Published online Dec 27, 2012. doi: 10.4240/wjgs.v4.i12.296
Revised: September 23, 2012
Accepted: December 1, 2012
Published online: December 27, 2012
AIM: To evaluate the applicability and safety of ambulatory laparoscopic cholecystectomy (LC) and to compare day case and overnight stay LC.
METHODS: Data were collected retrospectively and consecutively for day case and overnight stay LC patients from July 1, 2009 to April 30, 2011. Outcomes were analyzed for patient demographics, operation time, blood loss during operation and frequency and reasons for unexpected or prolonged hospitalization in each group.
RESULTS: There was no hospital mortality and no patient was readmitted with serious morbidity after discharge. 50 patients received a day case LC and 19 had an overnight stay LC. There was a significant difference in age between both groups (P < 0.02). There were no significant differences between the day case LC performed (n = 41) and failed (n = 9) groups and between the day case LC performed and the one night stay LC (n = 12) groups. There was a significant difference in age between the one night stay and more nights stay LC groups (P < 0.05). Thus, elderly patients showed a tendency to like to stay in hospital rather than being a day case. The proportion of unexpected or prolonged hospitalization was not significantly different between the day case and overnight stay LC groups, when the patient’s request was excluded.
CONCLUSION: Day case LC can be performed with a low rate of complications. In overnight stay patients, there are many who could be performed safely as a day case. Moreover, we need to take special care to treat elderly patients.
- Citation: Sato A, Terashita Y, Mori Y, Okubo T. Ambulatory laparoscopic cholecystectomy: An audit of day case vs overnight surgery at a community hospital in Japan. World J Gastrointest Surg 2012; 4(12): 296-300
- URL: https://www.wjgnet.com/1948-9366/full/v4/i12/296.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i12.296
Laparoscopic cholecystectomy (LC) has now become the standard procedure for the surgical treatment of symptomatic gallstone patients[1,2]. Because of the smaller scars and reduced postoperative pain, introduction of the LC procedure has resulted in a shorter hospital stay, a shorter period of convalescence and an earlier return to work. LC has been performed regularly as ambulatory surgery in patients with uncomplicated gallstone disease in the United States[3] and parts of Europe[4]. Ambulatory LC is performed in one hospital by day case[5-7], while in another hospital by overnight stay[8,9]. Both have not yet to gain acceptance in Japan.
The aim of this retrospective study was to evaluate the applicability and safety of ambulatory LC at a community hospital in Japan and to compare between day case and overnight stay LC.
This work was carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved ethically by the Nagoya Kyoritsu Hospital Trust. All patients provided informed written consent.
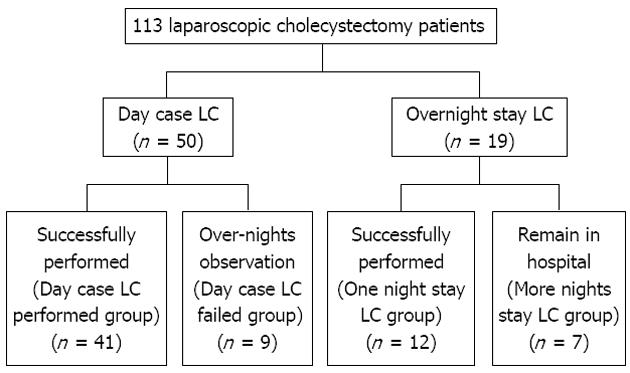
We have performed day case or overnight stay LC since 2001. From July 1, 2009, we have innovated a new technique of transversus abdominis plane block (TAP block)[10], a local anesthetic procedure, to decrease postoperative pain. Therefore, in this retrospective study, we reviewed the patients who underwent day case or overnight stay LC from July 1, 2009 to April 30, 2011. LC was performed on 113 patients at our hospital in this period. Of 113 patients, 69 underwent a day case or overnight stay LC, according to the following exclusion criteria (Figure 1). The other patients underwent LC as an inpatient procedure.
The requisite indication for day case or overnight stay LC was chronic symptomatic calculous gallbladder disease. The absolute contraindications to exclude day case or overnight stay LC were: (1) acute cholecystitis; (2) American Society of Anesthesiologists (ASA) grade > II ; (3) previous upper abdominal surgery; (4) living alone; and (5) living further than 3 h by car from our hospital. Sixty-nine patients decided of their own free will to undergo either day case or overnight stay LC.
