Published online Jun 27, 2013. doi: 10.4240/wjgs.v5.i6.192
Revised: April 22, 2013
Accepted: May 18, 2013
Published online: June 27, 2013
Processing time: 124 Days and 14.5 Hours
Superior mesenteric artery syndrome is a rare cause of upper gastrointestinal obstruction, and is characterized by 3rd duodenal obstruction between the abdominal aorta and the superior mesenteric artery. Classical symptoms are postprandial epigastric pain, nausea, vomiting, and weight loss, or acute upper gastrointestinal obstruction. We herein describe an unusual presentation, with jaundice due to compression of the common bile duct by the gastric obstruction and dilated duodenum.
Core tip: Superior mesenteric artery syndrome is a rare cause of upper gastrointestinal obstruction, with sometime unusual presentation, as in the present case, obstructive jaundice. Clinicians need to be aware of this rare situation and its main radiographic sign i.e., extraluminal compression of the duodenum between the superior mesenteric artery and the aorta.
- Citation: Jeune F, d’Assignies G, Sauvanet A, Gaujoux S. A rare cause of obstructive jaundice and gastric outlet obstruction. World J Gastrointest Surg 2013; 5(6): 192-194
- URL: https://www.wjgnet.com/1948-9366/full/v5/i6/192.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i6.192
Superior mesenteric artery syndrome is a rare cause of upper gastrointestinal obstruction, and is characterized by 3rd duodenal obstruction between the abdominal aorta and the superior mesenteric artery. This can be due to loss of intra-abdominal fat by malabsorption, cancer, anorexia nervosa, or spinal surgery decreasing aortomesenteric angle and the distance between the superior mesenteric artery (SMA) and aorta. Classical symptoms are postprandial epigastric pain, nausea, vomiting, and weight loss, or acute upper gastrointestinal obstruction. We report an unusual presentation, with jaundice du to compression of the common bile duct by the gastric obstruction and dilated duodenum.
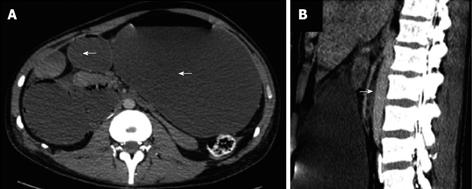
A 31-years old man was admitted in a traumatology unit after a fall from the 3rd floor, and was operated for a thoracic spine injury (without spinal cord injury) requiring a T2-T6 osteosynthesis. Three weeks latter, and after a more than 10 kg weight loss, the patients progressively complain of abdominal discomfort, nausea, vomiting and jaundice. Physical examination only revealed abdominal distension without tenderness in an undernourished and jaundiced patient. Blood work was significant for a bilirubin of 168 mmol/L and eleveted liver enzymes Aspartate Aminotransferase (92 UI/L), Alanine Aminotransferase (109 UI/L), and Gama Glutanyltransferase (288 UI/L). The remainder of his laboratory works was within normal limits. Contrast computed tomography (CT) was performed, revealing a complete gastric outlet obstruction (Figure 1), and elucidated the clinical situation.
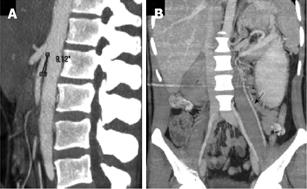
On the basis of clinical presentation and CT scan imaging SMA syndrome was suspected. CT scan reveled distension of the stomach, and the duodenum, with a flat bowel after its pass behind the SMA (Figure 1A). When compared to initial imaging, aortomesenteric angle was decreased to 9° (Figure 1A and 2A), because of the rapid and intense weight loss following surgery, associated with a decreased in retroperitoneal fat thickness. Additionally, because of the chronic gastric outlet obstruction, there either a direct compression of the common bile duct by the distended stomach and duodenum or an increased intraduodenal pressure, responsible for the obstructive jaundice, as proven by the rapid bilirubin and liver function test decreased after nasogastric tube decompression. The mechanism of this upper gastointestinal (GI) obstruction is an extraluminal compression of the duodenum between the SMA and the aorta. This was associated with a left renal vein obstruction with left gonadal vein dilatation (Figure 2B). After nasogastric tube decompression, obstructive jaundice and abdominal discomfort rapidly disappeared. Because of failure of parenteral nutrition and enteral feeding, possibly due to an important catabolism following extensive spine surgery, and anorexia in relation to a depressive syndrome, a Roux-en-Y gastrojejunostomy associated with duodenojejunal flexure lowering (Strong’s procedure) was performed, allowing oral feeding and weight gain within the next weeks.
SMA syndrome is a rare cause of upper gastrointestinal, first described in 1842 by Von Rokitanski, and characterized by 3rd duodenal obstruction between the abdominal aorta and the SMA[1]. This can be due to loss of intra-abdominal fat by malabsorption, cancer, anorexia nervosa, or spinal surgery[2,3] decreasing aortomesenteric angle and the distance between the SMA and aorta. Classical symptoms are postprandial epigastric pain, nausea, vomiting, and weight loss, or acute upper GI obstruction[4]. Biliary symptoms such as in this case have been rarely reported[5].
CT angiography with 3-D reconstruction and oral contrast provides the diagnosis. Diagnostic criteria include: aortomesenteric angle < 20°, aortomesenteric distance < 8 mm, gastric and duodenal dilatation above the third duodenum[6]. Left renal vein compression by SMA and its consequences such as varicocele, hematuria or orthostatic proteinuria, can also been seen so-called nutcracker syndrome[7].
Initial conservative treatment, with nasogastric decompression, electrolytic resuscitation and nutritional support, is successful in more than half of patients and seems to be efficient only in patients with short story of SMA syndrome and mild duodenal stenosis[8]. Two surgical options are indicated after medical treatment failure: obstruction bypass such as duodenojejunostomy and gastrojejunostomy or Treitz’s ligament lowering (the Strong’s procedure) to decompress the duodenum[9]. Clinicians need to be aware of this rare situation and its main radiographic sign, i.e., extraluminal compression of the duodenum between the SMA and the aorta, in order to promptly adapt their therapeutic strategy.
P- Reviewers Lesmana CRA, Zhang Y S- Editor Wen LL L- Editor A E- Editor Lu YJ
| 1. | Merrett ND, Wilson RB, Cosman P, Biankin AV. Superior mesenteric artery syndrome: diagnosis and treatment strategies. J Gastrointest Surg. 2009;13:287-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 202] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 2. | Vitale MG, Higgs GB, Liebling MS, Roth N, Roye DP. Superior mesenteric artery syndrome after segmental instrumentation: a biomechanical analysis. Am J Orthop (Belle Mead NJ). 1999;28:461-467. [PubMed] |
| 3. | Kepros JP. Superior mesenteric artery syndrome after multiple trauma. J Trauma. 2002;53:1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg. 2007;24:149-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 234] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 5. | Arbell D, Gross E, Koplewitz BZ, Vromen A, Bar-Ziv J, Udassin R. Superior mesenteric artery syndrome masquerading as recurrent biliary pancreatitis. Isr Med Assoc J. 2006;8:441-442. [PubMed] |
| 6. | Agrawal GA, Johnson PT, Fishman EK. Multidetector row CT of superior mesenteric artery syndrome. J Clin Gastroenterol. 2007;41:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Jones PA, Wastell C. Superior mesenteric artery syndrome. Postgrad Med J. 1983;59:376-379. [PubMed] |
| 8. | Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc. 2010;85:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 322] [Article Influence: 21.5] [Reference Citation Analysis (0)] |