Published online Jun 27, 2013. doi: 10.4240/wjgs.v5.i6.187
Revised: May 16, 2013
Accepted: June 1, 2013
Published online: June 27, 2013
Processing time: 81 Days and 16.4 Hours
AIM: To compare short term outcomes of elective laparoscopic and open right hemicolectomy (RH) in an elderly population.
METHODS: All patients over the age of 70 undergoing elective RH at Ninewells Hospital and Perth Royal Infirmary between January 2006 and May 2011 were included in our analysis. Operative details, hospital length of stay, morbidity and mortality was collected by way of proforma from a dedicated prospective database. An extracorporeal anastomosis was performed routinely in the laparoscopic group. The primary endpoints for analysis were morbidity and mortality. Our secondary endpoints were operative duration, length of hospital stay and discharge destination.
RESULTS: Two hundred and six patients were included in our analysis. One hundred and twenty-five patients underwent an open resection and 81 patients had a laparoscopic resection. The mean operating time was significantly longer in the laparoscopic group (139 ±
36 min vs 197 ± 53 min, P = 0.001). The mean length of hospital stay was similar in both groups (11.2 ± 7.8 d vs 9.6 ± 10.7 d, P = 0.28). The incidence of post-operative morbidities was 27% in the open group and 38% in the laparoscopic group (P = 0.12). Overall in-hospital mortality was 0.8% in open procedures vs 1% in laparoscopic.
CONCLUSION: Laparoscopic RH was associated with a significantly longer operative time compared to open RH. In our study, laparoscopic RH was not associated with reduced post-operative morbidity or significantly shorter length of hospital stay.
Core tip: This is the first study to assess open versus laparoscopic right hemicolectomy in the elderly population. Our results, whilst comparable to the published literature, do not show any benefits in terms of operative or short-term outcomes in laparoscopic surgery over open surgery in this particular group of patients.
- Citation: Quyn AJ, Moussa O, Millar F, Smith DM, Steele RJ. Open versus laparoscopic right hemicolectomy in the elderly population. World J Gastrointest Surg 2013; 5(6): 187-191
- URL: https://www.wjgnet.com/1948-9366/full/v5/i6/187.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i6.187
An ageing population and a longer life expectancy has led to an increased number of elderly patients presenting with colorectal cancer requiring surgical management. Since the successful introduction of laparoscopic colectomy by Verdeja et al[1], laparoscopic surgery for the treatment of colorectal cancer has been widely adapted. Laparoscopic colorectal surgery has been shown in many studies to be associated with superior perioperative outcomes when compared to open colorectal surgery with reported advantages including less analgesic requirements, earlier return of bowel function, as well as shorter hospital stay[2,3].
Laparoscopic colectomy in the elderly has also been shown to be safe[4-12], however it is unknown whether elderly patients gain the same benefits from laparoscopic colectomy that younger patients have been shown to receive. Concern regarding laparoscopic colectomy in the elderly population relates to the age-associated increase in co-morbidities, the significantly longer operative times, and the physiologic effects that prolonged time under anaesthesia and CO2 pneumoperitoneum have upon the multiple co-morbid conditions of these patients are unknown[13].
In addition, right hemi-colectomy is a very different operation to other colectomies. The operation does not involve the mobilisation of a difficult flexure and can often be completed through a small transverse incision. Studies have suggested that laparotomy via transverse skin crease incision can provide benefits in terms of ease of operation, reduced postoperative pain, earlier return of bowel function and more rapid discharge from hospital[14].
The aim of this study was to compare the short-term surgical outcomes of laparoscopically-assisted right hemicolectomy (LRH) and open right hemicolectomy (ORH).
All patients undergoing a right hemicolectomy in NHS Tayside (Ninewells Hospital and Perth Royal Infirmary) between January 2006 and May 2011 were included in our analysis. Patients were identified from a dedicated prospective database. Data was collected by way of proforma, this included: (1) patient characteristics (admission date, age, gender, presentation); (2) intervention details (type of surgical intervention, details of surgery, length of procedure, grade of surgeon, total length of hospital stay, date of discharge, discharge destination and whether this was different from admission); and (3) complications, outcome and mortality (including peri-operative and in hospital mortality).
