INTRODUCTION
Laparoscopic-assisted colon resection has been well described for multiple surgical indications. Recurrence rates of cancer after laparoscopically-assisted colectomy were similar to those after open colectomy, suggesting that laparoscopic surgery is an acceptable alternative to open surgery[1]. However, this typically requires an abdominal incision for specimen removal, which is commonly associated with postoperative pain. The combination of standard laparoscopy and specimen extraction through a natural orifice has the potential to reduce wound-related complications. We describe the technical approach to laparoscopic ileocecal resection with transanal specimen extraction which avoids an abdominal wall large incision and may be considered as an alternative approach to conventional minimally invasive colectomy, even in patients with right sided flat or small colon lesions.
CASE REPORT
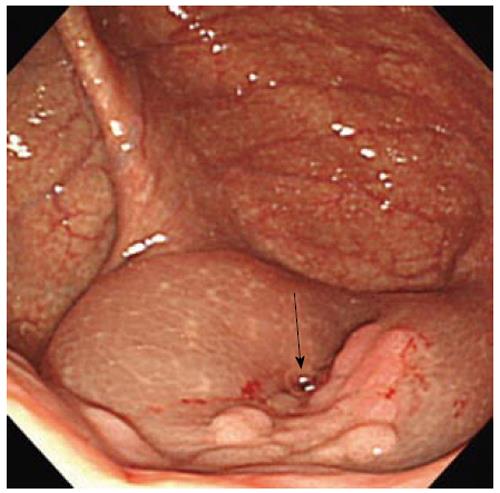
A 71-year old male with a history of chronic obstructive pulmonary disease and asthma complained of lower abdominal pain, which was then explained as a symptom of benign prostate hyperplasia later that day. Colonoscopy revealed a laterally spreading tumor at the cecum that was unresectable by colonoscopy due to the size and location of the lesion. The lesion was 25 mm and was just beside the appendix orifice (Figure 1). We first injected normal saline into below the mucus membrane to try endoscopic submucosal dissection but we gave up resection due to technical difficulty. Pathology of the biopsied specimen showed borderline malignancy. Therefore, we proposed laparoscopic ileocecal resection.
Figure 1 Lesion was beside the appendix orifice (arrow).
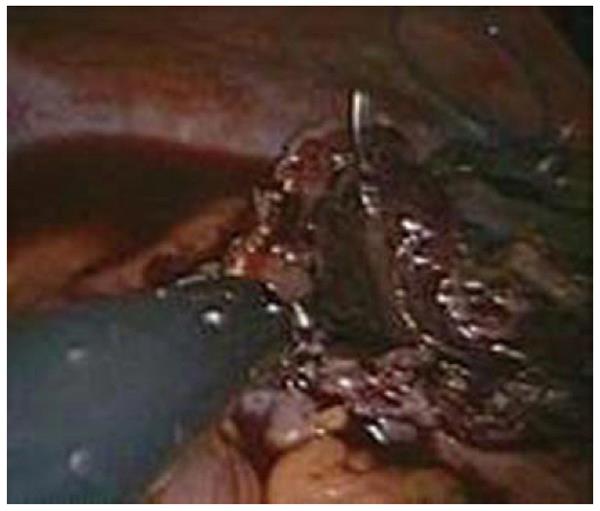
A preoperative oral magnesium citrate bowel preparation was given. After induction of general anesthesia, the patient was placed in the lithotomy position. The colonoscope was inserted in to the cecum in advance. A 15-mm SILS port was placed just caudal to the umbilicus for the 30-degree, 5mm laparoscopy and the flexible forceps. One additional 5-mm trocar was placed in the right upper quadrant. First, the ileocolic artery was identified. A lymph node around the artery was dissected using laparoscopic coagulating shears (LCS) and the ileocolic artery and vein were transected after clamping them with a 5 mm clip. The right colon and ileum were mobilized. The mesocolon was dissected from the terminal ileum to ascending colon where we prepared the distal margin of resection. The level of distal bowel resection was determined via intraoperative colonoscopy, the cecum and ascending colon were irrigated with iodine, and colonoscopy was also performed to ensure complete irrigation during operation. After clamping the laparoscopic bowel clip for the oral side of the cutting point of the terminal ileum, the lesion was transected using a LCS with adequate margins at the anal cut ends. The resected colon was retrieved using snare forceps via colonoscopy through the anus (Figure 2). Next, we made a temporary suture by using a barbed suture (V-Loc, Covidien) at both the oral and anal cut end of anti-mesenteric side of bowel. Then we made a side to side anastomosis with a flexible linear stapler under retraction of the stay suture. Succeeding, we made a continuous closure suture for both the oral and anal open edge (Figure 3). Then we cut out the suture line with the flexible linear stapler to make the intracorporeal functional end to end anastomosis. Finally, we made subcutaneous sutures for the two incisions (Figure 4).