Preoperative diagnostic examinations included routine blood tests, liver function tests, ultrasonic scan and computed tomography of the liver and the bile ducts, and drip infusion cholangiography using computed tomography (DIC-CT) or magnetic resonance cholangiography (MRC) to detect choledocholithiasis. An endoscopic retrograde cholangiography was performed prior to the surgery to remove choledochus calculi in patients diagnosed by DIC-CT or MRC.
The LC surgeries were performed first on a morning theatre list to ensure proper postoperative recovery prior to discharge. All patients underwent LC using a standard four ports (5 mm ports) technique. CO2 pneumoperitoneum was established with a maximum pressure of 12 mmHg and the camera was placed in the umbilical area. The trocar site to raise the bottom of the gallbladder was under the right costal arch in the midclavicular line. The left-hand port site was used to bring the portal triad into view, while the port under the xyphoid process, 2 cm under the midline, was used for dissecting Calot’s triangle. An ordinary electrosurgical device was used for the dissection. The umbilical port was opened under direct incision to remove the nylon bag which contained the resected gallbladder. Intraoperative cholangiography was not performed in any case because choledochus calculi were removed prior to LC.
As far as anesthesia is concerned, general anesthesia was adapted to suit the cardiovascular circumstance of each patient and a subcostal TAP block was performed using 25 mL of 0.5% ropivacaine in both sides of the abdomen immediately after induction of general anesthesia. This subcostal TAP block was performed under ultrasound by identifying the transversus abdominis plane between internal oblique muscle layer and transversus abdominis muscle layer in the abdominal wall[10].
The postoperative pain control regime consisted of 4 mg of lornoxicam 3 times a day as a regular prescription for the first 3 d and then on an as required basis, together with 50 mg of diclofenac sodium suppository as a one shot medicine.
The patients were divided into two groups, the day case LC group and overnight stay LC group in the first place. Then, each group was divided into two groups by whether it was successfully performed or not. The day case LC group was divided into day case LC performed group and day case LC failed group, and the overnight stay LC group was divided into one night stay LC group and more nights stay LC group (Figure 1).
Data included patient characteristics, operation time, blood loss during LC and frequency and reasons for unexpected or prolonged hospital stay in each group.
All values were given as mean ± SD. Student’s t test and χ2 test were used to compare the two groups. P < 0.05 was considered statistically significant.
None of the patients required conversion to open cholecystectomy. There was no hospital mortality and no patient was readmitted with serious morbidity after discharge. Fifty of 69 patients were operated on as a day case LC. Their mean age was 53.6 ± 14.5 years with a range of 28-78 and there were 24 males and 26 females. Their mean operation time was 108.4 ± 41.7 min and mean blood loss during the operation was 6.6 ± 22.4 mL. Another 19 patients were operated on as an overnight stay LC. Their mean age was 62.7 ± 13.9 years with a range of 37-80 and there were 9 males and 10 females. Their mean operation time was 107.4 ± 39.3 min and mean blood loss during the operation was 12.8 ± 20.5 mL. There were no significant differences in gender, operation time and blood loss during the operation but age (P < 0.02) between the day case and overnight stay LC group (Figure 1 and Table 1) was statistically significant.