Additional information was reported form detailed case-note review as required. The primary endpoints for analysis were morbidity and mortality. Our secondary endpoints were operative duration, length of hospital stay and discharge destination. Data was reported on an intention-to-treat basis.
Details of the operative procedure have been previously described but are summarised here[15]. All patients were administered prophylactic antibiotics at induction. With LRH a standard four port medial to lateral dissection was performed with high ligation of the ileocolic pedicle. The specimens were either extracted through a right iliac fossa muscle splitting incision or through an extended umbilical incision and an extracorporeal anastomosis performed. An Alexis wound protector (Applied Medical, United States) was used in all cases. An ORH was performed through a transverse muscle cutting incision when possible. A midline incision would be considered if previous laparotomy though a midline incision. A lateral to medial approach with high ligation of the ileocolic pedicle was performed routinely. With both techniques either a side-to-side ileocolic anastomosis or an interrupted end-to-end seromuscular sutured anastomosis was performed at the operating surgeon’s discretion.
There has been no consistent definition of the age cut-off for elderly in the literature. However, several studies evaluating the risks of mortality after colorectal surgery have shown an increased mortality rate after surgery in patients aged more than 70 compared to patients aged less than 70[16,17]. We have thus used the age of
70 years as our cut-off, to evaluate the short-term outcomes of laparoscopic colorectal surgery versus open colorectal surgery in our institution.
Data were processed using the Statistical Package for Social Sciences, version 18.0 (SPSS, Inc., Chicago, IL, United States, 2010). Qualitative variables were summarised by frequency and percentage, while non-normally distributed quantitative variables were described by the median and range. Student’s t-test and Fischer’s exact test as appropriate. Statistical significance was determined (P < 0.05). Data was analysed on an intention to treat basis.
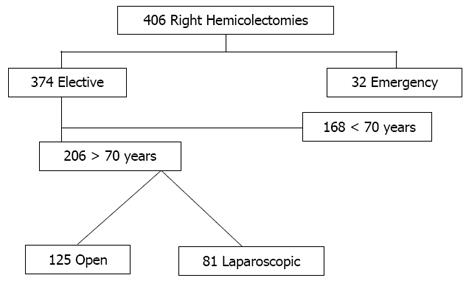
Three hundred and seventy-four patients underwent elective right hemicolectomy during the study period with 206 patients aged 70 years or older (Figure 1). Of these, 106 patients were male. One hundred and twenty-five patients underwent an ORH and 81 patients had a LRH. The clinical and demographic data are summarised in Table 1. There were no significant differences between the two groups. The indication for resection was cancer in the majority of cases. Both groups had a similar distribution of early (stages 1 and 2) and advanced tumours (stages 3 and 4; Table 1).
| Open (n = 125) | Lap (n = 81) | |
| Age, yr (range) | 79 (70-93) | 78 (70-91) |
| Sex (M/F) | 62/63 | 44/37 |
| Cancer stage | ||
| 1 | 21 | 8 |
| 2 | 45 | 29 |
| 3 | 35 | 20 |
| 4 | 3 | 1 |
| Polyp | 18 | 10 |
| Crohn’s disease | 1 | 0 |
Seven patients required conversion to open surgery. Reasons for conversion include dense adhesions from previous surgery and tumour related factors such as local invasion of surrounding structures or anatomic uncertainty. There was a significant difference in mean operating time with 139 ± 36 min in the open group vs 197 ± 53 min in laparoscopic (P = 0.001). The incidence of post-operative morbidities was 27% of open procedures and 38% of laparoscopic procedures (Table 2). Superficial wound infection requiring antibiotics occurred in 10% of ORH and 13% of LRH. The primary site of infection in the laparoscopic group was the extraction site. All incidences resolved with antibiotics. One patient had a deep wound dehiscence in the open group. The incidence of pneumonia and ileus were similar in both groups. Two patients required reoperation in the open group for anastomotic leak related collections. Five patients in the laparoscopic group required re-operation involving laparotomy. One patient required a laparotomy for ischaemic small bowel and four required a laparotomy for anastomotic leak. Overall in-hospital mortality was 1.6% in open procedures vs 1.2% in laparoscopic.
