Published online Nov 27, 2013. doi: 10.4240/wjgs.v5.i11.306
Revised: September 17, 2013
Accepted: October 18, 2013
Published online: November 27, 2013
Processing time: 96 Days and 9.9 Hours
We present a case of a 19-year-old man with a 6-year history of Crohn's disease (CD), previously treated with 6-mercaptopurine, who was admitted to our department for Epstein-Barr virus (EBV) infection and subsequently developed a hemophagocytic lymphohistiocytosis (HLH). HLH is a rare disease which causes phagocytosis of all bone marrow derived cells. It can be a primary form as a autosomic recessive disease, or a secondary form associated with a variety of infections; EBV is the most common, the one with poorer prognosis. The incidence of lymphoproliferative disorders was increased in patients with inflammatory bowel disease (IBD) treated with thiopurines. Specific EBV-related clinical and virological management should be considered when treating a patient with IBD with immunosuppressive therapy. Moreover EBV infection in immunosuppressed patient can occur with more aggressive forms such as encephalitis and diffuse large B cell lymphoma. Our case confirms what is described in the literature; patients with IBD, particularly patients with CD receiving thiopurine therapy, who present 5 d of fever and cervical lymphadenopathy or previous evidence of lymphopenia should be screened for HLH.
Core tip: About the case we’re presenting, a literature review showed how this rare disease is often lethal and how low is the percentage of patients who have successful treatment. We show our case history and our management which has permitted to discharge the patient with disease regression.
- Citation: Virdis F, Tacci S, Messina F, Varcada M. Hemophagocytic lymphohistiocytosis caused by primary Epstein-Barr virus in patient with Crohn’s disease. World Journal of Gastrointestinal Surgery 2013; 5(11): 306-308
- URL: https://www.wjgnet.com/1948-9366/full/v5/i11/306.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i11.306
Hemophagocytic lymphohistiocytosis (HLH) is a rare and often fatal disease which causes phagocytosis of all bone marrow derived cells. It can be a primary form as a autosomic recessive disease, or a secondary form associated with a variety of infections; Epstein-Barr virus (EBV) is the most common, the one with poorer prognosis. Patients with inflammatory bowel disease (IBD) are a greater risk of developing secondary HLH due to chronic systemic inflammation condition as well as exposure to immunosuppressive medications[1].
A 19-year-old man was moved to our Hospital from a local hospital in London, where he was admitted 10 d before with a history of fever, jaundice and weakness on a background of Crohn’s disease (CD), which was diagnosed 5 years before and was previously treated with 6-mercaptopurine (6-MP). Diagnosis of EBV infection was performed by serologic exams. During his inpatient stay he developed a progressive pancytopenia (white blood cell 0.5 × 109/L, neutrophils 0.7 × 109/L, hemoglobin 66 g/L, platelets 236.000/mm3), 6-MP therapy was therefore suspended and replaced with steroids. On clinical examination a continuous fever of up to 39 °C was reported. A bone-marrow biopsy was performed to clarify the cause of pancytopenia and it was positive for HLH; diagnosis was thus confirmed matching the diagnostic criteria for HLH (Table 1). Supportive treatment with granulocyte-colony stimulating factor and antibiotics was started. He had been transfused with packed red cells as necessary.
| The diagnosis of HLH may be established by1 |
| A molecular diagnosis consistent with HLH (for example, pathologic mutations of PRF1, UNC13D or STX11 are identified) or |
| Fulfillment of five out of the eight criteria listed below: |
| Fever |
| Splenomegaly |
| Cytopenias (affecting at least two of three lineages in the peripheral blood): |
| Hemoglobin < 9 g/100 mL (in infants < 4 wk: hemoglobin < 10 g/100 mL) |
| Platelets < 100-103/mL |
| Neutrophils < 1-103/mL |
| Hypertriglyceridemia (fasting, 265 mg/100 mL) and/or hypofibrinogenemia (150 mg/100 mL) |
| Hemophagocytosis in BM, spleen or lymph nodes |
| Low or absent NK cell activity |
| Ferritin 500 ng/mL |
| Soluble CD25 (that is, soluble IL-2 receptor) > 2400 U/mL (or per local reference laboratory) |
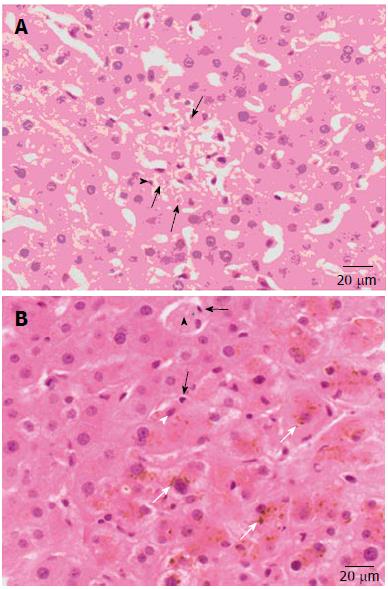
During his recover in our hospital he developed peri-rectal bleeding and a flexysigmoidoscopy showed multiple ulcers but a non specific point of bleeding. Due to this, a computed tomography (CT) angiogram was performed and at that time a bleeding point was identified at the splenic flexure. Hepatosplenomegaly was also noted. Consequently embolization of mesenteric artery was attempt but superior and inferior mesenteric arteries runs did not demonstrate any active bleeding. Moreover, a liver biopsy to exclude other liver diseases has been performed and it showed features consistent with active EBV infection with evidence of hemophagocytosis and no evidence of lymphoma (Figure 1). CT chest was performed and it showed diffuse adenopathy (mediastinal, supraclavicular, bilateral axillary). A right axillary core biopsy showed no evidence of lymphoma. HLH 2004 protocol with Etoposide and Rituximab was therefore started ten days after his admission in our Hospital.