| Day case LC group (n = 50) | Overnight stay LC group (n = 19) | P value | Day case LC performed group (n = 41) | Day case LC failed group (n = 9) | P value | One night stay LC group (n =12) | More nights stay LC group (n = 7) | P value | |
| Age (yr) | 53.6 ± 14.5 | 62.7 ± 13.9 | < 0.02 | 53.5 ± 14.9 | 54.3 ± 13.7 | NS | 57.9 ± 12.8 | 70.9 ± 12.8 | < 0.05 |
| Gender | |||||||||
| Male | 24 | 9 | NS | 20 | 4 | NS | 5 | 4 | NS |
| Female | 26 | 10 | 21 | 5 | 7 | 3 | |||
| Operation time (min) | 108.4 ± 41.7 | 107.4 ± 39.3 | NS | 106.4 ± 40.7 | 117.7 ± 47.7 | NS | 100.3 ± 42.9 | 119.4 ± 31.5 | NS |
| Blood loss during the operation (mL) | 6.6 ± 22.4 | 12.8 ± 20.5 | NS | 7.6 ± 24.6 | 2.0 ± 2.4 | NS | 10.9 ± 22.5 | 16.1 ± 17.6 | NS |
In 50 patients of the day case LC group, 41 patients were discharged on the same day within 8 h after assessment by the operating surgeon, based on a modified post-anesthesia discharge scoring system (MPADSS)[11]. Their mean age was 53.5 ± 14.9 years with a range of 28-78 and there were 20 males and 21 females. Their mean operation time was 106.4 ± 40.7 min and mean blood loss during the operation was 7.6 ± 24.6 mL. Another 9 patients needed to be admitted to hospital for 2.1 ± 2.0 nights. The reasons for 4 one night admissions were nausea and vomiting, those for another 3 for 4 and 5 nights admission were the requirement of clinical observation following drain insertion due to bile spill, and those for the other 2 were at the patient’s request. The term “patient’s request” means hospitalization regardless of approval for discharge by the operative surgeon according to MPADSS (Table 2). Their mean age was 54.3 ± 13.7 years with a range of 31-74 and there were 4 males and 5 females. Their mean operation time was 117.7 ± 47.7 min and mean blood loss during the operation was 2.0 ± 2.4 mL. There were no significant differences between the day case LC performed group (41 patients) and the day case LC failed group (9 patients) (Table 1).
| Day case LC group | Overnight stay LC group | |
| Nausea and vomiting | 4 | 1 |
| Necessity of clinical observation following drain insertion | 3 | 1 |
| Patient's request | 2 | 5 |
In 19 patients of the overnight stay LC group, 12 patients were discharged on the next day after the operation. Their mean age was 57.9 ± 12.8 years with a range of 37-76 and there were 5 males and 7 females. Their mean operation time was 100.3 ± 42.9 min and mean blood loss during the operation was 10.9 ± 22.5 mL. Another 7 patients had to remain in hospital for 3.1 ± 2.1 nights. The reasons for 5 for 2 nights admission were patient’s request, that for another 1 for 4 nights admission was nausea and vomiting, and that for the other 1 for 8 nights admission was requirement of clinical observation following drain insertion due to bile spill (Table 2). Their mean age was 70.9 ± 12.8 years with a range of 56-80 and there were 4 males and 3 females. Their mean operation time was 119.4 ± 31.5 min and mean blood loss during the operation was 16.1 ± 17.6 mL. There were no significant differences in gender, operation time and blood loss but age (P < 0.05) between the one night stay LC group (12 patients) and the more nights stay LC group (7 patients) was significant (Table 1).
When the day case LC performed group and the one night stay LC group were compared, there were no significant differences between the groups.
The proportion of patients requiring unexpected or prolonged hospital stay was 7 out of 50 (14.0%) in the day case LC group compared with 2 of 19 (10.5%) in the overnight stay LC group when patient’s request was excluded; thus 86.0% of patients in the day case LC group and 89.5% in the overnight stay LC group were discharged on the day of surgery or on the following day according to the schedule, respectively. There were no significant differences between the groups.
Although day case LC can save costs[3,9], concerns remain about patient safety. The morbidity of LC has been reported to be 4%-20%[12]. It is reported that about 50% of all complications during LC occur at the set-up of the pneumoperitoneum[13]. Typical mishaps at the set-up period are bleeding from trocar sites and vascular injury[13]. Other complications include bleeding from the liver bed, spillage of gallstones or bile, bowel injuries and so on.
It has been recommended that patients should be observed for at least 24 h so that an intervention can be performed quickly if major complications such as bleeding or bile duct injury occur[14]. The incidence of major complications is substantially low. Arterial bleeding or hemorrhage generally becomes symptomatic during operation or within a few hours after surgery. On the other hand, bile duct injury becomes symptomatic during operation or several days after surgery.
In the present study, patients who underwent day case LC were observed for approximately 8 h after surgery. They had to meet MPADSS[11] before discharge was allowed. No difference in the number of postsurgical complications was found between the day case LC group and the overnight stay LC group and none of complications manifested during the hospital stay. These results imply that the hospital stay did not reduce the detection and subsequent consequences of complications. Therefore, 8 h of observation after LC appears to be sufficient. Several studies have also demonstrated the safety of LC with discharge on the same day[15].