| Open | Laparoscopic | P value | |
| (n = 125) | (n = 81) | ||
| Operative time (min) | 139 ± 36 | 197 ± 53 | 0.001 |
| Length of stay (d) | 11.2 | 9.6 | NS |
| Morbidity | 27% | 38% | NS |
| Wound infection | 13 | 11 | NS |
| Pneumonia | 8 | 9 | NS |
| Ileus | 5 | 6 | NS |
| Urinary infection | 3 | 3 | NS |
| Cardiac event | 4 | 3 | NS |
| Anastomotic leak | 2 | 4 | NS |
| Reoperation | 2 | 5 | NS |
| Mortality | 1.60% | 1.20% | NS |
The mean length of hospital stay was 11.2 ± 7.8 d in open and 9.6 ± 10.7 d in laparoscopic (P = 0.28). Five percent of patients in the open group required transfer to further inpatient facility for further rehabilitation compared to 2% although this failed to reach statistical significance. Long term oncological outcome was not evaluated in this study.
The number of elderly patients presenting with colorectal cancer has paralleled the increased life expectancy in the last decades. This has led to a large, and constantly rising, number of elderly patients with colorectal cancer referred for surgical treatment. Studies have shown that colorectal surgery in elderly patients is generally well tolerated although pre-morbid cardiopulmonary conditions do predispose to higher morbidity and mortality rates as compared to younger patients[5].
Laparoscopic colorectal resection is fast becoming the gold standard of treatment for both malignant and benign colorectal lesions, with improved short-term and comparable long-term outcomes when compared to the open method[2,3,18]. The benefits of laparoscopy have been attributed to less post-operative pain, better pulmonary function and reduced stress response[19-21]. These outcomes are particularly important in elderly patients who are at higher risk of post-operative morbidity and mortality. However, there are concerns regarding the safety of laparoscopic colorectal surgery in elderly patients, mainly related to longer operative time as well as physiological stresses associated with carbon dioxide pneumoperitoneum and steep Trendelenburg required for the main duration of surgery. Hypercapnia, reduce venous return and increase peak airway pressure and decrease pulmonary compliance may all potentially increase the risk of cardio-respiratory complications[22].
Several studies have described laparoscopic colectomy as safe and feasible in the elderly population with reduced morbidity and reduced length of hospital stay when compared to open surgery[5-11] . This is the first study to specifically assess right hemicolectomy in the elderly population. In our series, there was no significant difference in length of hospital stay or morbidity. This conclusion is not drawn from a laparoscopic series which is inferior to other studies as our results are comparable with the published literature[8-11,23]. In addition we have previously published on the benefits of laparoscopic colectomy for cancer in a standard population[15].
The incidence of laparotomy for complications was higher in the laparoscopic group, 6% vs 1% in the open group, however this did not achieve statistical significance possibly relating to the small numbers in this study. We believe that elderly patients undergoing right hemicolectomy do not obtain the same benefits of laparoscopic surgery and that this relates to the very different access required and technical aspects of a right hemicolectomy compared to a left sided resection.
Previous studies comparing methods of right hemicolectomy in a standard population have in fact found no significant difference in post-operative outcomes between laparoscopic resection and open colectomy when performed through a transverse incision[14,24]. Laparoscopy and transverse laparotomy may have various advantages on short- and long-term outcome compared to a midline laparotomy. Patients may experience less postoperative pain, have a better pulmonary function, less wound dehiscence, and significantly less incisional hernias. In addition, two meta-analyses[25,26] have suggested a transverse approach is superior to the midline incision, because of its better anatomical and physiological principles and therefore less prone to develop short- or long-term abdominal wall complications. The duration of hospital stay has often been used as a crude marker of recovery however, in the elderly population there are many factors which prevent satisfactory early discharge and a considerable number of patients require periods of further rehabilitation or additional support at home to enable safe discharge. In the United Kingdom, these factors are often out with the control of the surgeon and nursing staff and require considerable input from social services. Therefore the accepted cost-benefit ratio of laparoscopic surgery may not apply to the elderly population[27].