Figure 2 Resected specimen was extracted through the opened colectomy made at the ascending colon using snare forceps via colonoscopy through the anus.
Figure 3 Intracorporeal laparoscopic full thickness V-Loc continuous suturing performed on the oral and anal open ends after side to side anastomosis by a linear stapler.
Figure 4 Post operative scars.
Laparoscopic ileocecal resection was successfully performed using a natural orifice removal approach with two skin incisions. Operating time was 240 min and the estimated blood loss was 28 mL. The resected specimen was 8cm with a 25 mm sized lateral spreading tumor at the cecum. The pathological diagnosis was adenoma with borderline malignancy, the same as the preoperative diagnosis. The patient complained of minimal pain. Oral intake was tolerated on postoperative day 1 and the patient was discharged on postoperative day 4 without complications.
DISCUSSION
These days, even in the colon, endoscopic submucosal dissection is performed safely and reveals good outcomes for wide based lesions such as laterally spreading tumors or early colonic cancers[2,3]. In this case, the lesion was just beside the appendix orifice. Therefore, we thought complete resection was impossible. We then proposed minimally invasive laparoscopic surgery for this patient. Laparoscopic surgery has increased dramatically around the world over the past 20 years and laparoscopic cholecystectomy has become a standard operation in the gall bladder. Furthermore, laparoscopic colectomy has shown favorable results[4] compared with open surgery[5-7]. However, it is still not considered a standard operation because the incision for removing the resected colon is large. In order to standardize laparoscopic colectomy, it is essential to minimize the incision. Therefore, although there is a transvaginal way[8], removal of the resected colon through the anus is the most reasonable way to minimize the incision. Using the anus as a route for specimen colectomy extraction has been described extensively both in experimental and clinical settings[9,10] and some reports describe a series of patients with left-sided malignancies who underwent successful laparoscopic sigmoidectomy and transanal specimen extraction, showing good oncological results[11]. It is true that retrieving the specimen from the right side of colon is more difficult than the left. One report shows a right side single incision operation but the size of scar is 3cm and not pure laparoscopic surgery[12]. A Medline search shows that there are no reports of transanal retrieval of the right side colon, except for the transvaginal route. If the lesion is small or flat, it is not impossible to pull out the lesion from the anus using colonoscopy. Whereas, restricted port, functional end to end anastomosis, which is one of the favorable intracorporeal laparoscopic anastomosis, is quite difficult. To solve this problem, we used two supportive sutures by a barbed suture (V-Loc). One is an anti-mesenteric side by side suture to protect from rotation and slipping out of the bowels from the linear stapler during side to side anastomosis. Another is a continuous closure suture for both the oral and anal open edge. Without this preparation suture before closing cut the colon by linear stapler, the closure of the colon may easily tend to be incomplete. The barbed suture is suitable for this procedure because this suture does not loosen the closed edge and does not require a suture tie. The linear cutter, a flexible equipment grasper, is also useful. In this operation there are some risks of infection due to opening the bowel in the abdominal cavity. To avoid stool leakage during the operation from the both oral and anal side of the colon, complete preparation was performed with iodine during surgery under direct view using colonoscopy. We are already accustomed to similar hybrid natural orifice transluminal endoscopic surgery (NOTES) procedures[13] and have also performed trans anal removal of the distal colon[14,15]. On the other hand, the procedure requires a surgeon with advanced laparoscopic skills and the ability to perform intracorporeal suturing. However, improved skills of laparoscopic surgeons and robotic surgery may resolve these technical issues. Although transanal specimen extraction may not be possible in patients with a small caliber colon or large lesion, pure laparoscopic ileocecal resection is an applicable option for patients requiring elective ileocecal resection or right hemicolectomy and appears to be associated with little incisional pain and rapid recovery. Laparoscopic surgery involving NOTES procedures are still being developed. Therefore, our technique might be feasible as a pre-NOTES technique. More studies on this surgical technique in future will confirm its technical feasibility.
Peer reviewers: A Ziya Anadol, MD, FACS, Gazi University School of Medicine, Department of Surgery, Besevler 06500, Ankara, Turkey; Jiro Watari, MD, PhD, Department of Gastroenterology, Hhogo College of Medicine, 1-1, Mukogawa-cho, Nishinomiya, Hyogo 663-8501, Japan
S- Editor Wang JL L- Editor Roemmele A E- Editor Xiong L