In the present study, the vast majority of patients in both the day case LC group and the overnight stay LC group were successfully discharged and the proportion of people with unexpected or prolonged hospital stay was similar in both groups when patient’s request was excluded. In addition, the duration of any unexpected or prolonged hospitalization was similar between the groups, suggesting that the severity of the causative condition was neither increased nor reduced by an overnight stay. These results demonstrate that in patients with an overnight stay, there are many patients who can have a day case LC safely.
It is important to identify risk factors for admission preoperatively to avoid the disappointment and disruption of an unexpected admission. The present study demonstrated that LC can be performed in selected patients as a day case procedure without jeopardizing the safety of the patients. The absence of readmission indicates that the criteria in this study are appropriate and strict. A previous diagnosis of acute cholecystitis or biliary pancreatitis was reported to be a highly predictive factor of hospital admission and patients with ASA grade of more than II were more likely to require a postoperative stay of over 12 h[16].
The only difference between the day case and overnight LC group was age. Age was also the only difference between the one night stay and more nights stay group. The mean age was gradually higher from day case to more nights stay as hospital stay became longer. This result demonstrates that elderly patients show a tendency to like to stay in hospital rather than be a day case. This is unique in Japan and has not been reported from any other countries. Maggiore[7] reported that being 75 or older is a relative contraindication that led to exclusion in his criteria of patient selection. Some selection criteria for day case LC excludes patients older than 70 years[17,18]. Of course, these exclusion criteria are derived from the fact that elderly patients have a high risk of postoperative complications. Not only so, elderly patients in Japan are likely to stay hospital longer after LC probably because the hospital cost is relatively lower in Japan and their anxiety due to fear of suffering complications and pain at home is strong. Therefore, we must take special care to give elderly patients adequate information before surgery and a support system after discharge.
Adequate pain relief is essential in day case surgery. Various methods, such as peritoneal instillation of local anesthetic agents[19,20] and wound infiltration with local anesthetic agents[21], have been attempted to decrease postoperative pain. But Hilvering et al[22] reported the opposite result, that combined subcutaneous and intraperitoneal administration of levobupivacaine did not influence postoperative abdominal pain after LC. We innovated the TAP block as a postoperative pain block[10] and after that no patients complained of postoperative pain.
Postoperative nausea and vomiting are other factors that may influence postoperative discharge and hospital stay[23]. In this study, the most common reasons for unexpected or prolonged hospital stay were nausea and vomiting. Nearly half of unexpected or prolonged hospital stay patients in both day case and overnight LC groups were due to nausea and vomiting. Hereafter, an effective protocol for control of nausea and vomiting is an essential component in the day case LC service. The routine use of prophylactic anti-emetic agents such as ondansetron[5] and preemptive analgesia with non-steroidal anti-inflammatory drugs[24] may reduce the incidence of postoperative nausea and vomiting.
Laparoscopic cholecystectomy (LC) is a popular procedure in Japan. This surgery has been performed as an inpatient surgery, while it has been done regularly as ambulatory surgery in patients with uncomplicated gallstone disease in the United States and parts of Europe. On the other hand, ambulatory LC is performed in one hospital by day case, while in another hospital by overnight stay.
In this study, the authors attempted to evaluate the applicability and safety of the ambulatory LC and to compare day case and overnight stay LC.
In this study, the authors demonstrate that day case LC can be performed safely with a low rate of complications and no readmissions and that most of the patients with an overnight stay LC can be performed safely as a day case. They also indicate the application and discharge criteria for ambulatory LC.
This study may represent a future strategy for LC as a day case procedure.
The authors studied the applicability and safety of the ambulatory LC and the comparison between a day case and overnight stay procedure. It revealed that ambulatory LC can be performed as a day case procedure, according to the criteria as described in this manuscript, and that elderly patients need special care to reduce their anxiety due to the fear of suffering complications and pain after discharge. The results are interesting and may represent a future strategy for LC as a day case procedure.