Laparoscopic RH in an elderly population is feasible and our results would support the evidence from previous studies. However, we found no evidence to suggest that it is better than open RH and believe that the decision regarding the method of operation should reflect local expertise, patient co-morbidities and consideration of expected tolerance of longer operating times and physiological effects of pneumoperitoneum.
In conclusion, our results suggest that laparoscopic RH in the elderly population is associated with a significantly longer operative time compared to open right hemicolectomy and that in our study, laparoscopic RH is not associated with reduced post-operative morbidity or significantly shorter length of hospital stay.
Laparoscopic colorectal surgery is associated with superior perioperative outcomes when compared to open surgery. However, in the elderly population these benefits are often overshadowed by co-morbidities and difficulties in achieving rapid discharge. Right hemicolectomies (RH) represent a distinct group of colorectal resections where the benefits of the laparoscopic approach may be reduced.
Several studies have advocated the use of laparoscopic colectomy in the elderly population. However right hemicolectomy frequently does not involve the mobilisation of a difficult flexure and can be safely achieved through a small transverse incision thus reducing the potential benefits of laparoscopy. Elderly patients often have a reduced physiological reserve due to co-morbidity and exposing them to the additional physiological challenge of pneumoperitoneum may subject them to added risk.
This is the first article to compare open and laparoscopic right hemicolectomy specifically in an elderly population.
Authors found no evidence to suggest that it is better than open RH and believe that the decision regarding the method of operation should reflect local expertise, patient co-morbidities and consideration of expected tolerance of longer operating times and physiological effects of pneumoperitoneum.
This is a comparative study of the short-term results of laparoscopic and open right hemicolectomy in the elderly, which is based on a prospective database. It is indeed the first study to evaluate the two approaches of right hemicolectomy exclusively in the elderly. As such, it represents a novel research and provides sufficient data for scientific conclusions and further investigation. The impact of laparoscopic and open right hemicolectomy in the older population has been unselectively investigated in several studies where older patients were included in patient groups of various ages.
P- Reviewers Chalkiadakis GE, Rangarajan M, Santoro GA S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | Verdeja JC, Jacobs M, Goldstein HS. Placement of drains in laparoscopic procedures. J Laparoendosc Surg. 1992;2:193-196. [PubMed] |
| 2. | Hewett PJ, Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Rieger NA, Smith JS, Solomon MJ, Stephens JH, Stevenson AR. Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg. 2008;248:728-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Abraham NS, Byrne CM, Young JM, Solomon MJ. Meta-analysis of non-randomized comparative studies of the short-term outcomes of laparoscopic resection for colorectal cancer. ANZ J Surg. 2007;77:508-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 445] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 4. | Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Hewett PJ, Rieger NA, Smith JS, Solomon MJ, Stevenson AR. Australasian Laparoscopic Colon Cancer Study shows that elderly patients may benefit from lower postoperative complication rates following laparoscopic versus open resection. Br J Surg. 2010;97:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Chautard J, Alves A, Zalinski S, Bretagnol F, Valleur P, Panis Y. Laparoscopic colorectal surgery in elderly patients: a matched case-control study in 178 patients. J Am Coll Surg. 2008;206:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Yamamoto S, Watanabe M, Hasegawa H, Baba H, Kitajima M. Short-term surgical outcomes of laparoscopic colonic surgery in octogenarians: a matched case-control study. Surg Laparosc Endosc Percutan Tech. 2003;13:95-100. [PubMed] |