The patient clinically improved from a HLH point of view whilst on the HLH 2004 protocol. However increasing cervical lymphadenopathy was noted and a subsequent biopsy demonstrated diffuse large B cell lymphoma (DLBCL) secondary to EBV. He was therefore started on Cyclophosphamide, Hydroxydaunorubicin, Oncovin, Prednisone chemotherapy. The patient was noted to have two tonic clonic seizures on the ward, one of which resulted in aspiration pneumonia; transfer in intensive treatment unit for intubation and ventilation was required.
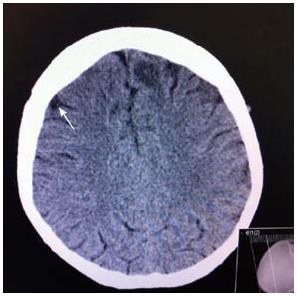
The CT head reported multifocal low attenuation areas of the brain (Figure 2); radiologist report showed as these lesions could have represented central nervous system (CNS) infiltration by the HLH process. However the patient neurological condition was discussed with neurological team and a diagnosis of EBV encephalitis was made. This was treated with Rituximab, Methotrexate, Hydrocortisone and supportive care. His neurological condition improved and the most recent magnetic resonance imaging head showed significant disease improvement. Patient was discharge three months after his admission date.
HLH is a rare, often fatal disease in which macrophages are inappropriately activated resulting in phagocytosis of all bone marrow derived cells[1].
There are two presentation forms: the first, primary, is an autosomic recessive disease; the second is a secondary HLH which can present at any age and has been documented in association with a variety of infections. While there are a wide variety of micro organisms related to the development of HLH, EBV is the most common, the one with poorer prognosis, and the one benefiting most from early treatment with etoposide[2].
The literature review shows how the incidence of lymphoproliferative disorders was increased in patients with IBD treated with thiopurines[3].
However, thiopurines may interfere with the host’s response to a primary EBV infection[1].
EBV can induce HLH; case reports describing HLH and/or lymphoma in patients with CD have also been published[4].
Biank et al[1] described 11 additional cases in the literature of HLH in patient with IBD and only 3 of 11 cases reported were associated with an EBV infection. A new review of literature identified 3 further cases; therefore our case is potentially the seventh described in literature. Our patient met diagnostic criteria for HLH (Table 1).
Moreover he developed CNS symptoms with lesions on the CT head which could represent CNS infiltration by the disease process. CNS symptoms occurs in 35%-49% of patients with HLH[5].
In the case we have reported the patient started etoposide 20 d after his first admission. Etoposide may be life-saving, especially in patients with HLH due to EBV infection; mortality was 14 times higher for patients with EBV-associated HLH who did not receive etoposide within the first 4 wk[6].
Our patient also developed a DLBCL secondary to EBV; in literature we founded only one case involving hepatosplenic lymphoma, HLH and EBV infection in a patient with CD undergoing thiopurine and infliximab therapies[3].
Secondary HLH in patients with IBD is often due to EBV infection. Specific EBV-related clinical and virological management should be considered when treating a patient with IBD with immunosuppressive therapy[4].
Particularly, patients treated with thiopurine have greater risk to develop EBV infection, due to inadequate immune system response. Our case confirms what is described in the literature; patients with IBD, particularly patients with CD receiving thiopurine therapy, who present five days of fever and cervical lymphadenopathy or previous evidence of lymphopenia should be screened for HLH[1].
Moreover EBV infection in immunosuppressed patient can occur with more aggressive forms such as encephalitis and DLBCL.
P- Reviewer: Campo SMA S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
| 1. | Biank VF, Sheth MK, Talano J, Margolis D, Simpson P, Kugathasan S, Stephens M. Association of Crohn’s disease, thiopurines, and primary epstein-barr virus infection with hemophagocytic lymphohistiocytosis. J Pediatr. 2011;159:808-812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Salado CT, Gallego AG, Carnerero EL, De la Cruz Ramírez D, Justiniano JM, Galán JL, Guisado MA. Hemophagocytic lymphohistiocytosis in Crohn’s disease associated with primary infection by Epstein-Barr virus. Inflamm Bowel Dis. 2011;17:E143-E144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Côté-Daigneault J, Bernard EJ. Hepatosplenic lymphoma presenting initially as hemophagocytic syndrome in a 21-year-old man with Crohn’s disease: a case report and literature review. Can J Gastroenterol. 2011;25:417-418. [PubMed] |
| 4. | N’guyen Y, Andreoletti L, Patey M, Lecoq-Lafon C, Cornillet P, Léon A, Jaussaud R, Fieschi C, Strady C. Fatal Epstein-Barr virus primo infection in a 25-year-old man treated with azathioprine for Crohn’s disease. J Clin Microbiol. 2009;47:1252-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Available from: http: //www.startoncology.net/site/index.php?option=com_content&view=article&id=96: hemophagocytic-lymphohistiocytosis&catid=49: histiocyte-disorders-cat&Itemid=53&lang=en. |
| 6. | Janka G, zur Stadt U. Familial and acquired hemophagocytic lymphohistiocytosis. Hematology Am Soc Hematol Educ Program. 2005;1:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 134] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Jordan MB, Filipovich AH. Hematopoietic cell transplantation for hemophagocytic lymphohistiocytosis: a journey of a thousand miles begins with a single (big) step. Bone Marrow Transplant. 2008;42:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 4.5] [Reference Citation Analysis (0)] |