Peer reviewer: Zenichi Morise, MD, PhD, Department of Surgery, Fujita Health University School of Medicine, 1-98 Dengakugakubo Kutsukakecho, Toyoake, Aichi 470-1192, Japan
S- Editor Wen LL L- Editor Roemmele A E- Editor Xiong L
| 1. | Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new 'gold standard'? Arch Surg. 1992;127:917-21; discussion 921-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 298] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | Leeder PC, Matthews T, Krzeminska K, Dehn TC. Routine day-case laparoscopic cholecystectomy. Br J Surg. 2004;91:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Jain PK, Hayden JD, Sedman PC, Royston CM, O'Boyle CJ. A prospective study of ambulatory laparoscopic cholecystectomy: training economic, and patient benefits. Surg Endosc. 2005;19:1082-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Tenconi SM, Boni L, Colombo EM, Dionigi G, Rovera F, Cassinotti E. Laparoscopic cholecystectomy as day-surgery procedure: current indications and patients' selection. Int J Surg. 2008;6 Suppl 1:S86-S88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Briggs CD, Irving GB, Mann CD, Cresswell A, Englert L, Peterson M, Cameron IC. Introduction of a day-case laparoscopic cholecystectomy service in the UK: a critical analysis of factors influencing same-day discharge and contact with primary care providers. Ann R Coll Surg Engl. 2009;91:583-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Calland JF, Tanaka K, Foley E, Bovbjerg VE, Markey DW, Blome S, Minasi JS, Hanks JB, Moore MM, Young JS. Outpatient laparoscopic cholecystectomy: patient outcomes after implementation of a clinical pathway. Ann Surg. 2001;233:704-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 106] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Kow AW, Tan A, Chan SP, Lee SF, Chan CY, Liau KH, Ho CK. An audit of ambulatory laparoscopic cholecystectomy in a Singapore institution: are we ready for day-case laparoscopic cholecystectomy? HPB (Oxford). 2008;10:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Victorzon M, Tolonen P, Vuorialho T. Day-case laparoscopic cholecystectomy: treatment of choice for selected patients? Surg Endosc. 2007;21:70-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 518] [Cited by in RCA: 493] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 11. | Chung F. Are discharge criteria changing? J Clin Anesth. 1993;5:64S-68S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 81] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Keulemans Y, Eshuis J, de Haes H, de Wit LT, Gouma DJ. Laparoscopic cholecystectomy: day-care versus clinical observation. Ann Surg. 1998;228:734-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 107] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Shamiyeh A, Wayand W. Laparoscopic cholecystectomy: early and late complications and their treatment. Langenbecks Arch Surg. 2004;389:164-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | Modini C, Mingoli A, Castaldo P, Sgarzini G, Marzano M, Nardacchione F. Aortic laceration during laparoscopic cholecystectomy that required delayed emergency laparotomy. Eur J Surg. 1996;162:739-741. [PubMed] |
| 15. | Gurusamy K, Junnarkar S, Farouk M, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of day-case laparoscopic cholecystectomy. Br J Surg. 2008;95:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Simpson JP, Savarise MT, Moore J. Outpatient laparoscopic cholecystectomy: what predicts the need for admission? Am Surg. 1999;65:525-58; discussion 529. [PubMed] |
| 17. | Johansson M, Thune A, Nelvin L, Lundell L. Randomized clinical trial of day-care versus overnight-stay laparoscopic cholecystectomy. Br J Surg. 2006;93:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Fassiadis N, Pepas L, Grandy-Smith S, Paix A, El-Hasani S. Outcome and patient acceptance of outpatient laparoscopic cholecystectomy. JSLS. 2004;8:251-253. [PubMed] |
| 19. | Tsimoyiannis EC, Glantzounis G, Lekkas ET, Siakas P, Jabarin M, Tzourou H. Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1998;8:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Boddy AP, Mehta S, Rhodes M. The effect of intraperitoneal local anesthesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Anesth Analg. 2006;103:682-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Lepner U, Goroshina J, Samarütel J. Postoperative pain relief after laparoscopic cholecystectomy: a randomised prospective double-blind clinical trial. Scand J Surg. 2003;92:121-124. [PubMed] |
| 22. | Hilvering B, Draaisma WA, van der Bilt JD, Valk RM, Kofman KE, Consten EC. Randomized clinical trial of combined preincisional infiltration and intraperitoneal instillation of levobupivacaine for postoperative pain after laparoscopic cholecystectomy. Br J Surg. 2011;98:784-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Hollington P, Toogood GJ, Padbury RT. A prospective randomized trial of day-stay only versus overnight-stay laparoscopic cholecystectomy. Aust N Z J Surg. 1999;69:841-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87:62-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 441] [Article Influence: 18.4] [Reference Citation Analysis (0)] |