| 7. | Faiz O, Haji A, Bottle A, Clark SK, Darzi AW, Aylin P. Elective colonic surgery for cancer in the elderly: an investigation into postoperative mortality in English NHS hospitals between 1996 and 2007. Colorectal Dis. 2011;13:779-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Law WL, Chu KW, Tung PH. Laparoscopic colorectal resection: a safe option for elderly patients. J Am Coll Surg. 2002;195:768-773. [PubMed] |
| 9. | Senagore AJ, Madbouly KM, Fazio VW, Duepree HJ, Brady KM, Delaney CP. Advantages of laparoscopic colectomy in older patients. Arch Surg. 2003;138:252-256. [PubMed] |
| 10. | Stewart BT, Stitz RW, Lumley JW. Laparoscopically assisted colorectal surgery in the elderly. Br J Surg. 1999;86:938-941. [PubMed] |
| 11. | Stocchi L, Nelson H, Young-Fadok TM, Larson DR, Ilstrup DM. Safety and advantages of laparoscopic vs. open colectomy in the elderly: matched-control study. Dis Colon Rectum. 2000;43:326-332. [PubMed] |
| 12. | Tan WS, Chew MH, Lim IA, Ng KH, Tang CL, Eu KW. Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis. 2012;27:773-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Russo A, Marana E, Viviani D, Polidori L, Colicci S, Mettimano M, Proietti R, Di Stasio E. Diastolic function: the influence of pneumoperitoneum and Trendelenburg positioning during laparoscopic hysterectomy. Eur J Anaesthesiol. 2009;26:923-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Tanis E, van Geloven AA, Bemelman WA, Wind J. A comparison of short-term outcome after laparoscopic, transverse, and midline right-sided colectomy. Int J Colorectal Dis. 2012;27:797-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Polignano FM, Quyn AJ, Sanjay P, Henderson NA, Tait IS. Totally laparoscopic strategies for the management of colorectal cancer with synchronous liver metastasis. Surg Endosc. 2012;26:2571-2578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Alves A, Panis Y, Mantion G, Slim K, Kwiatkowski F, Vicaut E. The AFC score: validation of a 4-item predicting score of postoperative mortality after colorectal resection for cancer or diverticulitis: results of a prospective multicenter study in 1049 patients. Ann Surg. 2007;246:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg. 2005;140:278-283, discussion 284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 378] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 18. | Cheung HY, Chung CC, Fung JT, Wong JC, Yau KK, Li MK. Laparoscopic resection for colorectal cancer in octogenarians: results in a decade. Dis Colon Rectum. 2007;50:1905-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Hildebrandt U, Kessler K, Plusczyk T, Pistorius G, Vollmar B, Menger MD. Comparison of surgical stress between laparoscopic and open colonic resections. Surg Endosc. 2003;17:242-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 20. | Huang C, Huang R, Jiang T, Huang K, Cao J, Qiu Z. Laparoscopic and open resection for colorectal cancer: an evaluation of cellular immunity. BMC Gastroenterol. 2010;10:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Veenhof AA, Vlug MS, van der Pas MH, Sietses C, van der Peet DL, de Lange-de Klerk ES, Bonjer HJ, Bemelman WA, Cuesta MA. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg. 2012;255:216-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 22. | Gerges FJ, Kanazi GE, Jabbour-Khoury SI. Anesthesia for laparoscopy: a review. J Clin Anesth. 2006;18:67-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 173] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 23. | Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum. 2005;48:2070-2075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 24. | Veenhof AA, Van Der Pas MH, Van Der Peet DL, Bonjer HJ, Meijerink WJ, Cuesta MA, Engel AF. Laparoscopic versus transverse Incision right colectomy for colon carcinoma. Colorectal Dis. 2010;Sep 21; [Epub ahead of print]. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Grantcharov TP, Rosenberg J. Vertical compared with transverse incisions in abdominal surgery. Eur J Surg. 2001;167:260-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 157] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 26. | Brown SR, Goodfellow PB. Transverse verses midline incisions for abdominal surgery. Cochrane Database Syst Rev. 2005;CD005199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 27. | Hernández RA, de Verteuil RM, Fraser CM, Vale LD. Systematic review of economic evaluations of laparoscopic surgery for colorectal cancer. Colorectal Dis. 2008;10:859-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |