is to induce remission of the acute flare, and design appropriate maintenance therapy to improve quality of life. Surgical intervention in ulcerative colitis is typically reserved for failure of medical therapy, acute change such as toxic colitis, perforation, bleeding, or the development of strictures or neoplasm. Surgical intervention with a gravid uterus presents several unique challenges[7].
There were two main decision pathways in our case. First, the decision to continue medical management or pursue surgical intervention. With patient’s non-toxic state there was no urgent need for surgery, but due to the stricture and phlegmon, patient would have been unlikely to maintain adequate nutrition without repeat dilation or stenting of the strictured colonic segment. We also had concern for a developing malignancy, since UC may confer an increased risk for developing colon cancer of up to 30%[8]. Furthermore, increasing immunosuppression in the setting of a known perforation and abscess can be risky. This made surgical intervention the preferred approach.
The second decision is which operation is best suited to her case. Diversion only would allow nutritional intake and provide proximal decompression, but would leave a severely inflamed segment of colon in place thus requiring escalation of medical therapy and likely steroids throughout the rest of her pregnancy. The strictured segment of colon would ultimately require resection at a later date anyway. We elected to proceed with a subtotal colectomy. Primary anastomosis was considered too risky under the circumstances, and an end ileostomy eliminated the risk of a possible anastomotic leak. Ileostomy placement in a patient with a gravid uterus must also be given special consideration to avoid obstruction as the abdomen changes in girth[9]. A rectal stump was left in place to allow future reconstruction. Surveillance of the remaining rectal stump is recommended for malignancy concern.
A literature review in 2005 identified only five cases in 25 years at a large referral center, and 37 published cases in the literature for fulminant ulcerative colitis requiring an operation during pregnancy[4]. Although early cases noted a fetal mortality as high as 49%, more recent studies have shown subtotal colectomy and Brooke ileostomy to be safe in the pregnant population[4].
In summary, we successfully managed a case of complicated UC in pregnancy via extended colectomy, partial gastrectomy and end ileostomy. Patient had an uneventful recovery and delivered a healthy newborn a few weeks later. Consideration should be given to surgical resection in cases of complicated UC in pregnant women in well selected cases following multidisciplinary evaluation.
Twenty-three years old pregnant female with known ulcerative colitis presents with abdominal pain, nausea, emesis, and diarrhea for two months.
Physical exam revealed a gravid uterus with focal tenderness in the mid epigastric region and the left upper quadrant.
Differential diagnosis included inflammatory bowel disease flare, gastroenteritis or infectious colitis, diverticulitis, and appendicitis-the next step was to discern via imaging and colonoscopic evaluation.
Laboratory analysis was significant for leukocytosis at 14.0 × 109/L, erythrocyte sedimentation rate of 75 mm/h and C-reactive protein of 7.0 mg/dL.
Computerized tomography revealed a colonic stricture near the splenic flexure, with dilated proximal colon and a fluid collection surrounding the splenic flexure measuring up to 4.0 cm.
Pathology revealed diffuse mucosal inflammation limited to the colon and rectum, with a normal short terminal ileum segment. A colonic ulcer was identified as well as the adherent abscess measuring 5.5 cm.
Treatment included antibiosis as well as surgical management including subtotal colectomy and end ileostomy.
A literature review in 2005 identified only five cases in 25 years at a large referral center, and 37 published cases in the literature for fulminant ulcerative colitis requiring an operation during pregnancy. Although early cases noted a fetal mortality as high as 49%, more recent studies have shown subtotal colectomy and Brooke ileostomy to be safe in the pregnant population.
An important lesson is that surgical management of complicated inflammatory bowel disease flare can be safe in pregnancy and should be considered in appropriate circumstances.
Authors report a case of a surgically treated complicated during pregnancy. They successfully managed a case of complicated Ulcerative Colitis in pregnancy and this information is important.
P- Reviewer: Cologne KG, Ozkan OV, Pescatori M S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
| 1. | Beaulieu DB, Kane S. Inflammatory bowel disease in pregnancy. Gastroenterol Clin North Am. 2011;40:399-413, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Mahadevan U. Pregnancy and inflammatory bowel disease. Gastroenterol Clin North Am. 2009;38:629-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Nasef NA, Ferguson LR. Inflammatory bowel disease and pregnancy: overlapping pathways. Transl Res. 2012;160:65-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Dozois EJ, Wolff BG, Tremaine WJ, Watson WJ, Drelichman ER, Carne PW, Bakken JL. Maternal and fetal outcome after colectomy for fulminant ulcerative colitis during pregnancy: case series and literature review. Dis Colon Rectum. 2006;49:64-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Wilson IA, Dench J, Garrett WV. Surgical management of ulcerative colitis in an ongoing pregnancy: report of a case and literature review. Int J Colorectal Dis. 2014;29:271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Reddy D, Murphy SJ, Kane SV, Present DH, Kornbluth AA. Relapses of inflammatory bowel disease during pregnancy: in-hospital management and birth outcomes. Am J Gastroenterol. 2008;103:1203-1209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Germain A, Brunaud L. Visceral surgery and pregnancy. J Visc Surg. 2010;147:e129-e135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Rogler G. Chronic ulcerative colitis and colorectal cancer. Cancer Lett. 2013;345:230-234. [RCA] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 277] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 9. | Spring A, Lee M, Patchett S, Deasy J, Wilson I, Cahill RA. Ileostomy obstruction in the third trimester of pregnancy. Colorectal Disease. 2012;14:e631-e632. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |